|
|
 |
 |
 |
 |
|
|
The best of the best: a review of select glaucoma case reports published in 2014
Digital Journal of Ophthalmology 2015
Volume 21, Number 4
October 18, 2015
DOI: 10.5693/djo.01.2015.08.001
|
Printer Friendly
Download PDF |
|
|


 Ambika Hoguet, MD,
Ambika Hoguet, MD, | Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, Massachusetts Louis R. Pasquale, MD | Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, Massachusetts Channing Division of Network Medicine, Brigham and Women’s Hospital, Boston, Massachusetts
|
|
|
| Abstract | | This review article summarizes four key case reports published in the field of glaucoma in the year 2014. The first article describes successful early drainage of delayed suprachoroidal hemorrhage in 7 patients who underwent glaucoma surgery. The second describes the use of a corneal patch graft to repair leaking or hypotonous blebs in patients who underwent glaucoma filtration surgery. The third article describes methods to reduce complications when implanting posterior chamber phakic intraocular lenses. The last article describes the clinical course and treatment of a patient in whom oseltamivir use resulted in bilateral acute angle closure. | | | Body | Introduction
The field of glaucoma is changing rapidly as our understanding of the disease evolves; novel treatment options are being developed, and technology improves. Reviewing case reports is an indispensible way to advance our knowledge of glaucoma using the "N = 1" approach. A well-written case report can provide information about the unique presentation of a disease, novel therapeutic approaches, innovative surgical techniques, and uncommon but important outcomes of medical and surgical interventions.
As a reflection of our growing fund of knowledge, in the year 2014 alone, 84 case reports in the field of glaucoma were published in the English language (as indexed in MEDLINE). To assess which articles have the greatest potential for impacting current practice, we assessed each publication with respect to the following parameters: (1) contribution to improving patient care, (2) unique clinical case or management technique, (3) comprehensive description of the clinical or surgical scenario, and (4) use of clinically relevant images when indicated. Here, we summarize (in no particular order) what we consider to be the most clinically relevant publications of the year. Although there were several excellent candidates, we chose 4 based on the above criteria. These cases provide new insights into the surgical management of difficult glaucoma problems and provide information about a new scenario, where we may encounter drug-induced bilateral secondary angle closure glaucoma.
An alternative approach for management of delayed suprachoroidal hemorrhage after glaucoma procedures
In this interventional case series by Pakravan and colleagues,(1) 7 eyes of 7 patients who developed a delayed suprachoroidal hemorrhage (DSCH) following glaucoma surgery were treated surgically within 36 hours of diagnosis rather than after the recommended 7-14 days. All of these cases had pain, profound vision loss, and elevated intraocular pressure (IOP). This is important because sometimes DSCH can be limited and only produce mild signs and symptoms—in such cases it may be reasonable to observe. The choroidal tap and anterior chamber reformation was performed in a similar fashion for all patients (Figure 1). The authors highlight the details of 2 clinical cases for which they performed this surgery and provide results for all 7 patients in whom this intervention was performed. All 7 eyes had improvement in visual acuity and IOP postoperatively, and no complications were reported related to the procedure (range of follow-up, 6-40 months). Intraoperatively, not much egress of blood was noted in most cases; however, slow evacuation of blood continued through the sclerotomy sites in the postoperative period. The surgery can be performed by an anterior segment surgeon and can result in rapid relief of pain.
DSCH is a known complication of both trabeculectomy and glaucoma drainage implant surgery, occurring in 1.5% to 7.1% cases.(2) Traditionally, most specialists recommend waiting 7-14 days before draining a DSCH to allow time for liquefaction of blood; however, this approach has the potential to increase exposure to intractable elevated IOP, enhance intraocular inflammation, and predispose to retinal complications. In this case series, the authors noted that blood continued to liquefy and egress through the sclerotomy sites slowly following immediate drainage; they suggest that immediate drainage can lead to favorable outcomes. As DSCH is a relatively rare event, increased reporting of outcomes in patients who undergo surgical drainage (both early, as in this report, or late) will be helpful in understanding how to optimize management of this surgical complication.
