|
|
 |
 |
 |
 |
|
|
The current state of retinopathy of prematurity in India, Kenya, Mexico, Nigeria, Philippines, Romania, Thailand, and Venezuela
Digital Journal of Ophthalmology 2019
Volume 25, Number 4
October 12, 2019
DOI: 10.5693/djo.01.2019.08.002
|
Printer Friendly
Download PDF |
|
|



Theodore Bowe, BS | Retina Service, Mass Eye Ear, Harvard Medical School, Boston; Department of Ophthalmology, Boston Children’s Hospital, Harvard Medical School, Boston Lily Nyamai, MD | Department of Ophthalmology, University of Nairobi, College of Health Sciences Dupe Ademola-Popoola, MD | Department of Ophthalmology, University of Ilorin and University of Ilorin Teaching Hospital, Ilorin, Nigeria Atchara Amphornphruet, MD | Department of Ophthalmology, Queen Sirikit National Institute of Child Health, Bangkok, Thailand Rachelle Anzures, MD | Retina Service, St. Lukes Medical Center, Manila, Phillipines Linda A. Cernichiaro-Espinosa, MD | Retina and Vitreous Department, Asociación para Evitar la Ceguera en Mexico, “Hospital Luis Sanchez Bulnes,” IAP, Mexico City, Mexico Roseline Duke, MD | Calabar Childrens Eye Center, Department of Ophthalmology, University of Calabar, Calabar, Nigeria Fahir Duran, MD | Department of Ophthalmology, Hospital Pediatrico Dr. Agustin Zubillaga, Barquisimeto, Venezuela Maria Ana Martinez-Castellanos, MD | Retina Service, St. Luke’s Medical Center, Manila, Phillipines; Retina and Vitreous Department, Asociación para Evitar la Ceguera en Mexico, “Hospital Luis Sanchez Bulnes,” IAP, Mexico City, Mexico Prabhujot Kaur Multani, DNB | Retina Service, L.V. Prasad Eye Institute, Bhubaneswar, India Cristina E. Nitulescu, MD | Marie Sklodowska Curie Children’s Clinical Hospital, Bucharest, Romania Tapas Ranjan Padhi, MS | Retina Service, L.V. Prasad Eye Institute, Bhubaneswar, India Boontip Tipsuriyaporn, MD | Retina Service, Mass Eye Ear, Harvard Medical School, Boston; Department of Ophthalmology, Boston Children’s Hospital, Harvard Medical School, Boston; Department of Ophthalmology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand R.V. Paul Chan, MD, MSc | Department of Ophthalmology, University of Illinois Chicago School of Medicine, Chicago J. Peter Campbell, MD, MPH | Casey Eye Institute, Oregon Health Sciences University, Portland Yoshihiro Yonekawa, MD | Mid Atlantic Retina, Wills Eye Hospital, Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia
|
|
|
| Abstract | | Retinopathy of prematurity (ROP) is one of the leading causes of preventable blindness in children worldwide. Middle-income nations are currently experiencing epidemic levels of ROP, because greater access to neonatal intensive care units has improved survival rates of premature infants, but without sophisticated oxygen regulation. The epidemiology, screening infrastructure, treatment options, and challenges that these countries face are often tied to unique local socioeconomic, cultural, geopolitical, and medical factors. We present an overview and narratives of the current state of ROP in eight countries that are or soon will be experiencing ROP epidemics—India, Kenya, Mexico, Nigeria, Phillipines, Romania, Thailand, and Venezuela—with a view to fostering both an understanding of the differences in the ROP landscape in various settings and an interest in the further development of ROP screening and treatment services tailored to local requirements. | | | Body | Advances in neonatal care have led to a significant reduction in the minimum age of viability for preterm infants. These improvements, ironically, have led to the development of retinopathy of prematurity (ROP),(1) which first emerged in the 1940s in industrialized nations (“first epidemic”). Early research into the risk factors for ROP found an association between oxygen supplementation and the development of ROP.(2-6) Reduction of oxygen subsequently reduced the rates of ROP; however, it soon became evident that with oxygen reduction came increased mortality from pulmonary and neurological complications.(7) Reinstitution of oxygen therapy led to reemergence of ROP. With time, the balance between ROP and oxygen supplementation have become better titrated, first aided by blood gas analysis, and now by pulse oxymetry.
High-income nations are currently undergoing a “second epidemic” of ROP, where infants are even smaller and younger due to further advances in neonatology to allow micropreemies to survive.(8,9) These infants present more commonly with posterior and aggressive forms of ROP.(10,11) However, the highest overall prevalence and incidence of ROP is now in middle-income nations, where the development of neonatal units have resulted in improved survival of preterm infants, but at times without sophisticated titration of oxygen delivery and measurement, especially in rural hospitals.(10,11) The mechanism is similar to the first ROP epidemic in high income nations. The current ROP epidemic in middle-income nations is known as the “third epidemic.”(12) As an extension of this third epidemic, lower-income nations, where neonatal care has improved greatly, are starting to experience a new wave of ROP.
Much of the world is now addressing ROP as a major public health issue, but issues of epidemiology, screening, and management are not only influenced by medical factors but also driven by local socioeconomic, political, and cultural factors. Table 1 presents screening criteria for each nation. Indeed, every locality has unique considerations when addressing the epidemic. We present the perspectives and narratives of ROP experts from eight middle- and lower-income nations from four continents. Our goal is to describe the diverse global ROP situation to foster better understanding of the unique challenges faced and to learn about how local medical systems in varying communities and organizations maximize care.
