|
|
 |
 |
 |
 |
|
|
Circumferential viscodilation of Schlemm’s canal with a flexible microcannula during non-penetrating glaucoma surgery
Digital Journal of Ophthalmology 2006
Volume 12, Number 1
March 15, 2006
|
Printer Friendly
|



Bruce Cameron | Northwest Eye Surgeons Michael Field | Northwest Eye Surgeons Michael Field | Northwest Eye Surgeons Stuart Ball | Premier Medical Group John Kearney | Cataract Care Center
|
|
|
| Abstract | Purpose:
A pilot study was performed to evaluate the safety and performance of the flexible Ophthalmic Microcannula (iScience Surgical Corporation, Menlo Park, CA) in accessing and dilating Schlemm’s canal during non-penetrating surgery for the treatment of glaucoma.
Materials and Methods:
Patients with previous surgery, angle recession and combined cases with cataract surgery were allowed for inclusion. Fifty-six glaucomatous eyes with open angles of 56 subjects underwent viscocanalostomy or deep sclerectomy surgery for the treatment of glaucoma by four US surgeons. The flexible microcannula was introduced into Schlemm’s canal at the scleral dissection site and the canal was progressively cannulated, up to the entire canal circumference. Patients were assessed at 1 day, 1 week, and 1, 3, and 6 months following the procedure. A prototype high resolution ultrasound imaging system was used to characterize the anterior segment and Schlemm’s canal when possible.
Results:
The mean baseline intraocular pressure (IOP) of eyes treated with canal dilation during non-penetrating glaucoma surgery was 24.9 mm Hg (SD 9.4) while on 2.1 glaucoma medications. After 180 days post-op, mean IOP of eyes with canal dilation was reduced to 16.4 mm Hg (SD 4.1) while on 0.2 glaucoma medications. No potential life or sight threatening surgical complications were noted. High resolution imaging demonstrated significant dilation of Schlemm’s canal associated with microcannula viscodilation, up to the entire length of the canal.
Conclusions:
Schlemm’s canal dilation up to the entire canal circumference has been demonstrated via a flexible microcannula. Non-penetrating glaucoma surgery with canal dilation demonstrated reduced IOP post-operatively with no sight threatening surgical complications. Specific treatment of the canal to restore natural outflow of aqueous may be a viable means of treating patients with glaucoma. The promising results achieved to date will be further investigated in a larger multi-center study.
| | | Introduction | Most current incisional surgical treatment for open angle glaucoma generally relies upon bypassing the trabeculo-canalicular outflow pathway for aqueous humor. Trabeculectomy, non-penetrating deep sclerectomy, and shunt implantation all involve formation of a flow path from the anterior chamber to a sub-conjunctival bleb or reservoir [1-5]. The aqueous humor subsequently diffuses into conjunctival tissues and the tear film. Post-surgical complications from these forms of glaucoma surgery are often related to the instability of the surgically formed flow path and bleb [5-7] as well as compromised status of the blood-eye barrier.
Previous research into the mechanism of open angle glaucoma has characterized significant changes to the trabeculo-canalicular outflow pathway with disease progression. The trabecular meshwork shows increased flow resistance with age and glaucoma progression [8-10]. Schlemm’s canal demonstrates a reduction in size with age and also appears to be smaller in the histopathology of glaucoma patients [11-13]. The characterization of the trabeculo-canalicular ouflow pathway and its restoration as a treatment for open angle glaucoma is a surgical approach that has been subject to extensive research [14-16]. Goniotomy, a surgical procedure that opens the trabecular meshwork to Schlemm’s canal to restore aqueous outflow to Schlemm’s canal, is a primary surgical treatment for infantile glaucoma as well as many other forms of glaucoma in children, but is generally considered ineffective in open angle glaucoma of adults [17-18].
