|
|
 |
 |
 |
 |
|
|
The best of the best: a review of select oculoplastic case series published in 2015
Digital Journal of Ophthalmology 2017
Volume 23, Number 4
November 21, 2017
DOI: 10.5693/djo.01.2017.09.001
|
Printer Friendly
Download PDF |
|
|



Jenny Temnogorod, MD | Department of Ophthalmology, SUNY Downstate Medical Center, Brooklyn, New York Roman Shinder, MD, FACS | Department of Ophthalmology, SUNY Downstate Medical Center, Brooklyn, New York
|
|
|
| Abstract | | This review summarizes three case series published in the field of oculoplastic surgery in the year 2015. The first article describes the use of hedgehog pathway inhibitors for medical therapy of advanced periocular basal cell carcinoma and basal cell nevus syndrome. The second describes the use of c-reactive protein as a marker for starting treatment with steroids in children with orbital cellulitis. The third article presents an endoscopic medial orbital fat decompression technique for treatment of proptosis in thyroid eye disease. | | | Body | There have been many advances in diagnosis and treatment oculoplastics. We highlight three especially interesting and relevant case series, all published in 2015, that describe different aspects of oculoplastics practice, including new criteria for treatment as well as medical and surgical therapy.
Hedgehog pathway inhibition for locally advanced periocular basal cell carcinoma and basal cell nevus syndrome
Basal cell carcinoma (BCC) constitutes 90% of eyelid malignancies. The preferred treatment for BCC is local surgical excision, which has a cure rate of 90%-99%.(1) However, certain patients are not good candidates for surgery, including those with multiple lesions, large tumor size, and invasion of tumor into the orbit or the paranasal sinus.(2) Similarly, surgery is not the best option for patients with basal cell nevus syndrome (Gorlin syndrome), who develop numerous microscopic and macroscopic BCC lesions.(3)
Ozgur et al present a retrospective, interventional case series of patients with advanced periocular BCC or basal cell nevus syndrome treated medically with vismodegib (Erivedge; Genentech, South San Francisco, CA; GDC-0449), a selective hedgehog pathway inhibitor.(2) The hedgehog pathway is a common signal transduction pathway during embryogenesis and is also involved in stem cell proliferation in some adult tissues.(4) Genetic mutations in this pathway have been found to contribute to the pathogenesis of BCC and basal cell nevus syndrome.(3,4) Vismodegib binds to and inactivates smoothened (Smo), a receptor in the hedgehog pathway leading to inhibition of downstream signaling and decreased production of proliferation factors (Figure 1).(4)
Ozgur et al describe 12 patients treated with vismodegib: 10 patients with locally advanced BCC for whom surgical excision or radiation would have resulted in significant morbidity or deformity and 2 patients with basal cell nevus syndrome. A complete response occurred in 3 patients, partial response in 6 patients, and stable disease for at least 16 months in 3 patients. Two patients developed progressive disease, one after 16 months of stable disease and the other after 38 months of complete response. Five of the patients without metastases to lymph nodes or other sites were able to avoid orbital exenteration because of this treatment. Long-term follow-up is needed to assess the duration of response in these patients.
Grade I drug-related side effects, not requiring further treatment, were reported by all patients in this series. These included muscle spasms, weight loss, dysgeusia, alopecia, decreased appetite, and fatigue. Five patients also reported grade II side effects, but no patients developed grade III or higher adverse effects, although such side effects have been reported.(5) Grade II side effects are defined as moderate ones, with minimal, local or noninvasive intervention indicated; they may limit age-appropriate daily activities. Grade III side effects are defined as severe or medically significant ones; they may be disabling but not immediately life threatening, and they may require hospitalization. Another consideration that led to discontinuation of therapy by 2 patients in the series is the cost of vismodegib, which is approximately $7,500 per month.(2) Overall, hedgehog pathway–targeted therapy, such as vismodegib, can be considered for a population of patients with locally advanced BCC or basal cell nevus syndrome for whom surgical excision or radiation therapy would result in significant facial deformity or ocular morbidity, including vision loss, or those unable to undergo surgery because of other comorbidities.
