|
|
 |
 |
 |
 |
|
|
Factors associated with visual outcome in acute post cataract surgery endophthalmitis – a prospective analytical study
Digital Journal of Ophthalmology 2022
Volume 28, Number 1
February 12, 2022
|
Printer Friendly
Download PDF |


 Tharini Senthamizh, MS (Ophthalmology)
Tharini Senthamizh, MS (Ophthalmology) | Aravind Eye Hospital, Madurai, India Haripriya Aravind, MS (Ophthalmology) | Department of Cataract and IOL services, Aravind Eye Hospital, Madurai, India Tanpreet Pal Singh, MS (Ophthalmology) | Department of Cataract and IOL services, Aravind Eye Hospital, Madurai, India
|
|
|
| Abstract | Purpose
To identify predictors of visual outcome in patients with acute endophthalmitis following cataract surgery.
Methods
This cross-sectional study included consecutive patients with acute endophthalmitis following cataract surgery at our tertiary care center between January 2017 and June 2018. Baseline demographic details, surgical details, and treatment offered were extracted from the medical record, and patients were followed for 3 months after diagnosis and treatment for endophthalmitis. A good outcome was defined as visual acuity of greater than 6/12; a poor outcome, visual acuity of less than 6/60 on 3-month follow-up. The factors associated with these outcomes were analyzed.
Results
A total of 60 patients were included, of whom 32 (53%) had good visual outcome, and 11 (18%) had poor visual outcome. On univariate analysis, factors associated with good outcome were younger age at surgery, male sex, diabetes, absence of hypopyon, and absence of fibrillary membrane over the intraocular lens (IOL). Poor visual acuity at presentation, inability to visualize the optic disc on indirect ophthalmoscopy, and negative microbiological culture were associated with poor visual outcome. Stepwise logistic regression analysis showed that absent hypopyon (OR = 19.50; 95% CI, 2.87-132.14) and absent fibrillary membrane over the IOL (OR =15.0; 95% CI, 2.34-96.89) were independent factors for good visual outcome. Negative microbiological culture (OR = 18.67; 95% CI, 2.32-150.13) was the only independent factor associated with poor visual outcome.
Conclusions
The clinical findings at presentation and microbiological profile play an important role in determining the outcome in patients with acute post-cataract surgery endophthalmitis. | | | Introduction | | The incidence of post-cataract-surgery endophthalmitis ranges from 0.02% to 0.26%.(1) Despite improved sterile precautions, rapid and precise identification of microorganisms, and more advanced treatment modalities, the final outcome of endophthalmitis remains poor. Most studies analyzing the risk factors for visual outcome in endophthalmitis are retrospective.(2,3) Because of epidemiological variations and evolving surgical techniques, newer prospective studies are needed to analyze the predictive factors that can help clinicians to stratify patients for proper treatment. The current study aimed to assess the factors predictive of visual outcomes in patients with acute endophthalmitis following cataract surgery. | | | Materials and Methods | We conducted a cross sectional analytical study at Aravind Eye Hospital, a tertiary eye care center in Madurai, South India, between January 2017 and June 2018. The study adhered to tenets of the Declaration of Helsinki and was approved by the Ethics Committee, Aravind Eye Care system. Consecutive patients who presented with clinical signs and symptoms of acute endophthalmitis within 6 weeks of cataract surgery were included. Those who presented with features of endophthalmitis secondary to other surgical procedures, trauma, endogenous endophthalmitis, toxic anterior segment syndrome, and those with poorly controlled diabetes were excluded. All patients were admitted, and baseline demographic details and surgery details were extracted from the medical records retrospectively. The initial procedures performed were extracapsular cataract extraction (ECCE), small-incision cataract surgery (SICS), and phacoemulsification. The operating surgeons included both trainees and experts.
Patients were treated per the hospital standard treatment protocol and followed for 3 months. Best-corrected visual acuity was tested using the Snellen chart at discharge and the first and third months after diagnosis of endophthalmitis. Visual acuity at 3 months’ follow-up was considered the final visual outcome, and those with visual acuity >6/12 were considered to have a good outcome; those with visual acuity of <6/60 are considered to have a poor outcome. Acute postoperative endophthalmitis was diagnosed based on symptoms, including pain, decreased vision, and signs including lid edema, conjunctival congestion, inflammation of the anterior chamber, hypopyon, fibrillary membrane (FM) over the intraocular lens (IOL), posterior segment inflammation, and ultrasonographic evidence of vitreous inflammation. On admission, patients underwent an immediate diagnostic aqueous tap, vitreous tap, or a primary core vitrectomy, according to surgeon discretion. For patients undergoing vitrectomy, undiluted vitreous samples were collected. All the collected samples were sent for Gram staining and potassium hydroxide (KOH) staining and cultured in blood agar, Sabourad’s agar, thioglycolate broth, and brain heart infusion broth. No transport media was used. Inoculation was performed immediately.