Corneal patch graft for the repair of late-onset hypotony or filtering bleb leak after trabeculectomy: a new surgical technique
Some patients with intractable hypotony are found to have devitalized sclera upon surgical repair, and this problem cannot be fixed with conjunctiva or even an overlay of scleral reinforcing material. Here, Bochmann and colleagues(3) describe a novel approach for treating bleb-related complications due to defects of deep scleral tissue in 5 patients who previously underwent trabeculectomy with mitomycin C. Four patients had failed a previous conjunctival repair procedure. The surgical technique allowed the repair of thin (or absent) scleral tissue that was too weak be sutured in a manner that would allow adequate outflow resistance. To do this, the authors used the remaining anterior lamella of a donor cornea that was used previously for Descemet stripping automated endothelial keratoplasty (Figure 2). The postoperative care included the use of additional glaucoma medications and laser suture lysis. Four patients had resolution of their leak and normalization of their IOP (all patients needed supplemental glaucoma drops), and 1 patient had a resolution of bleb leak but went on to require the implantation of a glaucoma drainage device at 5 weeks.
Bleb leaks are an unfortunate consequence of trabeculectomy surgery (wound leaks occurred within 1 month of surgery in 11% of patients and after 1 month in 6% of patients enrolled in the tube vs trabeculectomy study)(4) and are even more common with the widespread use of antifibrotic agents such as mitomycin C.(5) Often, the resulting thin-walled, avascular blebs with weakened underlying scleral tissue can be difficult to treat. Glaucoma surgeons can add this technique to their armamentarium for certain patients who develop late-onset hypotony of bleb leaks.
Pseudophacomorphic glaucoma along with pupillary block after VisianTM Implantable collamer lens implantation for high myopia.
To date, over 400,000 Visian implantable collamer lenses (STAAR surgical, Monrovia, CA) have been used to correct refractive error.(6) With careful patient selection and judicious surgical technique, the procedure is considered relatively safe.(7) However, devastating complications, including pupillary block glaucoma, can occur. McCaughey and colleagues present the case of a 44-year-old highly myopic woman who underwent bilateral implantation of a Visian implantable collamer lens (ICL) and suffered consecutive iatrogenic pupillary block.(8) Preoperatively, a single laser peripheral iridectomy was performed in each eye. Three hours postoperatively, the patient was in pupillary block in her right eye, likely due to use of an oversized ICL. On postoperative day 1 she was found to have corneal edema, with synechiae to the ICL. She underwent surgical synechiolysis with iris and lens repositioning (Figure 3; taken approximately 4 months postoperatively). Two weeks later, she developed pupillary block in her left eye due to a nonpatent iridotomy and underwent unsuccessful laser followed by successful surgical peripheral iridectomy (Figure 4; taken approximately 4 months postoperatively).
The Visian ICL is a posterior chamber phakic intraocular lens whose plate haptics are supported by the ciliary sulcus, creating an anterior vault that can place patients at an increased risk for pupillary block. Experts recommend the placement of two patent peripheral iridectomies (separated by approximately 80°-90°) and adequate biometric measures to ensure appropriate lens sizing to prevent these complications. With placement of only a single iridotomy, rotation or decentration of the lens can potentially cause blockage of the iridectomy by a haptic. In addition, a postoperative inflammatory response can lead to a nonfunctional laser iridotomy, which is not typical when laser is used to prevent or break pupillary block glaucoma. If an ICL is oversized, the lens vault can push the iris forward and cause direct compression of the trabecular meshwork; permanent resolution requires explantation of the ICL. This case highlights the importance of preoperative planning in these patients and reminds us of the need to tailor treatment to the specific cause of postoperative angle closure. In these patients, it is important to first confirm the patency of the peripheral iridotomy. If it is patent, then one has to consider the lens vault is blocking aqueous outflow.