C-reactive protein as a marker for initiating steroid treatment in children with orbital cellulitis
Davies et al present a prospective, comparative interventional study using c-reactive protein (CRP) as a marker for starting treatment with steroids in children with orbital cellulitis.(6) Prior to this, only one other prospective study evaluated the use of corticosteroids as an adjunct to antibiotics in the treatment of orbital cellulitis, although pediatric patients were excluded.(7) Pushker et al demonstrated that patients who received steroids after initial clinical improvement on antibiotics recovered more quickly and required less hospitalization.(7) One retrospective study evaluated the use of steroids in children with orbital cellulitis and, although it did not show a statistically significant decrease in hospital stay between the two groups, the authors reported that steroids had no adverse effects on resolution of cellulitis.(8)
Davies et al sought to determine whether addition of steroids would improve the treatment of orbital cellulitis in children and to evaluate CRP as a marker for starting steroids, because previous studies had not recommended guidelines on the timing.(6) They enrolled 31 children: 24 received oral prednisone in addition to intravenous antibiotics, and 7 (the control group) received only antibiotics, per family preference. The dose of prednisone administered was 1mg/kg/day for 7 days. CRP, an acute-phase reactant that is elevated during inflammatory processes and has a relatively short half-life, has been used to monitor patients’ response to therapy.(9) Based on review of previous literature on the use of CRP as a marker, Davies et al decided to start oral steroids for their patients when the CRP level decreased to <4 mg/dl.(6)
The children in the group that received steroids had shorter hospital stays compared to the group that did not, a difference that was statistically significant. Furthermore, the difference was still statistically significant when calculated from the day when CRP decreased to below 4 mg/dl, eliminating lead time bias. No serious side effects of corticosteroids were reported after the 7-day treatment course, but 2 families noted behavioral changes after initiation of steroid treatment that lead to early discontinuation of prednisone in 1 patient. Overall, this study provides evidence for the overall efficacy of treating children with orbital cellulitis using systemic steroids. In addition, it suggests a standardized dosing schedule for oral prednisone and a time to initiate treatment based on CRP level.
Endoscopic medial orbital fat decompression for proptosis in type 1 Graves orbitopathy
In this retrospective, noncomparative, interventional case series, Wu et al present their technique for orbital decompression in patients with proptosis due to thyroid eye disease (TED).(10) They studied 108 Asian patients with inactive disease and significant bilateral proptosis due to orbital fat expansion without marked extraocular muscle enlargement, as noted on preoperative computed tomography scans. The procedure includes endoscopic removal of the medial orbital wall, without disturbing the inferomedial strut, and removal of extraconal and intraconal fat under direct endoscopic visualization with a low-suction device created for this procedure. The trigger on the instrument allows for release of the fat before cutting if blood vessels are visible within the fat globule. The main portion of the fat decompression includes excision of intraconal fat, with minimal amount of extraconal fat removed for exposure. The amount of fat removed was not calculated but judged by the surgeon based on reduction in proptosis.
After an average of 16 months of follow-up, measurements revealed a mean decrease in proptosis of 8.2 mm and symmetry within 2 mm in 98.1% of patients. Previously, it had been suggested that the endoscopic approach alone was most appropriate for patients with optic neuropathy and those with mild proptosis, because of the limited reduction in proptosis.(11) Other authors have stated concerns that orbital fat decompression can result in restrictive strabismus and postoperative diplopia that is difficult to treat.(12) In the current study 25 patients had diplopia within a 30-degree visual field in the immediate postoperative period, but in 23 patients diplopia resolved completely within 3 months. Two patients required strabismus surgery, which was performed successfully in both cases.(10) The authors attribute their relatively low rate of diplopia to several factors, including intact anterior periorbita and inferomedial bony strut, greater removal of intraconal versus extraconal fat and replacement of the periosteal strip over the medial rectus to keep it in a more anatomic position.
