|
|
 |
 |
 |
 |
|
|
Management of subretinal gas complication following pneumatic retinopexy
Digital Journal of Ophthalmology 2004
Volume 10, Number 2
May 14, 2004
|
Printer Friendly
|


 Julie Chen
Julie Chen | Massachusetts Eye and Ear Infirmary and Harvard Medical School Ivana Kim, M.D. | Massachusetts Eye and Ear Infirmary and Harvard Medical School Joan Miller, M.D. | Massachusetts Eye and Ear Infirmary and Harvard Medical School
|
|
|
| Abstract | | Pneumatic retinopexy is a popular and effective procedure for treating retinal detachments. We report a case of a 60-year-old female who presented with a large superior horseshoe tear and associated retinal detachment of the left eye. She underwent pneumatic retinopexy complicated by subretinal gas, which was successfully managed with vitrectomy with perfluorocarbon liquid injection and fluid/exchange. Following the case presentation, treatment options for the management of subretinal gas will be discussed. | | | Discussion | CASE PRESENTATION
A 60-year-old female presented with complaints of floaters and lines in the left eye for several days. On the day of her visit, she noted loss of vision in the inferior visual field of the left eye. Her ocular history was notable for laser retinopexy in the left eye for a retinal tear 10 years earlier. Her medical history and family history was noncontributory, and she was not using any ocular medications.
Examination
Visual acuity with correction was 20/25 OD and 20/40 OS. Pressures were 12 OU. Slit-lamp examination showed trace nuclear sclerosis OU. Dilated fundus exam revealed a bullous retinal detachment in the left eye from 10 o'clock to 1 o'clock extending posteriorly to just above the superotemporal arcade. A superior horseshoe tear approaching one clock hour in size with significant vitreous traction on the flap was noted at 12 o'clock, anterior to the equator. An operculated hole was also noted just temporal to the tear (Figure 1). Pigmentary change consistent with previous laser was noted in the inferior periphery. Fundus examination of the right eye was unremarkable.
Treatment Course
The patient was treated initially with pneumatic retinopexy. Cryopexy was first applied to the retinal breaks, and 0.3 cc of 100% perfluoropropane (C3F8) was injected 4 mm posterior to the limbus at the 4:00 meridian using a 30 gauge needle. A paracentesis was then performed, yielding 0.2 cc of aqueous fluid. The gas injection was complicated by the formation of multiple small gas bubbles, many of which migrated subretinally. Most of the bubbles dislodged with supine positioning. The patient was then instructed to maintain strict face-down positioning. However, fundus examination 8 hours after the procedure revealed increased subretinal gas with large bubbles extending from 12 o'clock to 2 o'clock (Figure 2).
The decision was made to proceed with pars plana vitrectomy to remove the subretinal gas. Using a wide-angle system for visualization, vitrectomy was performed with careful attention to the region of the tear. Peripheral vitreous was removed with the aid of scleral depression. A small amount of subretinal gas was removed with aspiration using the vitrectomy handpiece. Perfluorocarbon liquid was then injected to push the remaining subretinal gas through the retinal tear. Substantial flattening of the retina was observed, but a small pocket of subretinal gas remained anteriorly. A retinotomy was created anteriorly at 11 o'clock to release the remaining gas. Air-fluid exchange was then performed. A small bubble (approximately 500 um in diameter) of subretinal gas remained. Air was then exchanged with 14% perfluoropropane (C3F8) and the sclerotomies closed. At the end of the case, the intraocular pressure was in the range of 10-15 mm Hg. The patient received 600 mg intravenous clindamycin preoperatively and a subconjunctival injection of gentamicin and decadron at the end of the procedure.
On the first postoperative day, fundus examination revealed an attached retina with a small subretinal gas bubble and 80-90% gas fill. One week after surgery, fundus examination revealed an attached retina with 80-90% gas fill and no subretinal gas remaining. Slit lamp examination revealed 1+ posterior subcapsular cataract. At 11 weeks, the visual acuity in the operated eye was 20/125 improving to 20/40 with pinhole. Slit-lamp examination revealed 3+ nuclear sclerosis and 1+ posterior subcapsular cataract. A layering of tiny bubbles was noted in the inferior angle, which was felt to be residual perfluorocarbon liquid. Fundus examination revealed an attached retina with minimal gas remaining, and there were mild epiretinal membrane changes noted. (See Figure 3). Five months after her initial presentation, the patient underwent bilateral phacoemulsification with placement of PCIOL. One month later, her visual acuity without glasses in the operated eye was 20/63, improving to 20/32 with pinhole.