Oseltamivir (Tamiflu)-induced bilateral acute angle closure glaucoma and transient myopia.
Lee and colleagues present the case of a 27-year-old emmetropic, previously healthy woman who developed bilateral, acute, angle closure 4 days after beginning oral oseltamivir (75 mg twice daily) to treat the flu.(9) This case is particularly interesting because of the relatively low effectiveness (23%) of the influenza vaccine during the 2014-15 flu season.(10) The patient developed a bilateral myopic shift (right eye, spherical equivalent 4.5 D; left eye, 4 D) accompanied by an IOP as high as 60 mm Hg, in both eyes. Ultrasound biomicroscopy on presentation revealed 360-degree ciliochoroidal effusions, anterior rotation of the ciliary processes, and forward displacement of the lens-iris diaphragm in both eyes. Oseltamivir-induced secondary angle closure was suspected, and the patient was started on topical cycloplegic agents and topical prednisolone. Oral oseltamivir was discontinued. Three days later, her myopic shift was nearly resolved and examination revealed deepening of her anterior chamber. Ultrasound biomicroscopy showed resolution of ciliochoroidal effusions in both eyes. Topical anti-inflammatories, glaucoma medications, and cycloplegia were discontinued at that time. She remained asymptomatic for a 2-week follow-up period.
Several drugs, including dopaminergic agents such as carbegoline, are associated with the development of ciliochoroidal effusions leading to bilateral acute angle closure.(11) In this case, the authors suspect that oseltamivir may have produced elevated serum dopamine levels, leading to an alteration in membrane potential and creation of ciliochoroidal effusions.(12) Oseltamivir joins a growing list of compounds associated with bilateral secondary angle-closure glaucoma that do not contain sulfonamide moieties.13 It should be noted that, to our knowledge, influenza infection has not been previously associated with secondary angle-closure glaucoma. Physicians should keep this association in mind during future flu seasons as the report herein is fairly convincing. | |

Figure 1
Schematic diagram of choroidal tap from Pakravan and colleagues.(1) A clear corneal traction suture is used to gain exposure to the ocular surface 4 mm posterior to the limbus. A cut down to bare choroid is made, exposing the suprachoroidal space. This is followed by a sclerectomy (not shown) to facilitate drainage of blood postoperatively. Copyright 2012 by Lippincott Williams & Wilkins. Reprinted with permission.
|
|

Figure 2
Surgical repair of a weakened scleral trabeculectomy flap using a corneal patch graft. The corneal patch graft is sutured to the scleral tissue bed. Bochmann and colleagues.(3) Copyright 2013 Lippincott Williams & Wilkins. Reprinted with permission.
|
|
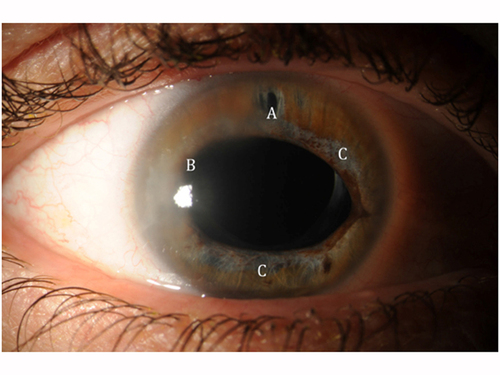
Figure 3
Slit-lamp photograph of the right eye taken after ICL repositioning showing a patent peripheral iridotomy (A), temporal corneal edema (B), traumatic mydriasis, and iris atrophy (C). McCaughey and colleagues.(8) Reprinted with permission.