Recently, interest in restoration of the trabeculo-canalicular outflow pathway has been stimulated by promising results from several different approaches. Viscocanalostomy, a non-penetrating surgical procedure, involves the injection of viscoelastic locally through a small bore, rigid metal cannula into Schlemm’s canal to dilate a portion of the canal and promote flow from a surgically created window in Descemet’s membrane that is permeable to aqueous [19]. Although several studies have demonstrated the effectiveness of viscocanalostomy in IOP reduction [20-22], variances in results are presumably due to surgical technique as well as potential differences in patient population [23]. More recently, innovative implants that form an aqueous connection from the anterior chamber to Schlemm’s canal to restore trabeculo-canalicular outflow have been described [24-26].
To investigate the potential for restoration of the trabeculo-canalicular pathway, this pilot study characterized the surgical results from patients treated with an flexible microcannula (iScience Surgical Corp.) designed to access and dilate up to the entire length of Schlemm’s canal during non-penetrating glaucoma surgery. High resolution ultrasound images were obtained when possible to characterize Schlemm’s canal morphology.
| | | Materials and Methods | The study was designed as a pilot study on the use of a flexible microcannula to access and dilate progressively longer lengths of Schlemm’s canal during non-penetrating glaucoma surgery. Evaluation of microcannula safety and development of surgical methods for use of the microcannula based on patient follow-up examinations and surgeon feedback were primary objectives, with the goal of using the results in the design of a prospective, multi-center study with greater statistical power.
Before entry into the study, informed consent was obtained from all patients. Patients selected were diagnosed with primary open angle glaucoma or primary open angle glaucoma and cataract and were scheduled for glaucoma surgery or combined cataract and glaucoma surgery. Neovascular diseases, uveitis, chronic angle closure and any other condition deemed by the investigator to make study participation inappropriate were exclusionary.
Preoperatively, patients underwent best corrected visual acuity assessment, slitlamp examination, and gonisocopy. IOP was determined by Goldmann applanation tonometry. Demographics and baseline characteristics were obtained for each patient (Table I). After surgery, patients were followed prospectively and assessed at minimum on day 1, 1 week, and at 1, 3 and 6 months. In addition to the biomicroscopy and functional examination at each post-operative follow-up, IOP was assessed to allow use of IOP reduction as an outcome measure and to perform trend analysis of surgical parameters.
Surgical Technique:
The glaucoma surgery was performed in accordance with the current practice of the investigator, with the addition of the flexible microcannula to dilate Schlemm’s canal. One of the investigators performed viscocanalostomy (n=31), while the other three surgeons performed a deep sclerectomy form of non-penetrating glaucoma surgery (n=25). All investigators surgically exposed Schlemm’s canal allowing full access to the ostia. The microcannula was used to additionally dilate Schlemm’s canal in the deep sclerectomy procedures. In the viscocanalostomy procedures, the microcannula was used instead of the standard metal microcannula. The surgically created ostia of Schlemm’s canal were identified at the edges of the dissection. The microcannula was grasped using forceps and the tip was placed in alignment with the canal. The microcannula tip was gradually advanced into the canal. A light beacon incorporated in the microcannula tip was used to assess the positioning of the microcannula. The microcannula was advanced approximately 3 clock hours and up to 12 clock hours, at the surgeon’s discretion, while observing the beacon tip emitting light through the sclera. The canal was expanded by injecting the viscoelastic into the microcannula. Dilation of discrete locations of the canal was performed at one or multiple sites along the length of the canal. As the study progressed, canal dilation was performed continuously along the entire length of the canal. In three cases, the microcannula was unable to cannulate 900 or 3 clock hours, and in two cases the surgeon was unable to progress to the desired clock hour.