ROP in India
Tapas Ranjan Padhi and Prabhujot Kaur Multani, Bhubaneswar, India
India has the highest overall number of premature births in the world.(13) Although the infant mortality rate is still relatively high, it is improving regularly. The number of neonatal intensive care units (NICUs) is rapidly increasing, with 700 government special newborn care units across India.(14) India is currently facing an ROP epidemic that has penetrated into peripheral rural districts. The incidence of ROP in different regions across India has been reported to range from 38% to 47%.(15-19) Inconsistencies of neonatal care have led to large variability in ROP incidence and severity within India. Oxygen delivery and monitoring varies greatly among various NICUs. Our institution is a tertiary eye institute providing advanced ROP care to all sections of society regardless of their financial status in Eastern India. Ten years ago, an organized, protocol-based ROP screening network in this region did not exist.
We initiated our program in 2008 and expanded it into a robust network that covers all the NICUs at Bhubaneswar and neighboring special newborn care units (SNCU) in four rural districts. Our protocol for screening was the same as of the National Neonatal Foundation of India (<34 weeks’ gestational age [GA] and/or birth weight [BW] of <1750 g). However, from 2015 onward, we expanded our screening guidelines to GA of <35 weeks and/or BW of <2000 g. In addition, infants of 34-37 weeks’ GA or with BW of 1750-2000 g are screened in the presence of risk factors for ROP.(19) Note that, compared to screening guidelines set in in the United States, ours capture larger and older infants because affected infants in India tend to be older and have larger birth weights.
In the initial years, the screening program was relatively disorganized and documentation was lacking. We depended mainly on referrals initiated by the neighboring NICUs. We faced resistance to systematic screening not only from the parents but also pediatricians, some of whom felt that uncovering higher incidence of ROP in their NICUs would reflect poorly on their neonatal care. Over time, we strengthened our screening program by conducting ROP-awareness talks, especially on World ROP Day and Children’s Day, and medical education programs for pediatricians, and by continuing to send reminders to NICUs, pediatricians, and parents about the importance of screening. Counseling parents about ROP greatly improved compliance with the screening program. Additionally, the Indian ROP (I-ROP) group has worked relentlessly to formulate India-specific screening guidelines, to bring ROP specialists together, and to encourage collaborations between invested nongovernmental organizations (NGOs), the government, neonatologists, and ophthalmologists.
The number of infants screened annually has progressively increased over the years from 137 babies in 2010 to 2,413 in 2018. During this period, the prevalence of any stage of ROP detected has been 38.45% (2,447 of 6,363 infants). ROP regressed spontaneously in 80% of infants with ROP, and 20% required treatment. Of the infants treated with laser photocoagulation, a majority regressed (92%), and the remaining required subsequent pharmacotherapy with intravitreal vascular endothelial growth factor (VEGF) inhibitors and/or vitreoretinal surgeries.
Overall, 1.8% of infants presented to us with stage 4 or 5 ROP, and the numbers have been increasing as we incoporate more rural and newly established NICUs into our network. This reflects the need of increased ROP awareness in these rural areas for stricter adherence to screening guidelines for more timely examinations and referrals. Oxygen delivery, monitoring practices, and care for collateral health problems are still substandard in many of these hospitals.
The government support for ROP was very poor in the initial years. However, there have recently been many ROP initiatives both by the government and NGOs. Locally, we work with the National Programme for Control of Blindness (NPCB) and Rashtriya Bal Swasthya Karyakram (RBSK) in Odisha. Their support includes assisting in referrals, donating indirect ophthalmoscopes, and supporting training programs for ophthalmologists. They plan to purchase fundus cameras in the future. Similar activities are taking place in other states as well. Other NGOs, including Sight Savers, Orbis, and Public Health Foundation of India (PHFI) have been working extensively on ROP. They are focused on building capacity and share our common goal of making districts independent in providing comprehensive ROP care.
ROP in the Philippines
Rachelle Anzures, San Pablo City, Phillipines
The Philippines has been identified as at high risk for ROP blindness because of inadequate neonatal care and screening.(11) National statistics on the incidence of ROP are currently lacking, but prevalence reports from tertiary hospitals have ranged from 14% to 33%.(20-24)
In 2012 the Philippine Academy of Ophthalmology created the Retinopathy of Prematurity Working Group to address the increasing incidence of ROP in the Philippines. The group has actively campaigned to increase ROP awareness among ophthalmologists, neonatologists, pediatricians, obstetricians, nurses, parents, and the community. We believe that the key is to involve actively all stakeholders in the management of ROP.
The demographics of infants with ROP in the Philippines are different than those in industrialized countries. A retrospective, multicenter study by Corpus et al demonstrated that 16% of babies with ROP would be missed if US screening criteria were employed.(24) The proposal to officially modify the screening criteria to GA of <35 weeks and BW of ≤2000 g still awaits approval pending the results of a larger, prospective multicenter study.
In celebration of World Prematurity Day in 2013, the Recommended Philippine Guideline for Screening and Referral of Retinopathy of Prematurity was launched.(25) This policy statement contains screening and referral guidelines, with recommendations for the management of ROP. The document also includes a list of pediatric ophthalmologists and vitreoretinal specialists who perform screenings. A national ROP hotline was also initiated to help refer infants to the nearest available screener.
The drive to boost ROP screening support from ophthalmologists came in the form of ROP lectures and workshops at annual conventions. The aim of these activities is to promote ROP awareness in order to educate and to encourage potential screeners through a review of disease classification, management and proper techniques in screening preterm babies. As of 2016, a total of 163 Filipino ophthalmologists have attended this program.