Wu et al present a different endoscopic approach to orbital decompression for select patients with TED-related proptosis. Their technique had excellent results in their Asian study cohort; however, results could vary in non-Asian patients. They also present a low-suction cutting device developed for this procedure that proved useful for orbital fat removal.
| |
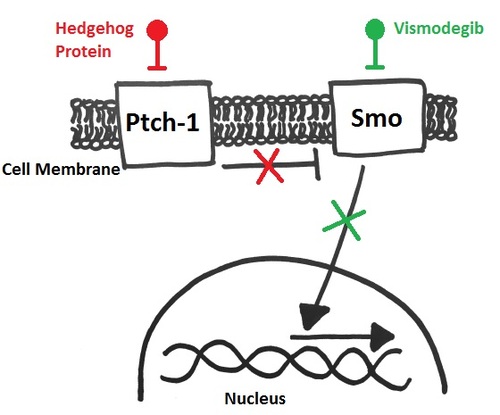
Figure 1
Diagram of the Hedgehog pathway. Patched-1 transmembrane receptor (Ptch-1) is a tumor suppressor that normally inhibits the smoothened receptor (Smo). When a Hedgehog protein binds to Ptch-1, this inhibition stops and Smo is activated, leading to cellular proliferation and tumorigenesis. Vismodegib binds to and inactivates Smo, inhibiting downstream signaling.
|
|
| Summary | • Hedgehog pathway–targeted therapy should be considered for patients with advanced basal cell carcinoma or basal cell nevus syndrome for whom surgery is not the optimal treatment.
• When CRP level is <4 mg/ml, treatment with oral prednisone 1mg/kg/day for 7 days can be started in children with orbital cellulitis to hasten recovery.
• An endoscopic medial orbital fat decompression as described by Wu et al can be used as a sole procedure for treatment of proptosis in select patients with thyroid eye disease.
| | | References | 1. Cook BE Jr, Bartley GB. Epidemiologic characteristics and clinical course of patients with malignant eyelid tumors in an incidence cohort in Olmsted County, Minnesota. Ophthalmology 1999;106:746-50.
2. Ozgur OK, Yin V, Chou E, et al. Hedgehog pathway inhibition for locally advanced periocular basal cell carcinoma and basal cell nevus syndrome. Am J Ophthalmol 2015;160:220-7.
3. Athar M, Li C, Kim AL, Spiegelman VS, Bickers DR. Sonic hedgehog signaling in basal cell nevus syndrome. Cancer Res 2014;74:4967-75.
4. Macha MA, Batra SK, Ganti AK. Profile of vismodegib and its potential in the treatment of advanced basal cell carcinoma. Cancer Manag Res 2013;5:197-203.
5. Von Hoff DD, LoRusso PM, Rudin CM, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med 2009;361:1164-72.
6. Davies BW, Smith JM, Hink EM, Durairaj VD. C-reactive protein as a marker for initiating steroid treatment in children with orbital cellulitis. Ophthal Plast Reconstr Surg 2015;31:364-8.
7. Pushker N, Tejwani LK, Bajaj MS, Khurana S, Velpandian T, Chandra M. Role of oral corticosteroids in orbital cellulitis. Am J Ophthalmol 2013;156:178-83.
8. Yen MT, Yen KG. Effect of corticosteroids in the acute management of pediatric orbital cellulitis with subperiosteal abscess. Ophthal Plast Reconstr Surg 2005;21:363-6.
9. Arnold JC, Cannavino CR, Ross MK, et al. Acute bacterial osteoarticular infections: eight-year analysis of C-reactive protein for oral step-down therapy. Pediatrics 2012;130:e821-8.
10. Wu W, Selva D, Bian Y, et al. Endoscopic medial orbital fat decompression for proptosis in type 1 Graves orbitopathy. Am J Ophthalmol 2015;159:277-84.
11. Chu EA, Miller NR, Grant MP, Merbs S, Tufano RP, Lane AP. Surgical treatment of dysthyroid orbitopathy. Otolaryngol Head Neck Surg 2009;141:39-45.
12. Garrity JA. Orbital lipectomy (fat decompression) for thyroid eye disease: an operation for everyone? Am J Ophthalmol 2011;151:399-400. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in