Anterior Segment Imaging:
The canal dilation was visualized using a prototype, high frequency ultrasound imaging system (iScience Surgical Corporation, Menlo Park, CA) with approximately 80 MHz frequency and 30 micron resolution, to characterize Schlemm’s canal morphology both during surgery and one day post-surgery. Additional images of patients at longer post-operative periods were obtained when possible within the six month follow-up period.
| | | Results | Microcannula Use
The illuminated tip of the microcannula could be observed transclerally during cannulation of the canal, giving surgical guidance during placement and advancement (Figure 1). During advancement of the microcannula within Schlemm’s canal, investigators occasionally encountered an area of increased mechanical resistance that inhibited further cannulation. In most cases, slight retraction of the microcannula and resumption of cannulation, injection of viscoelastic or a combination of both techniques allowed the area of resistance to be traversed.
Patient Outcome
IOP progress over time for all eyes is graphically displayed in Figure 2. IOP decreased from 25.1 + 8.7 mm Hg at baseline to 15.8 + 6.7 mm Hg on post-operative day 1, and stayed in the 16 – 18 mm Hg range during the six month follow-up. Simultaneously, the anti-glaucoma medication usage dropped from mean 2.1 + 1.0 medications at baseline to mean values ranging from 0 to 0.2 medications post-operatively (Figure 3).
Patients were divided into three groups to further investigate the efficacy of the microcannuala system. Group A (n=44) excludes all nine eyes that had the microcannula inserted into Schlemm’s canal without dilation and three eyes that could not be cannulated. Group B (n=39) excludes an additional five eyes that underwent previous glaucoma surgery. Group C is a subset of group B and consists of 18 eyes that underwent dilation of the canal along the entire circumference by continuous injection of viscoelastic during cannulation. Table II presents the IOP over time for the three groups and all eyes. No clinically significant trend was observed among the subgroups.
IOP equal or less than 21 mm Hg (IOP < 21 mm Hg) without medication was determined for each time interval for all eyes and groups A, B and C (Table III). The proportion of eyes with IOP < 21 mm Hg over time was higher for Group C, i.e., eyes that underwent dilation of the canal along the entire circumference by continuous injection of viscoelastic, than any other group at each post-operative interval. Eyes with no canal dilation were compared to eyes with 1 or 2 focal dilations, 3 or more focal dilations, or continuous 360 degree dilation of the entire canal length (Table IV). Though not statistically significant, the proportion of eyes achieving 21, 18, or 15 mm Hg at 6 months increased with increasing amount of canal dilation, with the exception of 360 degree dilation achieving 18 mm Hg or less.
Loss of more than 2 lines in best corrected visual acuity was in general transient and was mainly reported at post-operative day 1 and post-operative day 7. Only four eyes were reported with a loss of more than 2 lines in visual acuity at the last available visit. These losses were attributed to preexisting/concomitant conditions including extensive preoperative optic nerve damage, preoperative diabetic retinopathy and central retinal vein occlusion and age-related macular degeneration with subsequent vision loss.
Post-operative gonioscopy data showed a significant decrease in the proportion of eyes with Shaffer grade 1 and a significant increase in the proportion of eyes with Shaffer grade 4 as compared to baseline in all four quadrants, possibly associated with concomitant cataract surgery in the combined surgical cases.
Few operative complications were reported. Intraoperatively, three cases of hyphema were reported, two of these cases were accompanied by perforation of Schlemm’s canal and Descemet’s membrane detachment respectively. In addition, rupture of the trabecular meshwork was reported intraoperatively for one eye. The remaining operative complications consisted of one case each of pupillary block requiring YAG iridotomy, corneal abrasion, wound closure, hypotony and choroidal detachment. Post-operative complications included two eyes (3.6%) that required Nd:YAG goniopuncture to control raised IOP, and one eye which was reported with uveitis, decreased visual acuity and elevated IOP. Only one complication, closure of the operative wound with a significant increase in IOP, was considered severe and this complication resolved completely the following day after surgical revision. The remaining complications were rated as mild or moderate in severity.