The participation of pediatricians, neonatologists, and NICU nurses cannot be overemphasized in the campaign to eliminate ROP blindness. For this reason, the inaugural Philippine ROP Symposium was organized in November 2014. The conference featured a mulidisciplinary panel of international experts, and the occasion was well attended by 150 pediatricians and NICU nurses.
The commitment to advance ROP education among ophthalmology residents and general ophthalmologists was carried out further by tele-education via the Web-based ROP Training Module Program.(26) Trainees were given access to a website where tutorials highlight the relevant ROP findings and management; 156 ophthalmology residents and 13 general ophthalmologists have completed the program successfully.
To take a step further in ophthalmologists’ education, a mentoring program for ROP screening is currently being developed. A skilled mentor will be paired with a trainee to improve his or her screening skills and to develop confidence. The ultimate goal is to establish a network of competent ROP screeners in the Philippines.
A resource website is planned where doctors and parents can have access to various education materials and a database of ROP screeners and treaters throughout the Philippines. A national ROP registry is envisioned, which can be used to collate data and monitor the ROP situation in the country. In the future, legislation for mandatory ROP screening of all identified high-risk babies would ensure that infants will be properly screened and treated. There is still extensive work to be done to implement a standardized ROP screening program throughout the country, but we are committed to preventing the most common cause of blindness in the increasing number of premature infants.
ROP in Mexico
Linda A. Cernichiar-Espinosa and Maria Ana Martinez-Castellanos, Toluca, Mexico
Despite the advances in NICUs in our country, timely diagnosis is generally lacking, and ROP treatment is consequently delayed. Disease severity is correlated with access to screening programs and the quality of care in NICUs. In Mexico approximately 24% of childhood blindness occurs as a result of ROP, with large variations by regions.(27,28)
It can be a challenge to acquire accurate healthcare statistics in Mexico. The last relevant reports by the Grupo ROP México are from 2011. At the time, a survey of 79 neonatal units found that only 53% had stablished ROP screening programs, and only 44% were able to offer treatment.(29)
The increasing body of peer-reviewed evidence suggests that there is a tendency for severe ROP to occur in older and heavier babies (>32 weeks’ GA and/or BW of >1251 g) in moderately and poorly developed countries, which is clearly associated with uncontrolled oxygen administration. We have previously reported unique fluorescein angiographic patterns in these babies.(30,31)
In 2016 our study group from the Asociación para Evitar la Ceguera en México, IAP (APEC), a tertiary-care, referal ophthalmological hospital, performed a survey through social media and learned that many NICUs still do not have blenders for oxygen administration.
The economic impact of ROP on our society is high.(27) Our group participated in the development of the the Economic Model of Retinopathy of Prematurity (EcROP), which showed that the cost per neonate treated in Mexico is estimated to be $3,228 USD; parental indirect cost due to estimated lost wages and productivity was $305,584 USD; and a lifetime loss of productivity resulting from a blind individual was $142,172 USD.
Treatment in Mexico varies geographically, by disease severity, and by location of screening and/or treatment (NICU vs referral center). Treatment employed is approximately 20% laser, 20% anti-VEGF, and 60% combined treatment (laser plus anti-VEGF).(29,32) At our center, if type 1 ROP is diagnosed, immediate intravitreal anti-VEGF is injected. After weekly follow-up, if stage 3 and/or plus disease reappears, or there is evidence of worsening vascular tortuosity with any stage of ROP (after previous regression), retreatment with anti-VEGF monotherapy is considered. We only consider laser for cases where follow-up is not feasible or where there is an oxygen-induced retinopathy with persistent large areas of avascular retina. If there is regression of ROP, we observe every 1 to 2 weeks up to week 52 post-gestational age, then monthly until 6 months of age.
At our center, we performed a retrospective study from October 2011 to March 2015 that included 261 patients screened for ROP who matched the inclusion criteria: 83% were diagnosed with ROP in one eye, with 33% of those patients requiring treatment. Of these, 28% were stage 1, 40% were stage 2, 9% were stage 3, 11% were stage 4, and 13% were stage 5. These numbers are much more skewed toward advanced stages of ROP than those seen in the United States, because of the nature of our referral institution and due to the oxygen dysregulation at most NICUs throughout the country. There was at least one comorbidity (eg, ventricular hemorrhage, bronchopulmonary displasia) in 92% of infants diagnosed with ROP. As a result of our study, we recommend increasing the screening criteria in Mexico to incorporate newborns with GA of ≤34 weeks or BW of ≤1750 g regardless of any other diagnosis.(33,34)
ROP in Venezuela
Fahir Duran, Barquisimeto, Venezuela
The National Program for the Prevention of Childhood Blindness due to Retinopathy of Prematurity emerged in Venezuela in 2005 to initiate the formalization of nationwide ROP screening. NGOs provided critical support. Training workshops led by international ROP experts were held in the capital district and Lara State to assist specialists in their surveillance and treatment of ROP. These training programs have since extended to other states. Currently, ROP treatment is carried out in the states of Caracas-Dtto Capital, Maracaibo-Edo Zulia, and Barquisimeto-Edo, with only the latter two having the capability to offer vitrectomy.
The ROP screening criteria adopted in Latin America varies from US guidelines. Data on GA are often unreliable; thus, the criterion of birth weight is more important. A consensus was reached in Venezuela that neonates with BW of <1750 g and/or GA of <35 weeks would be evaluated as well as neonates who according to the neonatologist’s recommendation merit evaluation on the basis of present risk factors, regardless of BW or GA. All at-risk preterm infants who completed their fourth week of life in an NICU or in neonatal care are evaluated at their place of hospitalization.
