|
|
 |
 |
 |
 |
|
|
Flipped ophthalmology classroom augmented with case-based learning
Digital Journal of Ophthalmology 2021
Volume 27, Number 1
February 1, 2021
DOI: 10.5693/djo.01.2021.01.004
|
Printer Friendly
Download PDF |


 Ryan J. Diel, MD
Ryan J. Diel, MD | Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals & Clinics, Iowa City, Iowa Kelly H. Yom, BS | Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals Clinics, Iowa City, Iowa David Ramirez, MD | Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals & Clinics, Iowa City, Iowa Karam Alawa, MD | Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals & Clinics, Iowa City, Iowa Justine Cheng, MD | Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals & Clinics, Iowa City, Iowa Salma Dawoud, MD | Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals & Clinics, Iowa City, Iowa Michelle R. Snyder, MD | Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals & Clinics, Iowa City, Iowa Pavlina S. Kemp, MD | Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals & Clinics, Iowa City, Iowa
|
|
|
| Abstract | Background
Although the flipped classroom model provides an effective way to teach ophthalmology to medical students, there are concerns that it overburdens the learner. The purpose of this study was to assess medical students’ perceptions of a case-based flipped classroom style compared with a traditional didactic lecture series and to evaluate the effects of case-based learning on students’ confidence in managing common ophthalmic complaints.
Methods
We created an interactive, case-based flipped classroom ophthalmology curriculum. Paired pre- and post-clerkship surveys were distributed to students on the first and last day of the 2-week clerkship. Questions were formatted as statements using a 6-point Likert scale to assess students’ prior exposure to a flipped classroom, perceptions of the flipped classroom curriculum, and confidence in evaluating ophthalmic complaints.
Results
A total of 75 students were included during the period July 2019 to March 2020. Pre-clerkship questionnaires revealed no preference for either teaching modality. Wilcoxon signed-rank testing comparing pre- and post-clerkship data revealed a significant increase in students’ favoring the case-based flipped-classroom model. Participants reported significant reductions in pressure to perform, course burden, and overall anxiety as well as increased confidence in triaging common eye complaints.
Conclusions
The case-based flipped classroom modality prioritizes key learning objectives while increasing student participation and confidence. The reproducibility and accessibility of standardized prepared video lectures and cases may help institutions to better incorporate ophthalmology into preexisting rotations. | | | Introduction | Exposure to ophthalmology represents an increasingly small fraction of medical education. While most medical schools offer preclinical exposure to ophthalmology, clinical exposure is largely institution dependent and in some cases nonexistent.(1) Comparatively, diseases of the eye and adnexa profoundly affect patients’ quality of life and comprise nearly 5% of outpatient primary care and emergency department visits.(2) This disparity suggests that ophthalmic medical education in its current form may be inadequate in preparing future primary care providers to manage these conditions.(3) Increased time commitment for both faculty and participants seems to be a driving force to decrease eye-related course hours.(4) There are no Liaison Committee on Medical Education (LCME) requirements addressing ophthalmology; however, LCME and medical school curriculum committees emphasize core rotations in the medical student experience. As the amount of knowledge expected of students increases across all disciplines, there is less emphasis on subspecialties such as ophthalmology.(1)
Previously, we demonstrated that implementing a primary care-focused, fully flipped classroom modality through the use of electronically delivered lecture material followed by in-class sessions resulted in higher clerkship satisfaction scores without negatively affecting knowledge acquisition.(5) The purpose of this study was to examine students’ perceptions of the ophthalmology clerkship prior to and after engaging with the flipped-classroom model augmented with case-based learning to determine whether a case-based model is preferred over the traditional classroom and to determine whether case-based learning helps students feel more confident in their ability to handle a variety of ophthalmic complaints in a primary care setting.
| | | Materials and Methods | This study was determined to be exempt from approval by the University of Iowa Institutional Review Boards. Students were informed that participation in this study was voluntary and assured that their participation and answers would not affect their performance in the clerkship.
Curriculum Structure
At the University of Iowa, the introductory clinical ophthalmology clerkship comprises a 2-week selective rotation. Each session accommodates a maximum of 8 medical students who have completed their 3rd semester of medical school. Over 100 medical students participate each year.