Anterior Segment Imaging
The post-operative cross-sectional ultrasound images of the anterior segment and Schlemm’s canal obtained from the study eyes showed marked differences in morphology as compared to pre-operative images. Typically Schlemm’s canal appeared preoperatively either as a flattened tissue space in the anterior segment angle or the canal could not be visualized. Immediately post-surgery, Schlemm’s canal was clearly visible as an open tissue space or lumen after passage of the flexible microcannula alone. Injection of viscoelastic into Schlemm’s canal with the microcannula produced a much greater opening of the canal lumen in the region near the tip of the microcannula during injection. The canal demonstrated a maximal cross-sectional dimension in the range of 183 to 373 microns immediately after visco-dilation, as measured by the caliper function of the ultrasound imaging system on images from eight eyes. On the day following surgery, imaging of the treated eyes typically demonstrated a reduced lumen size, presumably due to dissolution of the injected viscoelastic from the canal. In cases where the canal was resolved by imaging pre-operatively, the maximal cross-sectional dimension of the canal was significantly larger post-operatively in the region of viscodilation (Figure 4) even after dissolution of the viscoelastic.
Some treated eyes were available for imaging during the follow-up period. Whereas in most cases Schlemm’s canal could not be well resolved as a tissue space prior to surgery, imaging of the regions dilated during surgery were typically able to be resolved as a flattened canal structure during the six month follow-up period (Figure 5). Images from one patient, #2598 are shown pre-op, immediately post-op, one day post-op (Figure 4A,B,C) and 112 days post-op (Figure 5B). | | | Discussion | In almost all cases, the flexible microcannula allowed the surgeon to access extended lengths of Schlemm’s canal, up to the full circumference. Injection of viscoelastic through the microcannula produced dilation of the canal as demonstrated by high frequency ultrasound imaging of the anterior segment angle. The use of the microcannula was generally free of surgical complications, especially after initial experience.
The patient outcomes in response to glaucoma surgery with microcannula viscodilation of Schlemm’s canal demonstrated post-operative IOP and medication reduction in the range of previously reported non-penetrating glaucoma surgery [27]. Though not statistically significant due to the small number of patients, a trend of greater IOP control without medications was associated with viscodilation of increased lengths of the canal (Table IV).
High resolution ultrasound imaging of the anterior segment and Schlemm’s canal demonstrated significant dilation of the canal lumen associated with viscodilation and noticeable tissue deformation post-operatively. In many eyes imaged throughout the course of the study, Schlemm’s canal was more easily resolved in the areas of canal dilation possibly indicating that flow through the compromised trabeculo-canalicular outflow pathway was increased surgically in some OAG patients. The mechanism for increase of trabecular-canalicular outflow from viscodilation of Schlemm’s canal has been the subject of previous research indicating a potential increase in permeability from stretching of the trabecular meshwork [28].
Due to the promising clinical results from this pilot study, a larger study involving full circumferential dilation of Schlemm’s canal in OAG patients with extended follow-up and more extensive anterior segment imaging has been initiated.
| | | Acknowledgements | | The study authors would like to acknowledge the clinical staffs at the three study centers for their involvement and extra efforts that contributed to this clinical research study. | | | References | 1. Cairns JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol 1968;66(4):673-9.
2. Jones E, Clarke J, Khaw PT. Recent advances in trabeculectomy technique. Curr Opin Ophthalmol 2005;16(2):107-13.
3. Rosengren B. Sinusotomy according to Krasnov. Trans Ophthalmol Soc U K. 1966;86:261-9.
4. Mermoud A. Sinusotomy and deep sclerectomy. Eye 2000;14:531-5.
5. Krupin T. Implanted aqueous shunt devices for glaucoma surgery. J Ophthalmic Nurs Technol 1992;11(1):23-5.
6. Mac I, Soltau JB. Glaucoma-filtering bleb infections. Curr Opin Ophthalmol 2003;14(2):91-4.
7. Ophir A. Encapsulated filtering bleb. A selective review--new deductions. Eye 1992;6:348-52.
8. Grant MW. Experimental aqueous perfusion in enucleated human eyes. Arch Ophthalmol 1963;69:783-801.
9. Grant WM. Further studies on facility of flow through the trabecular meshwork. AMA Arch Ophthalmol 1958;60:523-33.
10. Nesterov AP, Batmanov YE. Trabecular wall of Schlemm's canal in the early stage of primary open-angle glaucoma. Am J Ophthalmol 1974;78(4):639-47.