If they have been discharged prior to ROP evaluation, the mother is informed of the day and time they are scheduled for the examination. The evaluation consists of indirect ophthalmoscopy with 28 D or 30 D lenses. Successive evaluations depend on the ROP stage found in their first examination, and infants are released from the program when peripheral retinal vascularization is documented.
In 2016 in the state of Lara (Barquisimeto), at the University Hospital of Pediatrics “Dr Agustín Zubillaga,” a total of 445 patients from different localities were evaluated. Of the 445, 69 neonates presented with ROP, 35 of whom were treated with laser.
In view of the current socioeconomic and political situations in Venezuela, ROP specialists do not currently have govermental support for the acquisition of new equipment or even for maintenance of existing technologies; thus, we care for our patients with limited resources. Challenges include increasing ROP prevalence, too few specialists, and lack of coverage in all states.
In the pediatric hospital Agustín Zubillaga, there are 25 incubators in the NICU. But all of incubators are not always functional, and vitreoretinal surgery cannot be performed. Only stage 5 surgeries are performed in private clinics, such as the Acosta Ortiz clinic, where necessary equipment is available to perform the surgeries. In 2016, 21 babies were operated on for stage 5 ROP at the Acosta Ortiz clinic. There were many more patients who could not undergo surgery because of lack of funds.
ROP in Romania
Cristina Nitulescu, Bucharest, Romania
The ROP National Program in Romania was begun in 2002 in Bucharest and expanded to other cities in 2004. There are currently 14 ROP centers, 5 for screening only, 7 equipped for laser therapy, and another 7 equipped for anti-VEGF therapy. Our national criteria are that all babies born with GA of ≤32 weeks and/or BW of ≤1500 g and larger babies with risk factors (hypoxia at birth/mechanical ventilation, oxygen administration without compliance with protocols, neonatal sepsis, blood transfusions, necrotizing enterocolitis, neonatal shock treated with dopamine, intraventricular haemorrhage) must be screened at 4 weeks after birth, but not earlier than 30/31 weeks' postmenstrual age. Laser therapy was initiated in Romania in 2004 and intraocular anti-VEGF was initiated in 2010.
National data is not available, but from our institutional publications the incidence of any ROP in the population that meets our screening criteria can be estimated to be 40%-50%, with treatment-requiring ROP 9%-16%. There is much variation among regions, concordant with a significant discrepancy regarding oxygen administration in NICUs. We know of at least 100 blind or low-vision children born from 2002-2017 whose condition is attributable to missed screenings. From a sample of 3,245 children screened in the country between 2002-2009, 14.5% were treated with laser (the single modality of treatment at that time), 40 children were diagnosed with stage 4B/5 at first examination, and 44 had unfavorable evolution after laser photocoagulation. In a sample of 1,206 children screened in Bucharest between 2010 and 2012, 16.7% had severe ROP with 75% treated with laser, 23% treated with anti-VEGF with or without laser therapy, 3 children screened too late were operated on outside of the country, and 10 children had stage 4/5 in only one eye after treatment. From this sample, 10 children were diagnosed with stage 5 ROP at first eye examination. In a sample of 2,496 babies born between 2013 and 2017 and screened in Bucharest, 9.5% had severe ROP, and all of those treated in time had a favorable result. Of those treated, 56% were treated with laser, 43% with anti-VEGF, 9 children screened too late were referred for surgery outside of the country and 12 children were diagnosed with stage 4/5 ROP at first eye examination.
At the time of this writing, Romania had only 22 ophthalmologists involved in ROP screening, with 12 trained for laser therapy. Many ophthalmologists feel that there is currently too much responsibility and too little compensation in ROP care, which can be time intensive as well. Screening is unfortunately not completed for many children who meet the indications. There is no national pediatric retina surgery unit, and children are referred for surgery in other countries. There is little adherence to oxygen protocols in NICUs and little access to oxygen blenders. Many neonatologists are unaware of the importance of ROP screening, which leads to late or no screening. Finally, there is limited financial support from the national government for ROP screening and treatment.
Strengthening our ROP program is vital, because of the huge costs imposed on the children, their families, and the entire country by this preventable disease. Our most immediate needs include improving education among healthcare providers regarding ROP and the necessity of screening all the infants who meet the criteria. We are currently working with NGOs to develop four ROP Centers of Excellence to take the lead in making national guidelines, reviewing neonatal protocols, providing equipment (including blenders) to NICUs, and training ophthalmologists and neonatologists.
ROP in Nigeria
Roseline Duke and Dupe Ademola-Popoola, Ilorin, Kwara State, Nigeria
ROP is no longer as rare in Nigeria as previously reported, and the survival rate of extremely preterm babies with associated ocular sequelae, resulting in visual impairment and blindness, is increasing.(35) Although there is no national ROP program, a sentinel of routine screening sites exists in fewer than 10 of over 50 total NICU facilities in the country.
Challenges identified with ROP screening and management include insufficient awareness by caregivers on prematurity-related eye problems and weak NICU-driven ROP screening efforts. Additionally, there are too few trained human resources, including ophthalmologists and dedicated ROP coordinators. Infrastructure and technology to bridge the gap in human resources, such as wide-field cameras for screening by midlevel professionals and telemedicine/computerized patient management systems would be beneficial, but they are not currently in use.(35) Mobile phone funduscopy is being used in a several places.(36) When a child needing ROP treatment is identified, the challenge of availability and affordability of timely treatment with laser or anti-VEGF injections becomes daunting, in part because parents must pay for treatment out of pocket.
