|
|
 |
 |
 |
 |
|
|
Bilateral orbital metastases from gastric adenocarcinoma presenting as presumed thyroid-related orbitopathy
Digital Journal of Ophthalmology 2005
Volume 11, Number 3
May 19, 2005
|
Printer Friendly
|



Christine S. Ament M.D. | Massachusetts Eye and Ear Infirmary Mark P. Hatton M.D. | Massachusetts Eye and Ear Infirmary Paul Caruso M.D. | Massachusetts Eye and Ear Infirmary Roger F. Lange M.D. | Mount Auburn Hospital Jenny Hong M.D. | Massachusetts Eye and Ear Infirmary Peter A.D. Rubin M.D. | Massachusetts Eye and Ear Infirmary
|
|
|
| Abstract | Objective
To present the case of a 72 year old woman with gastric adenocarcinoma metastatic to both orbits masquerading as thyroid-related orbitopathy.
Methods
Case report.
Results
A 72 year old woman developed double vision and conjunctival injection OU and was referred for evaluation of possible euthyroid thyroid-related orbitopathy. Her history was notable for unresectable gastic carcinoma. She was not proptotic, did not have lid retraction, but had marked limitation of eye movements OU in all directions of gaze. CT scans showed diffuse orbital masses OU. Her medical history and CT findings raised the suspicion of bilateral orbital metastases. This was confirmed with biopsy. Radiation to the orbits improved motility and injection but she died 1 month after completing treatment.
Conclusion
Ophthalmologists should consider metastatic cancer in the differential diagnosis of atypical orbitopathy.
Keywords
thyroid-related orbitopathy ; metastases ; proptosis ; ophthalmoplegia | | | Introduction | | A variety of orbital disorders, including infectious, inflammatory, and neoplastic, may present with findings suggestive of thyroid related orbitopathy, including proptosis, lid retraction, and decreased ocular motility. These entities should be considered when evaluating patients with presumed thyroid orbitopathy, and details from the history and examination can be useful in determining the correct diagnosis. | | | Materials and Methods | | Report of a case | | | Results | A 72 year-old woman was referred for evaluation of presumed euthyroid Grave's orbitopathy. She developed red eyes and double vision 2 months prior to presentation during hospitalization for surgery to remove a gastric tumor. Ophthalmology was consulted and the possibility of thyroid-related orbitopathy was raised, and she was referred with this diagnosis. Thyroid tests performed at that time were normal.
Her ocular history was unremarkable. Her medical history was significant for gastric adenocarcinoma diagnosed 2 years prior to presentation. She was treated with carboplatinum at that time. An attempt to remove the remaining tumor surgically was performed 2 months prior to our examination. This surgery was aborted when metastases to local lymph nodes and intraperitoneal spread was observed intra-operatively.
At presentation, visual acuity was 20/50 OD and 20/40 OS. There was no afferent pupillary defect. Motility was reduced in all directions OU. Lower eyelid retraction and lagophthalmos were present OU (Figure 1). There was no upper lid retraction. Exophthalmometry measurements were 21 mm OD and 20 mm OS. Anterior segment examination was significant for superficial punctate keratitis and conjunctival chemosis OU. Posterior segment examination was normal.
CT scan demonstrated diffuse masses throughout both orbits (Figure 2a and 2b). Biopsy via anterior orbitotomy demonstrated poorly differentiated carcinoma (Figure 3). Cells were positive for cytokeratins (AE1, 3/CAM5.2, CK7, CK20) and negative for leukocyte common antigen (LCA). A specific breast cancer marker (CGDFP) was negative. The original biopsy slides were reviewed. Malignant cells seen in the metastatic lymph node were poorly differentiated carcinoma cells similar in appearance to cells from the orbital lesion.
The patient was treated with 30 Gray of orbital radiation, divided over 10 doses. Motility, lid closure, and corneal appearance improved after treatment. She developed progressive intra-abdominal disease and died 1 month after completing radiation treatment.
| |

Figure 1.
Appearance at presentation.
|
|

Figure 2a
Coronal CT scan showing fiffuse masses in both orbits.
|
|

Figure 2b
Axial CT scan showing diffuse masses in both orbits.
|
|
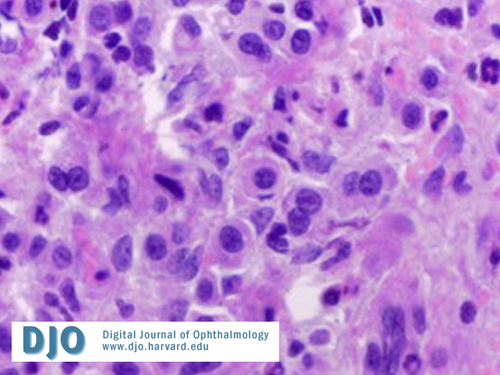
Figure 3.
Histology specimen from biopsy of the orbital mass.
|
|
| Discussion | Comment
Metastatic cancer is a rare cause of symptomatic orbital disease, and bilateral disease is exceedingly rare. Bilateral orbital metastases have been reported in association with breast, lung, and bladder cancer, lymphoma and neuroblastoma. We found two cases of bilateral orbital metastases from gastric cancer reported in the literature. One patient presented with proptosis and restricted motility; details of the second case are not reported. (1,2)
Orbital metastases from gastrointestinal malignancies are uncommon and occur more frequently with breast and lung cancer. (3,4) It is hypothesized that the frequency of lung metastases is due to a biologic capacity for early spread, but that the frequency of breast metastases is due to improvements in breast cancer treatment that allow patients to live for many years with their disease. (3) Orbital symptoms usually precede diagnosis of lung primary, but follow diagnosis of breast primary. (4,5) Gastric cancer metastasizes through lymphatic channels. Thirty-nine percent of patients have advanced intra-abdominal disease at diagnosis, and distant metastases are always accompanied by extensive local spread. (6) Many patients die of complications of local disease before distant metastases are symptomatic.
This patient presented with presumed Graves orbitopathy but had several features that made thyroid-related orbitopathy less likely, including lack of proptosis, isolated lower eyelid (but not upper) retraction, severely limited eye movements in all fields, and normal thyroid function tests. Ophthalmologists should seek detailed medical history and consider metastatic disease in patients with unusual orbitopathy.
| | | References | References
1. Albert DM, Rubenstein RA, and Scheie HG : Tumor metastasis to the eye. Am J Ophthalmol 1967;63:723-726.
2. Van Gelderen, WFC. Gastric carcinoma metastases to the extraocular muscles. J Comp Assist Tomog 1993;17: 499-500.
3. Ferry AP and Font RL. Carcinoma metastatic to the eye and orbit I. A clinicoathologic study of 227 cases. Arch Ophthalmol 1974;92: 276-286.
4. Amemiya T, Hayashida H, and Dake Y, Metastatic orbital tumors in Japan: A review of the literature. Ophthal Epidemiol 2002;9:35-47.
5. Char DH, Miller T, and Kroll S. Orbital metastases: diagnosis and course. Br J Ophthalmol 1997; 81:386-390.
6. Hundahl, S. Staging, stage migration, and patterns of spread in gastric cancer. Semin Rad Oncol 2002;12:141-149.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in