The flipped classroom curriculum, implemented in 2017, is a chief-complaint-based model with a primary care focus. Ten pre-recorded online video lectures, ranging in length from 24 to 35 minutes, were prepared in advance by the clerkship director. Each video corresponded to a chapter of the American Academy of Ophthalmology Basic Ophthalmology textbook.(6) At the start of the rotation, students were given access to the video lectures, lecture slide sets, and a course textbook. All content, including the modules and videos used can be found on EyeRounds.org (https://eyerounds.org/article/online-ophthalmology-curriculum/index.htm). Prior to daily learning sessions, students were asked to watch the lecture, view the slide set, or read the textbook chapter corresponding to that day’s topic. The in-class session was then dedicated to interactive case-based discussions led by faculty, fellows, or residents. The flipped classroom model stands in contrast to the traditional classroom, in which class time is used to deliver a didactic lecture with limited time for in-class discussion.
In addition to daily classroom time, the rotation included an eye examination skills session led by an ophthalmology resident, mid-clerkship feedback discussion with the clerkship director, and evaluation of clinical notes by residents and faculty. On the last day of the clerkship, students took a computerized multiple-choice examination. These parameters remain an integral part of the clerkship and were not factored into our analysis.
Study Design
In order to investigate learner attitudes before and after participation, we performed a prospective study consisting of paired pre-/post-surveys. Between July 2019 and March 2020, 75 students were surveyed. On the first day of the rotation, all students were asked to complete a 20-question survey. Students were asked whether they had heard of the flipped classroom approach, whether they had participated in a flipped classroom before, and whether they were considering a career in ophthalmology. Additional questions were formatted as statements using a 6-point Likert scale to assess students’ perceptions of the flipped classroom curriculum, and confidence in evaluating ophthalmic complaints before the rotation. On the last day of the rotation, all students were asked to complete the same set of questions and to state whether the course had enhanced their interest in the field of ophthalmology.
Statistical Analysis
Descriptive statistics were used to determine survey data means and proportions. The Wilcoxon signed-rank test was used to compare survey responses before and after clerkship participation. To analyze associations between groups further, the Likert responses “strongly agree,” “agree,” and “somewhat agree” were grouped together into one cohort; the Likert responses “strongly disagree,” “disagree,” and “somewhat disagree” were grouped in another. These dichotomous categorical variables were analyzed using ?2 analysis or the Fisher exact test. Statistical significance was set at P < 0.05. Statistical analysis was performed using SPSS Statistics (IBM, Armonk, NY). Because these data were a convenience-based sample, no calculations pertaining to power or sample size were performed. | | | Results | A total of 75 students completed the rotation and were included in this analysis: 6 second-year students, 23 third-year students, and 45 fourth-year students. One student did not report medical year status. Prior to participating in the ophthalmology clerkship, 85.3% of the students (n = 64) were familiar with a flipped classroom approach, and 81.3% (n = 61) had participated in a flipped classroom previously. Only 16% (n = 12) students indicated they were considering a career in ophthalmology prior to the clerkship.
Pooled data collected from all students on the first day of the clerkship revealed no preference for either the traditional or flipped classroom modality (mean with standard deviation, 3.53 ± 1.08, with 1 representing a strong preference for a traditional classroom and 6 representing a strong preference for a flipped classroom). Of the 75 students, 40 (54%) indicated that they preferred the flipped modality over the traditional lecture format. Likewise, data regarding course burden and anxiety were also neutral rated. However, students did agree that there was increased pressure to perform in a flipped classroom (mean, 4.61 ± 0.95).
Students with previous personal experience participating in a flipped classroom indicated that they preferred this modality to a traditional didactic series compared with those who had no such prior experience (P = 0.034). Pre-clerkship data indicated that those students who preferred the flipped classroom felt that the flipped classroom environment created more opportunities to learn (P = 0.003), enhanced critical thinking (P = 0.021), was more efficient (P = 0.001), and enhanced communication skills (P = 0.001) compared with those who preferred the traditional classroom. There was no association between students considering a career in ophthalmology and preference for the flipped classroom modality (P = 0.832). See Table 1. One student did indicate having previously participated but did not complete the survey in its entirety.
After completing the flipped classroom clerkship, nonparametric paired analysis revealed a significant increase in student ratings favoring a flipped classroom model over a traditional format (P < 0.001). Cited benefits included reduction in pressure to perform (P = 0.001), course burden (P = 0.002), and anxiety (P < 0.001) and increased confidence triaging common eye complaints (P < 0.001), acute vision loss (P = 0.036), and eye pain (P < 0.001). On average, students reported a higher interest in the field of ophthalmology (P < 0.001) after the clerkship, despite only 4 students indicating that they had changed their minds and were now considering a career in ophthalmology. Likewise, students felt that the flipped classroom should be used in other medical subspecialties (P = 0.003). There were no significant changes in the mean survey responses for any of the other questionnaire statements (Table 2). | | | Discussion | We created an interactive ophthalmology curriculum structured as a flipped classroom augmented with case-based learning. In this study, flipped classroom was defined as a technique that encourages active participation by instructing students to watch prerecorded lectures before class followed by interactive, small-group, case-based learning in-class. We then assessed students’ perceptions of this format compared to a traditional lecture series and their confidence in evaluating ophthalmic complaints. Students favored the case-based flipped classroom modality, which prioritizes key learning objectives while increasing participation and confidence triaging eye complaints. We believe that the reproducibility and accessibility of standardized prepared video lectures and cases will help other institutions better incorporate ophthalmology into preexisting rotations.