To address these challenges, some specific efforts have been undertaken. First, international organizations such as the International Pediatric Ophthalmology and Strabismus Council (IPOSC) and the American Association of Pediatric Ophthalmology and Strabismus (AAPOS) are supporting web-based trainings and workshops. Second, disease awareness has been promoted through presentations at clinical meetings and conferences of ophthalmologists, pediatricians, and neonatologists on prematurity-related ocular morbidities and the consequences, including medicolegal issues. We have emphasized the need for a national program on averting ROP blindness and strategies for effective prematurity-related programs at hospital, state, regional, and national levels aimed at strengthening collaboration. Third, social media groups have been formed for ophthalmologists, neonatologists, and others to share experiences and encourage safe NICU practices and screening for ROP in hospitals. We currently have 84 participants in our social media group. Finally, we have fostered the dissemination of information to mothers at immunization points, on radio, and through mass media (funded by the United States Agency for International Development) as well as the publication of educational resources and screening guidelines for ready access in NICUs.
ROP care in Nigeria can be further improved by establishing national safe NICU and ROP guidelines, ensuring functionality of incubators, using oxygen blenders in NICUs, and establishing telemedicine screening programs.
ROP in Kenya
Lily Nyamai, Nairobi, Kenya
Kenya has 188,100 preterms births every year. The hospitals in Kenya are graded from the least advanced, level 1, to the most advanced, level 7. All level 5 hospitals and above have neonatal units run by pediatricians.
Only two public hospitals in Kenya screen and treat ROP, the Kenyatta National Hospital of the University of Nairobi Teaching Hospital, and Moi Teaching and Referral Hospital in Eldoret. The neonatal units that screen for ROP have 80-150 babies admitted in the neonatal unit at any given time. These two public neonatal units each have an 8-10 bed capacity NICU. Each neonatal unit has 15 incubators, shared among neonates.
The challenges the neonatal unit faces is the inadequate number of NICU beds, incubators, and physical space. Oxygen in these units is administered by continuous positive air pressure, mechanical ventilation, oxygen masks, nasal prongs, and monitored by pulse oximetry. The nurse-to-patient ratio is 1:3 in the NICU and 1:8-16 in the rest of the neonatal unit. The neonates are in the care of 2-4 pediatric residents under a neonatologist. As the unit is highly understaffed, mothers play an important role in caring for the babies by observation, providing breast milk, and kangaroo care, but even this resource is under threat, because there is inadequate space to house them.
The screening of ROP in Kenya is fairly recent and began in 2010 as personal initiatives from ophthalmologists and neonatologists after fellowship training in retina, pediatric ophthalmology, and neonatology. Although there are no countrywide guidelines on the screening and treatment of ROP, the Kenyatta National Hospital has written guidelines for management that have been borrowed from other centers. ROP screening therefore varies among hospitals and depends on the knowledge and practice of the staff ophthalmologist or neonatologist. The generally agreed criteria for ROP screening in Kenya are as follows: (1) preterm, with GA of ≤34 weeks; (2) BW of <1750 g; and (3) age up to 36 weeks with unstable clinical course. Photographic documentation of the ROP screening process is ongoing at the Kenyatta National Hospital, although an electronic database for storing patient records has not yet been established.
All ROP centers are in Kenya are located in the capital city. Therefore, incidence data reflects a skewed population. The incidence of ROP ranges from 17% in the public hospitals to 30% in private hospitals.37 About 4% of preterm babies require treatment for ROP. Of these, 75% are treated using laser or anti-VEGF, and the remaining 25% require surgery (unpublished data). Treatment at the public hospital is centered on anti-VEGF injection, with laser provided in private facilities. Vitreoretinal surgery for ROP is only available at two private facilities. Only 9-10 ophthalmologists routinely carry out screening for ROP in three centers in the country. There are only 4 vitreoretinal surgeons who can perform pediatric retina surgery and laser treatment in preterm babies.
Anecdotally, ophthalmologists in Kenya have reported a rise in children presenting to the eye clinics with blindness due to ROP. Although resources are scare, Kenya has an opportunity to build nationwide ROP services, because there are effective programs training both ophthalmologists and pediatricians. Not much government support is available in ROP, however, mainly because disease awareness is lacking and resources are strained. Nevertheless, there is an ongoing study to better determine the incidence of ROP in our population, and the findings will be shared with the relevant authorities to help further development of the services.
ROP in Thailand
Boontip Tipsuriyaporn and Atchara Amphornphruet, Bangkok, Thailand
ROP is a leading cause of childhood blindness in Thailand. Primary drivers of ROP morbidity in our country are increasing preterm delivery rates, a shortage of trained ophthalmologists, and an insufficiency in the availability of ophthalmic and NICU instruments, including lasers and oxygen-monitoring systems.
The national survey of blindness, low vision, and visual impairment in Thailand in 2006-2007 showed that the prevalence of blindness in children aged 14 years and under was 0.11%, and that a staggering 67% of these cases were due to ROP.(38) According to the Ministry of Public Health, among the approximately 800,000 infants that are born each year, 11% are low birthweight and 8%-10% are born preterm.
Queen Sirikit National Institute of Child Health (QSNICH), a large tertiary referral hospital in Bangkok, reported that from 2006 to 2009, 40.7% (655/1609) of preterm infants born there had any stage of ROP. The mean GA of preterm infants with ROP was 29.1 weeks (range, 20-39), and the mean BW was 1254.6 grams (range, 545-2670 g). Prethreshold and threshold disease was found in 59% (n = 387), stage 4 and 5 ROP were found in 6% (n = 37), and aggressive posterior ROP (APROP) was found in 7% (n = 47).