DISCUSSION
Development of subretinal gas
This case demonstrates successful management of subretinal gas following pneumatic retinopexy. managed with pneumatic retinopexy. Subretinal gas is an established but rare complication of pneumatic retinopexy, occurring in about 1-5% of cases(1-3). McDonald et al. suggest that subretinal gas is usually a preventable complication, directly related to the presence of small bubbles or "fish eggs" in the vitreous following injection. They emphasize the importance of a careful injection technique to insure formation of a single gas bubble(4). If multiple bubbles are present, they advocate trying to create a single bubble by a "swab-snap" technique, described as bending and releasing a flexible swab against the sclera above the location of the bubbles. McDonald et al. argue that careful injection, followed by the swab-snap technique when needed, should prevent many cases of subretinal gas. Wong et al. hypothesize that unrelieved vitreoretinal traction in the presence of gas in the retrohyaloid space encourages development of subretinal gas. To prevent migration of gas bubbles under the retina, they propose relieving the vitreoretinal traction through scleral buckling(18).
Management of subretinal gas
Many options for the management of subretinal gas have been described, including scleral depression, positioning, scleral buckling, vitrectomy, and perfluorocarbon liquid injection. In many cases, the subretinal gas bubble can be maneuvered back through the retinal break using scleral depression and indirect ophthalmoscopy(7). If this fails and the amount of subretinal gas is small, strict prolonged positioning may resolve the detachment by allowing gas to escape through the retinal break into the vitreous cavity(7). However, Wong et al. caution that in some cases, positioning is unlikely to evacuate subretinal gas and may even lead to an extension of the detachment(5). Larger amounts of subretinal gas can be removed with a needle passed through the sclera and into the subretinal space. If the subretinal gas persists despite these maneuvers, McDonald et.al suggest attempting scleral buckling first, reserving vitrectomy and air-fluid exchange for cases with large amounts of subretinal gas(17).
We found a total of 13 cases in the literature on the management of subretinal gas complications following pneumatic retinopexy (See Table 1 for a summary of subretinal gas management in prior case reports). In 11 out of 13 cases reported, the retina was successfully reattached following the additional procedures. Of note, in the two unsuccessful cases, patients refused additional surgical intervention beyond positioning and pneumatic retinopexy. In 8 out of the 11 successful reattachments, pars plana vitrectomy +/- scleral buckling was utilized to manage the subretinal gas. In one case, vitrectomy plus scleral buckling was unsuccessful, and perfluorocarbon injection followed by buckle revision was needed to manage the subretinal gas. In the two remaining cases, the subretinal gas was managed with positioning alone in the first case, and scleral buckling plus cryopexy in the second case. In our patient, pars plana vitrectomy followed by perfluorocarbon liquid injection and air-fluid exchange was successful in reattaching the retina. The vitrectomy procedure was greatly facilitated by the wide-angle viewing system, and scleral buckling was not performed.
Our case is not the first report of perfluorocarbon liquid used to manage subretinal gas. Brown and Kirkby reported a case in 1997 of subretinal gas managed with scleral buckle, pneumatic retinopexy, and perfluorodecalin injection(19). In their patient, the retinal detachment was initially managed with cryopexy and exoplant. Postoperatively, the retina remained detached, and the patient underwent pneumatic retinopexy. However, three weeks later, the patient experienced redetachment, and subretinal gas was noted on exam. Standard pars plana vitrectomy was performed, and perfluorodecalin was introduced to push out the subretinal gas and fluid anteriorly through the original retinal break. Following air-fluid exchange, additional cryopexy was applied to the retinal breaks, and the scleral buckle was repositioned to support the breaks.
In our case report, we demonstrate that perfluorocarbon liquid can be used successfully to displace subretinal gas and achieve retinal reattachment without the use of scleral buckling. The use of a wide-angle viewing system greatly facilitated the procedure by allowing careful peripheral vitrectomy without requiring either lensectomy or scleral buckling. Postoperatively, our patient had a small (500 um diameter) subretinal gas bubble that dissolved after one week without complications. Postoperative retention of perfluorocarbon liquid is a common occurrence, estimated at 1-3.5% of cases, but very small amounts are unlikely to result in complications.
Conclusion
With the increasing use of pneumatic retinopexy to treat retinal detachments, complications such as subretinal gas will be encountered more frequently. Proper management of these complications is essential to achieving good visual outcomes. Our patient provides an example of the successful management of a subretinal gas complication following pneumatic retinopexy through the use of vitrectomy, wide-angle viewing, and perfluorocarbon liquid.
| |
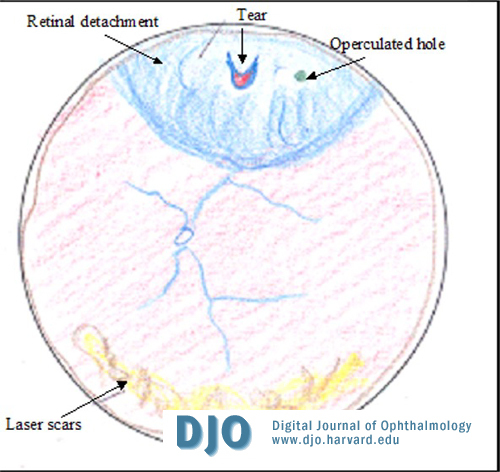
Figure 1
Fundus drawing of the left eye at presentation shows a large superior horseshoe tear with bullous retina detachment.