A variety of approaches have been used to address the decreasing emphasis of ophthalmology in medical education including: e-modules,(7) multimedia tools,(8) peer-to-peer learning,(9) and the flipped classroom.(10,11) Most recently, we demonstrated that the flipped classroom is an effective way to teach ophthalmology to medical students without sacrificing knowledge acquisition.(5) Nonetheless, there are drawbacks to the flipped classroom approach, especially with regard to the perceived burden and pressure placed on the learner(10) and the increased time required of the educator, who must prepare the prerecorded lectures, design cases, and lead interactive sessions. In this study, we sought to create an efficient and reproducible curriculum through the use of case-based learning in a flipped classroom setting.
We found that the majority of students surveyed had already participated in a flipped classroom prior to this study, and those with a previous personal experience participating in a flipped classroom favored this modality. Frequently cited benefits to the flipped classroom included more opportunities to learn and think critically, increased efficiency, and enhanced communication skills. Despite these cited benefits expressed by the majority, pooled data from all students did not reveal a strong preference for either the flipped or traditional classroom. These results suggest some degree of hesitancy on the part of many students, particularly those without a personal experience participating in a flipped classroom. As supported by the literature, the main factor driving this preference appeared to be feelings of increased pressure to perform in a flipped classroom setting.(10,11) Taken together, these data suggest that hesitancy may be driven by preconceived notions of a flipped classroom intensifying the pressure to perform.
We chose to use a flipped classroom augmented with high-yield cases, because team-based learning via case-based presentations has been shown to provide a supportive, nonintimidating environment that fosters independent clinical reasoning while increasing the overall enjoyment of learning.(12) We were able to create an interactive curriculum that prioritized what primary care physicians need to know about ophthalmology in an easily reproducible format. We hypothesized that by allowing students to take advantage of the flipped classroom lecture content before the in-person case-based lecture series, students would feel more confident and less anxious during the case-based discussions. Additionally, by eliminating the need to create their own case discussion, we feel our curriculum structure lessened overall course burden for the learner. Indeed, students reported significantly less anxiety, less course burden, and a decreased pressure to perform after having the opportunity to participate in our flipped classroom case-based learning.
Although the majority of students were not considering a career in ophthalmology, our curriculum model did enhance interest in the field. We believe that our approach achieves this, because the flipped classroom is an effective way to teach ophthalmology(5) and because use of focused interactive cases has been shown to increase retention and ability to apply knowledge.(12) Clinical clerkships that have limited preclinical emphasis, such as dermatology, otolaryngology, orthopedics, and urology, may also use this approach to better enhance their didactics.
Potential limitations to this study include the pre/post survey design, lack of longitudinal follow-up, use of an even-numbered Likert scale without a “neutral” option, and self-evaluation. This study focused primarily on learner satisfaction, with a curriculum designed to be easy to deliver and highly reproducible. Because our curriculum aimed to increase learner satisfaction, participants may have been biased toward it. Additionally, confidence in knowledge and skills would be expected to increase regardless of whether the traditional or flipped classroom format was employed. This portion of the study does not demonstrate the superiority of the flipped classroom approach to the traditional classroom but does address its effectiveness.
Study strengths include its prospective nature, with matched pre/post questionnaires allowing for individual comparison over a 2-week timeframe. By emphasizing case-based learning, we were able to tailor our curriculum to prioritize what primary care physicians need to know about ophthalmology. Furthermore, we believe that the reproducibility and accessibility of our curriculum changes will help other institutions without dedicated ophthalmology rotations to incorporate ophthalmology into preexisting rotations, particularly programs training front-line providers. Our results also demonstrate that students do not need to have a particular interest in the subject matter or an interest in pursuing ophthalmology as a career to view the curriculum positively. This supports the applicability of this format to a wide breadth of subspecialties, particularly as time constraints in medical school tighten.