In 2009 the Royal College of Ophthalmologists of Thailand proposed a screening guideline for ROP which recommended screening of all infants with a BW of ≤1500 g, a GA of ≤30 weeks, or, in any preterm infant who has a severe clinical course. An initial examination should be performed at 4-6 weeks chronological age or 31-33 weeks of post-conceptional age.(39) The follow-up period depends on the findings. The implementation of these guidelines is limited by the lack of specialized ophthalmologists in many areas of the country.(40)
Laser treatment–requiring ROP patients are most often referred from rural hospitals, where they do not have the ability to efficiently monitor neonatal oxygen levels. There is little reliable data on incidence of ROP in these areas due to incomplete screening. Telemedical screening for ROP has been shown to be reliable and cost effective; however, it is limited because of the high startup cost and the shortage of trained healthcare workers.(41,42)
Furthermore, the guidelines may not capture all infants requiring treatment. In a QSNICH report from 2010, 11.6% of infants with ROP (94/813) had APROP. Twenty of these 94 APROP cases (21.5%) presented in preterm infants with BW of >1500 g, and over half of the patients in the APROP group had a GA of >30 weeks, which signifies an alarming difference in the ROP risk factors compared to original screening guidelines adapted from the United States. The guidelines must be updated to reflect this finding.
Most of the tertiary ROP referral centers in Thailand can treat ROP with laser and anti-VEGF injections; however, <5% of hospitals can treat with vitreoretinal surgery. Despite the availability of laser photocoagulation, the success rates are not high. Of referred infants (92/400) who had already received laser-treatment and were subsequently referred to QSNICH for follow-up, 23% had further progression of disease to stage 4 or 5. The reported risk factors that were most correlated with ROP progression after laser treatment were inadequate laser, skip areas, and delayed referral (data presented at APAO 2013, Hong Kong).
Plans proposed by the government to reduce the burden of avoidable visual impairment related to ROP mirrors those proposed by other developing nations. These plans center around increasing the supply of trained ophthalmologists, improving access to high-tech neonatology services and medical devices, continuing to investigate the feasibility of telemedical screening programs that could extend the services of our current ophthalmologists, and addressing the differences in the demographics and screening criteria of ROP in Thailand. There is hope that by adopting these efforts, along with continuing to work collaboratively with the international community, we can reduce ROP-associated vision loss in Thailand.
Conclusions
The incidence of ROP is at epidemic proportions in middle-income nations and is increasing in low-income nations. Although high-income countries conduct much of the published research and disseminate many of the screening and treatment guidelines, it is vital to recognize that the frontlines of ROP care internationally differs in varied and crucial ways from the ROP picture in high-income countries. The vast majority of the burden of ROP in the world is being managed in middle- and low-income countries.
We have presented the perspectives from physicians treating ROP in eight countries. Although each country faces unique challenges, certain lessons and themes emerge from the collective experiences. Common challenges include a lack of recognition of the devasting effects of ROP. Governments are often unwilling or unable to fund ROP screening or treatment and are unaware of the consequences of failing to do so. Awareness is often lacking in other physicians as well. Additionally, statistics on incidence and risk factors can be difficult to accurately and reliably obtain. Notably, our contributors from India found a pattern of intentional underreporting of ROP rates by NICU physicians at certain locations. They found it necessary and helpful to emphasize that increased incidence of ROP in a NICU does not reflect poorly on the physician in charge of that NICU. International partnerships and NGOs have been vital to assist with surmounting some of these issues of training, education, and funding.
Additional challenges include large geographical variations in screening and treatment within a country. Telemedical screening programs are being used in many cases in the hope that they can decrease these geographical disparities. However, the cost of treatment can be prohibitively expensive, leading to undertreatment even in the case of timely diagnosis. In the face of these challenges, groups of ophthalmologists have harnessed the potential of the Internet and social media to share tips, tricks, and best practices with each other.
In middle- and low-income countries, ophthalmologists have found that screening criteria for ROP may need to be adjusted to include older and heavier infants to avoid missing patients with ROP requiring treatment. This is posited to be due to the improvement of the capabilities of NICUs in these countries, which have greatly advanced in their ability to preserve life, but frequently lack sophisticated oxygen delivery and monitoring systems. This is leading to demographics similar to those seen during the first epidemic of ROP in the United States and underscores the importance of having context- and country-specific screening criteria. This vital point was underscored by Anzures’ observation that, in a retrospective, multicenter study, 16.2% of infants with ROP in the Philippines would have been missed if US screening criteria had been applied to their population.
In addition, as mentioned in many of the comments from practitioners, in almost all countries, the chronic and consistent lack of oxygen blenders and pulse oximeters in rural NICUs with resultant sustained hyperoxygenation has resulted in the third epidemic of treatment requiring ROP throughout the world. Concomitant comorbidities including bronchopulmonary dysplasia, intraventricular hemorrhages, and necrotizing enterocolitis are also on the rise due partially to increased survival of very preterm infants and partially to hyperoxygenation.(43,44) As demonstrated in the Neonatal Oxygenation Prospective Meta-analysis (NeOProM) Collaboration, adequately controlled saturation parameters can lead to lower rates of ROP and many comorbidities.(45) However, the technologies required to achieve these parameters are relatively costly and not always available.