11. Grierson I, Howes RC, Wang Q. Age-related changes in the canal of Schlemm. Exp Eye Res 1984;39(4):505-12.
12. McMenamin PG, Lee WR, Aitken DA. Age-related changes in the human outflow apparatus. Ophthalmology 1986;93(2):194-209.
13. Boldea RC, Roy S, Mermoud A. Ageing of Schlemm's canal in nonglaucomatous subjects. Int Ophthalmol 2001;24(2):67-77.
14. Krasnov MM. Microsurgery of glaucoma. Indications and choice of techniques. Am J Ophthalmol 1969;67(6):857-64.
15. Ellingsen BA, Grant WM. Trabeculotomy and sinusotomy in enucleated human eyes. Invest Ophthalmol 1972;11(1): 21-8.
16. Moses RA, Grodzki WJ, Etheridge EL, Wilson CD. Schlemm's canal: the effect of intraocular pressure. Invest Ophthalmol Vis Sci. 1981;20(1):61-8.
17. Shaffer RN. Prognosis of goniotomy in primary infantile glaucoma (trabeculodysgenesis). Trans Am Ophthalmol Soc 1982;80:321-5.
18. Hoskins HD Jr, Shaffer RN, Hetherington J. Goniotomy vs trabeculotomy. J Pediatr Ophthalmol Strabismus 1984;21(4):153-8.
19. Stegmann R, Pienaar A, Miller D. Viscocanalostomy for open-angle glaucoma in black African patients. J Cataract Refract Surg 1999;25:316-22.
20. Shaarawy T, Nguyen C, Schnyder C, Mermoud A. Five year results of viscocanalostomy. Br J Ophthalmol 2003;87:441-5.
21. Wishart MS, Shergill T, Porooshani H. Viscocanalostomy and phacovicocanalostomy: long-term results. J Cataract Refract Surg 2002;28:745-51.
22. Jonescu-Cuypers CP, Jacobi PC, Konen W, Krieglstein GK. Primary viscocanalostomy versus trabeculectomy in white patients with open-angle glaucoma: A randomized clinical trial. Ophthalmology 2001;108(2):254-8.
23. Bauchiero L, Demarie A, Belli L, Brogliatti B. Deep sclerectomy and viscocanalostomy: critical revision of the results obtained during the learning curve. Acta Ophthalmol Scand Suppl. 2002;236:64-6.
24. Spiegel D, Kobuch K. Trabecular meshwork bypass tube shunt: initial case series. Br J Ophthalmol 2002;86(11):1228-31.
25. Bahler CK, Smedley GT, Zhou J, Johnson DH. Trabecular bypass stents decrease intraocular pressure in cultured human anterior segments. Am J Ophthalmol 2004;138(6):988-94.
26. Brown R, Clinical Studies on the Eyepass Bi-Directional Glaucoma Implant, Abstracts of the 15th Annual AGS Meeting 2005, Page 46, Abstract 25.
27. Jampel HD, Musch DC, Gillespie BW, Lichter PR, Wright MM, Guire KE and the CIGTS Group. Perioperative complications of trabeculectomy in the collaborative initial glaucoma treatment study. American Journal of Ophthalmology 2005;140(1):16-22.
28. The AGIS Investigators. The Advanced Glaucoma Intervention Study(AGIS): 11. Risk factors for failure of trabeculectomy and argon laser trabeculoplasty. American Journal of Ophthalmology 2002;134(4):481-98.
29. Borisuth, NSC, Bryan P, Krupin T. The risk profile of glaucoma filtration surgery. Current Opinions in Ophthalmology 1999;10(2):112-16.