Medical school education is increasingly embracing remote and digital formats for learning. Further work is required to assess the efficacy of the flipped classroom model in a completely virtual setting, as required, for example, by COVID-19 physical distancing constraints. Nevertheless, because our model uses prerecorded lectures delivered electronically and synchronous discussions that can be shared over video conferencing, we believe that the flipped classroom model is very adaptable and will continue to be an effective way to provide an ophthalmology curriculum to medical students, regardless of whether the format is primarily in person or online. | | | References | 1. Shah M, Knoch D, Waxman E. The state of ophthalmology medical student education in the United States and Canada, 2012 through 2013. Ophthalmology 2014;121:1160-3.
2. Rui P, Okeyode T. National Ambulatory Medical Care Survey: 2016 National Summary Tables, 2016. Available at: https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2016_namcs_web_tables.pdf. Accessed June 12, 2020.
3. Succar T, Grigg J, Beaver HA, Lee AG. A systematic review of best practices in teaching ophthalmology to medical students. Surv Ophthalmol 2016;61:83-94.
4. Albert DM, Bartley GB. A proposal to improve ophthalmic education in medical schools. Ophthalmology 2014;121:1157-9.
5. Diel RJ, Avdic A, Kemp PS. Flipped ophthalmology classroom: a better way to teach medical student. J Acad Ophthalmol 2020;12:e104-9.
6. Allen RC, Harper RA, American Academy of Ophthalmology. Basic ophthalmology: essentials for medical students. 10th ed. San Francisco, CA: American Academy of Ophthalmology; 2016.
7. Bandhu SD, Raje S. Experiences with e-learning in ophthalmology. Indian J Ophthalmol 2014;62:792-4.
8. Steedman M, Abouammoh M, Sharma S. Multimedia learning tools for teaching undergraduate ophthalmology: results of a randomized clinical study. Can J Ophthalmol 2012;47:66-71.
9. Krohn J, Kjersem B, Hovding G. Matching fundus photographs of classmates: an informal competition to promote learning and practice of direct ophthalmoscopy among medical students. J Vis Commun Med 2014;37:13-8.
10. Tang F, Chen C, Zhu Y, et al. Comparison between flipped classroom and lecture-based classroom in ophthalmology clerkship. Med Educ Online 2017;22:1395679.
11. Lin Y, Zhu Y, Chen C, et al. Facing the challenges in ophthalmology clerkship teaching: is flipped classroom the answer? PLoS One 2017;12:e0174829.
12. Horne A, Rosdahl J. Teaching clinical ophthalmology: medical student feedback on team case-based versus lecture format. J Surg Educ 2017;74:329-32. | |
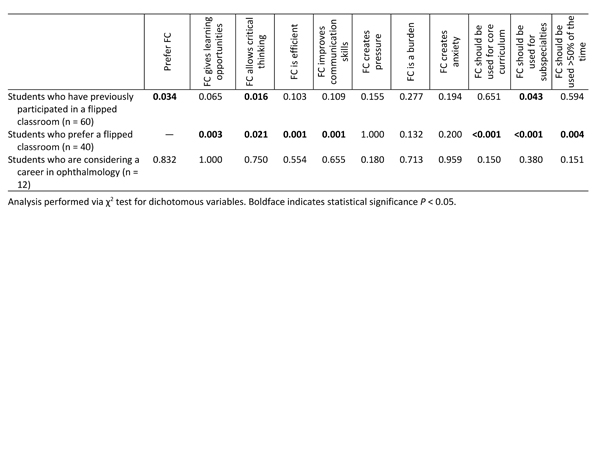
Table 1
Pre-clerkship questionnaire: associations between students’ baseline experiences and opinions regarding the flipped classroom (FC)
|
|
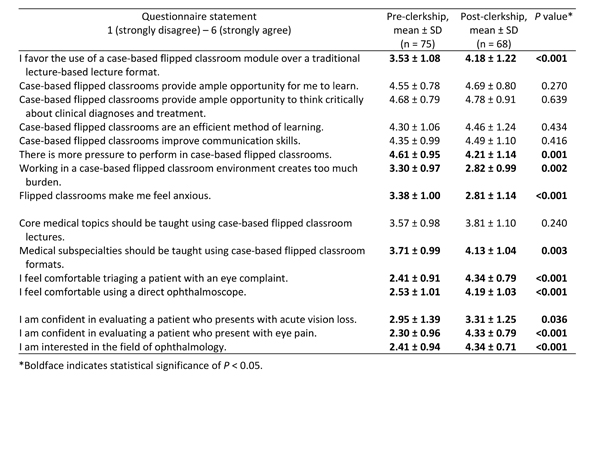
Table 2
Student questionnaire responses before and after completing flipped classroom
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in