Treatment can also be challenging, with many geographic areas lacking the capability or resources for laser therapy. Thus even moreso than in affluent nations, interest in and use of anti-VEGF injections has increased. This interest increases the necessity of resolving the lingering concerns about local and systemic effects of anti-VEGF treatment.(46,47) There is a lack of information to guide ophthalmolgists on dosing and implications that use may lead to persistent vascular abnormalities, late recurrence, and progressive atypical tractional retinal detachments.(46,47) The reliance on injection therapy for ROP in middle- and low-income nations only hightens the need for resolution of these knowledge gaps.
Funding/support
Research to Prevent Blindness, New York, NY (RVPC). This project was supported by grants K12EY027720 and P30EY10572 from the National Institutes of Health, Bethesda, MD (JPC); by grants SCH-1622679 from the National Science Foundation, Arlington, VA (JPC); and by unrestricted departmental funding and a Career Development Award from Research to Prevent Blindness, New York, NY (JPC). Funding organizations had no role in the design of conduct of this project.
Disclosures
Consultant for Alcon (RVPC, YY), Allergan (RVPC), Bausch & Lomb Surgical (RVPC), Visunex Medical Systems (RVPC). | |
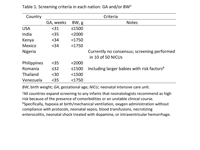
Table 1.
Screening criteria in each nation
|
|
| References | 1. Philip AGS. The evolution of neonatology. Pediatr Res 2005;58:799-815.
2. Michaelson IC. The mode of development of the vascular system of the retina with some observations on its significance for certain retinal disorders. Trans Ophthalmol Soc UK 1948;68:137-80.
3. Ashton N, Ward B, Serpell G. Role of oxygen in the genesis of retrolental fibroplasia: a preliminary report. Br J Ophthalmol 1953;37:513-20.
4. Patz A, Eastham A, Higginbotham DH, Kleh T. Oxygen studies in retrolental fibroplasia. II. The production of the microscopic changes of retrolental fibroplasia in experimental animals. Am J Ophthalmol 1953;36:1511-22.
5. Campbell K. Intensive oxygen therapy as a possible cause of retrolental fibroplasia: a clinical approach. Med J Aust 1951;2:48-50.
6. Patz A, Hoeck LE, De La Cruz E. Studies on the effect of high oxygen administration in retrolental fibroplasia. I. Nursery observations. Am J Ophthalmol 1952;35:1248-53.
7. Bolton DP, Cross KW. Further observations on cost of preventing retrolental fibroplasia. Lancet 1974;303:445-8.
8. Wu C, Löfqvist C, Smith LE, VanderVeen DK, Hellström A; WINROP Consortium. Importance of early postnatal weight gain for normal retinal angiogenesis in very preterm infants: a multicenter study analyzing weight velocity deviations for the prediction of retinopathy of prematurity. Arch Ophthalmol 2012;130:992-9.
9. Lundgren P, Wilde Å, Löfqvist C, Smith LE, Hård AL, Hellström A. Weight at first detection of retinopathy of prematurity predicts disease severity. Br J Ophthalmol 2014;98:1565-9.
10. Gilbert C, Rahi J, Eckstein M, O'Sullivan J, Foster A. Retinopathy of prematurity in middle-income countries. Lancet 1997;350:12-14.
11. Gilbert C. Retinopathy of prematurity: a global perspective of the epidemics, population of babies at risk and implications for control. Early Hum Dev 2008;84:77-82.
12. Quinn GE. Retinopathy of prematurity blindness worldwide: phenotypes in the
third epidemic. Eye Brain. 2016 May 19;8:31-36.
13. Vinekar A, Dogra M, Azad RV, Gilbert C, Gopal L, Trese M. The changing scenario of retinopathy of prematurity in middle and low income countries: unique solutions for unique problems. Indian J Ophthalmol 2019; 67:717-19.
14. Gopal L, Sharma T, Ramchandran S. Retinopathy of prematurity: a study. Indian J Ophthalmol 1995;43:59-61.
15. Charan R, Dogra MR, Gupta A, Narang A. The incidence of retinopathy of prematurity in a neonatal care unit. Indian J Ophthalmol 1995;43:123-6.
16. Rekha S, Battu RR. Retinopathy of prematurity: incidence and risk factors. Indian Pediatr 1996;33:999-1003.
17. Chattopadhyay MP, Pradhan A, Singh R, Datta S. Incidence and risk factors for retinopathy of prematurity in neonates. Indian Pediatr 2015;52:157-8.
18. Pejaver RK, Bilagi AP, Vinekar A. National Neonatology Foundation’s Evidence Based Clinical Practice Guidelines 2010. Retinopathy of Prematurity (NNF India, Guidelines) 2010:253-62.
19. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res 2013;74:35-49.
20. Philippine Pediatric Society. Policy statement on pediatric blindness prevention & vision screening. PPS Policy Statements 2004;1:25-27.
21. Arroyo MH, Camonias DL, Monzon-Pajarillo AK, et al. Criteria for the timing of initial retinal examination to screen for retinopathy of prematurity. Philipp J Ophthalmol 2010;35:15-19.
22. Cerdana HGS, Liao CS, Macias III EL, Nañagas LR. Results of initial screening for retinopathy of prematurity at a tertiary hospital. Philipp J Ophthalmol 2010;35:56-60. Available at https://paojournal.com/article/results-of-initial-screening-for-retinopathy-of-prematurity-at-a-tertiary-hospital/.
23. Ladores CS, Banzon MD. Status of screening for retinopathy of prematurity in a tertiary hospital. Philipp J Ophthalmol 2010;35:61-64.