|
|
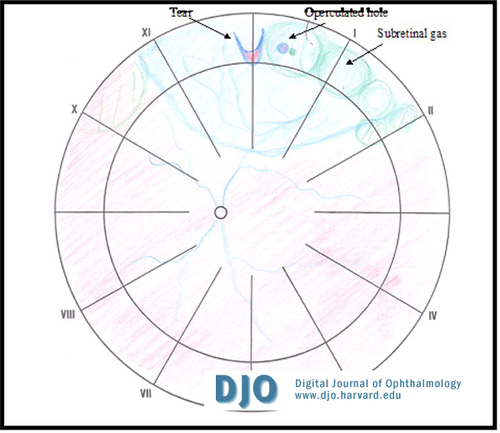
Figure 2
Fundus drawing of the left eye 8 hours after pneumatic retinopexy showing multiple bubbles of subretinal gas superiorly.
|
|

Figure 3
Fundus photograph of the left eye shows an attached retina. The phhotograph was taken 11 weeks after pneumatic retinopexy and subsequent vitrectomy to release subretinal gas.
|
|
| References | 1. Brinton DA, Hilton GF. Pneumatic Retinopexy and Alternative Retinal Reattachment Techniques. In Wilkinson CP, ed. Retina 3rd edition, Volume III. St Louis: CV Mosby, 2001; 2047-2062
2. Grizzard WS, Hilton GF, Hammer ME, Taren D, Brinton DA. Pneumatic Retinopexy Failures: Cause, Prevention, Timing, and Management. Ophthalmology 1995; 102(6); 929-936
3. Abecia E, Pinilla I, Olivan JM, Larrosa JM, Polo V Honrubia FM. Anatomic Results and Complications in a Long-Term Follow-up of Pneumatic Retinopexy Cases. Retina 2000 20(2); 156-161
4. McDonald, H. Richard, Abrams GW, Irvine AR, Sipperley JO, Boyden BS, Fiore JV, Zegarra H. "The Management of Subretinal Gas Following Attempted Pneumatic Retinal Reattachment." Ophthalmology 1987; 94(4): 319-326
5. Wong D, Ansons AM, Chignell AH, Yeoh R. Subretinal Gas. Eye 1990; 4:469-72
6. Brown AD, Kirkby GR. Removal of Subretinal Gas Using Perfluorocarbon Liquid. Retina 1997; 17(1); 71-72
7. Lose M, McDonald R, Campo R, Boyer DS, Schatx H. Pneumatic Retinopexy: Surgical Results. Archives of Ophthalmology 1988; 106:1670-1676
8. Elsing FH, Fekrat S, Green WH, Chang S, Wajer SD, Haller JA. Clinicopathologic findings in eyes with retained perfluoro-n-octane liquid. Ophthalmology 2001;108 (1): 45-48
| | | Tables |
Author |
Case |
Removal |
Final Result |
Visual Acuity |
Comment |
McDonald |
1 |
PPV, SB, AFX, Laser |
Attached |
20/70 |
|
|
2 |
PPV, AFX, Cryo |
Attached |
20/20 |
|
|
3 |
SB, Cryo |
Attached |
20/50 |
|
|
4 |
PPV, SB, AFX, Cryo |
Attached |
20/60 |
|
|
5 |
Positioning, Pneumatic, Cryo |
Detached |
HM |
Re-detached 2 weeks after positioning.
repeated pneumatic. Patient refused further surgery. |
|
6 |
Positioning |
Detached |
HM |
Patient refused further surgery. |
|
7 |
Positioning |
Attached |
20/20 |
Swab snap also performed |
Lowe |
8 |
PPV, SB, AFX, laser |
Attached |
20/200 |
|
Wong |
9 |
Positioning, PPV, AFX, Cryo, silicone oil, SB |
Attached |
N/A |
Failed positioning. re-detached 3 weeks after
PPV then treated with SB |
|
10 |
SB, PPV, AFX, Cryo |
Attached |
N/A |
Subretinal gas
persisted after SB, proceded to PPV |
Grizzard |
11 |
PPV, AFX |
Attached |
N/A |
Limited data available |
|
12 |
PPV, AFX |
Attached |
N/A |
Limited data available |
Brown |
13 |
SB, PPV, Perflurocarbon, AFX, Cryo |
Attached |
20/60 |
Failed SB with cryo prior to pneumatic. Tyre,
band and sleeve positioned to support breaks. |
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in