30. O’Brart DPS, Rowlands E, Islam N, Noury AMS. A randomised, prospective study comparing trabeculectomy augmented with antimetabolites with a viscocanalostomy technique for the management of open angle glaucoma uncontrolled by medical therapy. Br J Ophthalmology 2002; 86:748-54.
31. Luke C, Dietlein TS, Jacobi PC, Konen W, Krieglstein GK. A prospective randomized trial of viscocanalostomy versus trabeculectomy in open angle glaucoma: a 1-year follow-up study. Journal of Glaucoma2002; 11(4):294-99.
32. Yalvac IS, Sahin M, Eksioglu U, Midillioglu IK, Aslan BS, Duman S. Primary viscocanalostomy versus trabeculectomy for primary open-angle glaucoma, Three-year prospective randomized clinical trial. J Cataract Refract Surg 2004;30:2050-57.
33. Goldsmith JA, Ahmed IK, Crandall AS. Nonpenetrating glaucoma surgery. Ophthalmol Clin North Am 2005;18(3):443-60.
34. Smit BA, Johnstone MA. Effects of viscoelastic injection into Schlemm’s canal in primate and human eyes. Ophthalmology 2002;109:786-92.
| |
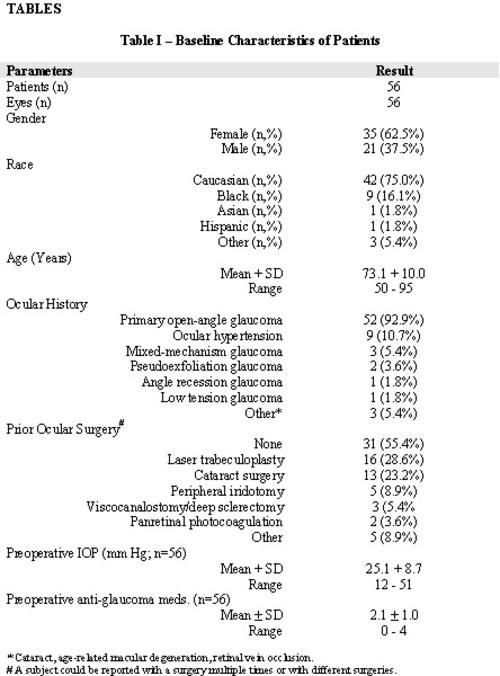
Table 1
|
|
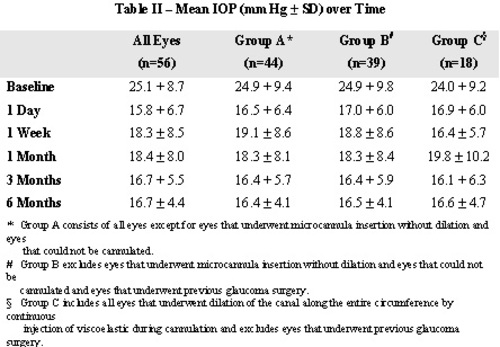
Table 2
|
|
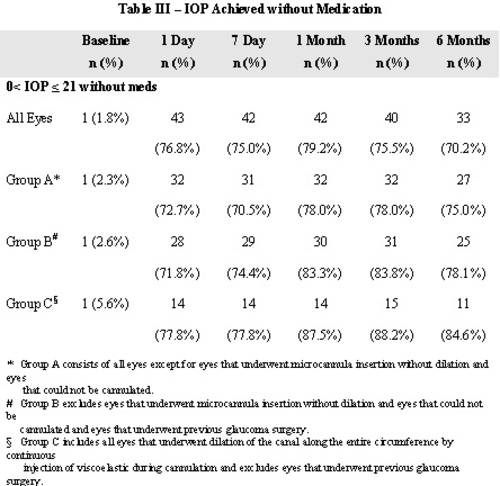
Table 3
|
|
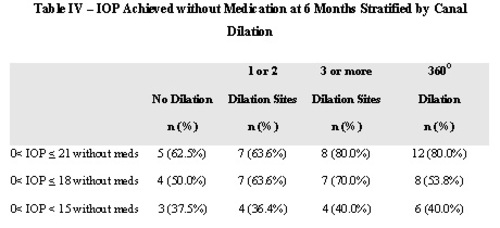
Table 4
|
|

Figure 1
Flexible microcannula with illuminated beacon tip visible transclerally during cannulation of Schlemm’s canal.MC = microcannula. Dashed arrow shows the microcannula path within Schlemm’s canal, and the dashed circle shows the area of beacon tip illumination.