24. Corpus K, Jimenez IV JM, Anzures R, Bascuna RI, Ventura R, Reandelar M; Retinopathy of Prematurity Working Group. Proposed new retinopathy of prematurity screening criteria: evidence for including older and heavier Filipino premature babies. Philipp J Ophthalmol 2013;38:72-9.
25. Philippine Academy of Ophthalmology, Retinopathy of Prematurity Working Group, Philippine Society of Pediatric Ophthalmology and Strabismus, Vitreoretina Society of the Philippines. Proposed Philippine guidelines for screening and referral of ROP. Philipp J Ophthalmol 2013;38:64-71.
26. American Academy of Ophthalmology. Retinopathy of prematurity: case-based training. 2019. Available at: https://www.aao.org/interactive-tool/retinopathy-of-prematurity-case-based-training.
27. Rothschild MI, Russ R, Brennan KA, et al. The Economic Model of Retinopathy of Prematurity (EcROP) screening and treatment: Mexico and the United States. Am J Ophthalmol 2016;168:110-21.
28. Zepeda Romero LC, Gutiérrez Padilla LA, De la Fuente Torres MA, Angulo Castelanos E, Ramos Padilla E, Quin GE. Detection and treatment for retinopathy of prematurity in Mexico: need for effective programs. J AAPOS 2008:12:225-6.
29. Maynez GO. Screening. In: Grupo ROP México. Retinopatía del premature. Mexican Society of Ophthalmology; 2011:53-59. http://www.ropmexico.org.mx/ingles/archivos/documentos/ROP_Mexico_libro.pdf. Accessed Jan 10, 2018.
30. Martínez-Castellanos MA, Vélez-Montoya R, Price KW, et al. Vascular changes on fluorescein angiography of premature infants with low risk of retinopathy of prematurity after high oxygen exposure. Int J Retin Vitr 2017;3:2.
31. American Academy of Pediatrics. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 2013;131:189-95.
32. Good WV. Early Treatment for Retinopathy of Prematurity Cooperative Group (ETDRS). Final results of the early treatment for retinopathy of prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc 2004;102:233-50.
33. Cernichiaro Espinosa LA, Olguín Manríquez FJ, Henaine Berra A, García Aguirre G, Quiroz-Mercado H, Martínez Castellanos MA. New insights in diagnosis and treatment for Retinopathy of prematurity. Int Ophthalmol 2016; 36:751-60.
34. Meraz-Gutiérrez MP, Olguín Manriquez FJ, Arriola-López AE, et al. Evidence to modify guidelines for routine Retinopathy of prematurity screening to avoid childhood blinfness in middle income countries. Rev Mex Oftalmol 2016;90:167-73.
35. Dupe S. Ademola-Popoola, Oluleye TS. Retinopathy of prematurity in a developing economy with improving health care. Curr Ophthalmol Rep 2017;5:114.
36. Oluleye TS, Rotimi-Samuel A, Adenekan A. Mobile phones for retinopathy of prematurity screening in Lagos, Nigeria, Sub-Saharan Africa. Eur J Ophthalmol 2015;26:92-4.
37. Wanjala I, Ilako D, Kariuki M. Retinopathy of prematurity as seen in two major hospitals in Nairobi, Kenya. East Afr J Ophthalmol 2007;13.
38. Jenchitr W, Hanutsaha P, Iamsirithaworn S. The national survey of blindness low vision and visual impairment in Thailand 2006-2007. Thai J Pub Hlth Ophthalmol 2007;21:11-94.
39. Sakchai Wongsakittirak, Chatuchan Unphureesathien. Screening for abnormal retinal disease in premature infants. Thammasat Ophthalmol J; 255:21-9.
40. Trinavarat A, Atchaneeyasakul L, Udompunturak S. Applicability of American and British criteria for screening of the retinopathy of prematurity in Thailand. Jpn J Ophthalmol 2004;48:50-3.
41. Prakalapakorn SG, Freedman SF, Hutchinson AK, Saehout P, Cetinkaya-Rundel M, Wallace DK, Kulvichit K. Real-world simulation of an alternative retinopathy of prematurity screening system in Thailand: a pilot study. J Pediatr Ophthalmol Strabismus 2018;55:245-53.
42. Wongwai P, Kingkaew P, Asawaphureekorn S. A store-and-forward telemedicine for retinopathy of prematurity screen: is it cost-effective in Thailand? Asian Biomed 2015;9:665-73.
43. Cherian S, Morris I, Evans J, Kotecha S. Oxygen therapy in preterm infants. Paediatr Respir Rev 2014;15:135-41.
44. Siffel C, Kistler KD, Lewis JFM, Sarda SP. Global incidence of bronchopulmonary dysplasia among extremely preterm infants: a systematic literature review. J Matern Fetal Neonatal Med 2019 Aug 9:1-11.
45. Askie LM, Darlow BA, Finer N, et al; Neonatal Oxygenation Prospective Meta-analysis (NeOProM) Collaboration. Association between oxygen saturation targeting and death or disability in extremely preterm infants in the Neonatal Oxygenation Prospective Meta-analysis Collaboration. JAMA 2018;319:2190-2201.
46. Yonekawa Y, Thomas BJ, Thanos A, et al. The cutting edge of retinopathy of prematurity care: expanding the boundaries of diagnosis and treatment. Retina 2017;37:2208-25.
47. Yonekawa Y, Wu WC, Nitulescu CE, et al. Progressive retinal detachment in infants with retinopathy of prematurity treated with intravitreal bevacizumab or ranibizumab. Retina 2018; 38:1079-83.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in