|
|
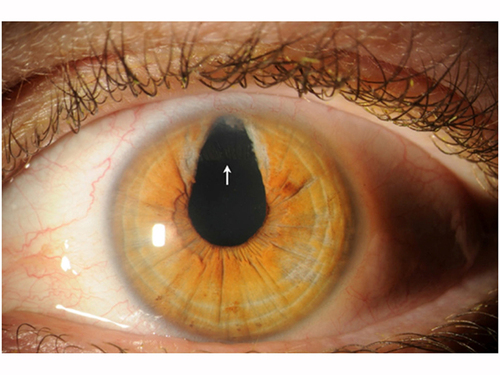
Figure 4
Slit-lamp photograph of the left eye showing a large sectoral surgical iridectomy exposing the edge of the Visian ICL (white arrow). McCaughey and colleagues.(8) Reprinted with permission.
|
|
| Summary | • Early treatment should be considered in patients who, following glaucoma surgery, develop a delayed suprachoroidal hemorrhage associated with pain, vision loss, and elevated intraocular pressure.
• Donor cornea can be used to repair a filtering bleb leak or late onset hypotony in patients with thin or absent scleral tissue at the trabeculectomy site.
• Implantation of posterior chamber phakic intraocular lenses mandates the placement of 2 patent peripheral iridotomies and adequate lens sizing to prevent postoperative complications including pupillary block.
• Oseltamivir should be considered among the growing list of compounds associated with bilateral secondary angle-closure glaucoma. | | | References | 1. Pakravan M, Yandazi S, Adroozifar M, Kouhestani N, Ghassami M, Shahshahan M. An alternative approach for management of delayed suprachoroidal hemorrhage after glaucoma procedures. J Glaucoma 2014;23:37-40.
2. Tuli SS, WuDunnD, Ciulla TA, Cantor LB. Delayed suprachoroidal hemorrhage after glaucoma filtration procedures. Ophthalmol 2001;108:1808-11.
3. Bochmann F, Kaufmann C, Kipfer A, Thiel MA. Corneal patch graft for the repair of late-onset hypotony or filtering bleb leak after trabeculectomy: a new surgical technique. J Glaucoma 2014; 23:e76-e80.
4. Gedde SJ, Herndon LW, Brandt JD, et al. Postoperative complications in the Tube Versus Trabeculectomy (TVT) study during five years of follow-up. Am J Ophthalmol. 2012; 153:804-14.
5. DeBry PW, Perkins TW, Heatley P, Kaufman P, Brumback LC. Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin C. Arch Ophthalmol 2002;120:297-300.
6. Star surgical. Visian ICL FAQs. Available at: http://staar.com/products/visian-icl. Accessed January 20, 2015.
7. Igarashi A, Shimizu K, Kamiya K. Eight-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Am J Ophthalmol 2014;157:532-9.
8. McCaughey MV, Mifflin T, Fenzl C, Goldsmith J, Moshirfar M. Pseudophacomorphic glaucoma along with pupillary block after VisianTM implantable collamer lens implantation for high myopia. Open J Ophthalmol 2014;4:107-11.
9. Lee JW, Lee JE, Choi HY, Lee JS. Oseltamivir (Tamiflu)-induced bilateral acute angle closure glaucoma and transient myopia. Indian J Ophthalmol 2014;62:1165-7.
10. Centers for disease control and prevention. Seasonal Influenza Vaccine Effectiveness, 2005-2015. Available at: http://www.cdc.gov/flu/professionals/vaccination/effectiveness-studies.htm. Accessed January 20, 2015.
11. Razmjoo H, Rezaei L, Dehghani A, Peyman A, Akhlaghi M. Bilateral angle-closure glaucoma in a young female receiving cabergoline: a case report. Case Report Ophthalmol 2011;2:30-3.
12. Cooper RL, Constable IJ, Davidson L. Aqueous humor catecholamines. Curr Eye Res 1984;3:809-13.
13. Murphy RM, Bakir B, O’Brien C, Wiggs JL, Pasquale LR. Drug-induced bilateral secondary angle closure glaucoma: a literature synthesis. J Glaucoma; April 21, 2015. Epub ahead of print. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in