|
|
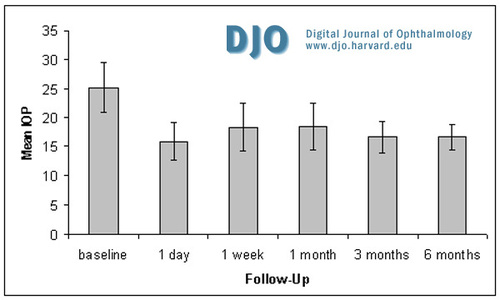
Figure 2
Mean IOP (+ SD) in all eyes over time.
|
|
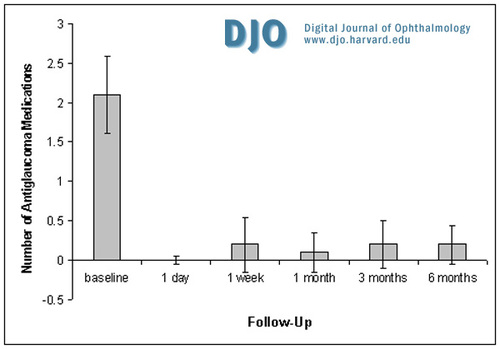
Figure 3
Mean number of anti-glaucoma medications (+ SD) in all eyes over time.
|
|

Figure 4A
Ultrasound imaging - cross-section of anterior segment angle of patient #2598 at 9:00 OSA pre-operatively.
|
|
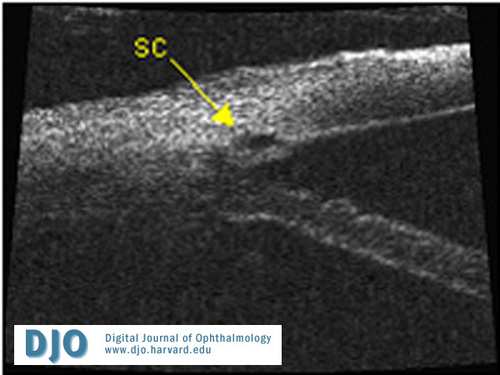
Figure 4B
Ultrasound imaging - cross-section of anterior segment angle of patient #2598 at 9:00 OSB immediately post-operatively demonstrating local viscodilation of Schlemm’s canal (SC).
|
|

Figure 4C
Ultrasound imaging - cross-section of anterior segment angle of patient #2598 at 9:00 OS one day post-op.
|
|

Figure 5A
Ultrasound imaging - cross-section of anterior segment angle of patient #208 at 6:00 OD, 148 days post-op.
|
|
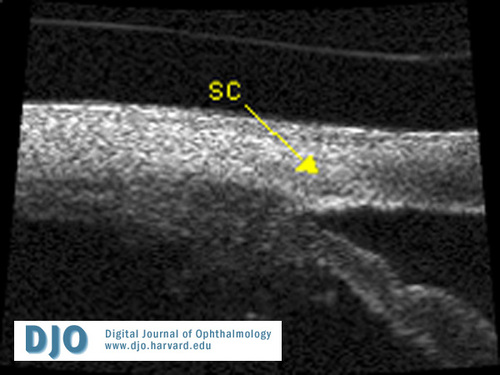
Figure 5B
Ultrasound imaging - cross-section of anterior segment angle of patient #2598 at 9:00 OS at 112 days post-operatively.
SC = Schlemm’s canal.
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in