All patients received topical moxifloxacin 5 mg/ml or topical voriconazole (10 mg/ml) for those with suspected fungal infection and intravitreal injection of vancomycin hydrochloride (1 mg/ 0.1ml), ceftazidime (2 mg/0.1 ml), and dexamethasone (0.4 mg / 0.1 ml in selected cases). The intravitreal steroid was avoided in patients with suspected fungal infection. In patients allergic to penicillin, vancomycin hydrochloride (1 mg / 0.1 ml) and amikacin (0.4 mg / 0.1 ml) were used. Based on culture reports, specific antibiotics were administered during repeat intravitreal injection or vitrectomy. Those who worsened with intravitreal antibiotics underwent salvage core vitrectomy.
Continuous variables were recorded as median (range); categorical variables, as a percentage. The association between prognostic factors and the visual outcome was analyzed using the ?2 test for categorical variables and the Mann-Whitney U test for continuous variables. Those factors found to be statistically significant in univariate analysis were analyzed using forward stepwise logistic regression using the likelihood ratio model. A P value of <0.05 was considered statistically significant. SPSS for Windows, version 19.0 (SPSS Inc, IBM, Armonk, NY) was used for all statistical operations. | | | Results | A total of 60 patients (32 females [53%]) were included in our study, with a median age of 64 years and an interquartile range 54-66.5. Although all patients presented within 6 weeks of cataract surgery, almost 55% presented 1-4 weeks after surgery. Of the total, 10 (17%) were diabetic and were taking oral hypoglycemic drugs. Of the 60 patients, 43 patients (72%) underwent manual SICS, 15 (25%) underwent phacoemulsification, and 2 (3%) underwent ECCE. Trainees performed the procedure in 8 cases (13%); the remaining 52 cases (87%) were operated on by expert surgeons. Duration of surgery was noted to be <15 minutes in 44 patients (73%). Intraoperative complications were noted in 13 patients (22%), of whom 6 (10%) had a posterior capsular rupture with vitreous disturbance.
All 13 patients with intraoperative complications received an intracameral injection of moxifloxacin (0.5 mg/0.1 ml) at the conclusion of surgery. On the day of presentation, 3 patients (5%) who underwent SICS had scleral wound infiltration, 5 (8.3%) had corneal wound infiltration, and 2 (3.3%) had melted cornea. 42 (70%) patients presented with hypopyon and 42 (70%) with FM over IOL. Primary core vitrectomy was performed for 7 patients (12%) because of poor media clarity and poor vision at presentation. Culture positivity was noted in 19 patients (32%), in 11 (58%) of whom coagulase-negative staphylococci were found (Figure 1). At 1 month’s follow-up, 27 patients (45%) had visual acuity worse than 6/12, and 15 (25%) had visual acuity worse than 6/60. There was improvement in this trend, with 31 (52%) having visual acuity better than 6/12 and 12 (20%) having visual acuity of worse than 6/60 at 3 months (Figure 2). A total of 18 patients (30%) patients had complications at 3 months, including phthisis, optic capture of IOL, with fibrous posterior capsular opacification and secondary glaucoma, of which 3 patients (17%) had FM over IOL at initial presentation.
On univariate analysis, significant factors associated with good outcome were younger age, male sex, diabetes, absence of hypopyon, and absence of FM over IOL. Visual acuity at presentation of <6/60, inability to visualize the fundus on indirect ophthalmoscopy, and negative microbiological culture were associated with poor outcome. There was no significant difference in outcome between the three cataract surgery groups (P = 1.000 [?2 test]). And none of the treatment modalities showed any significant association in univariate analysis (Table 1). Stepwise logistic regression (Tables 2 and 3) analysis showed that absent hypopyon (OR = 19.50; 95% CI, 2.87-132.14), and absent FM over IOL (OR = 15.0; 95% CI, 2.34-96.89) were significantly associated with good visual outcome, whereas diabetes had an inverse association with good visual outcome (OR = 0.035; 95% CI, 0.004-0.336). On the other hand, we found that negative microbiological culture (OR = 18.67; 95% CI, 2.32-150.13) was the only independent factor significantly associated with poor visual outcome. | |
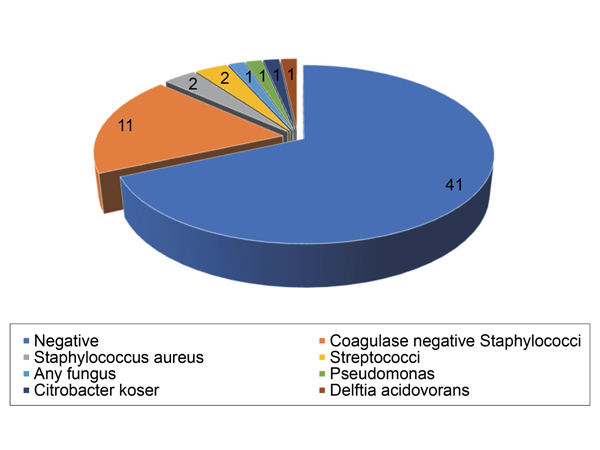
Figure 1.
Microorganisms isolated from vitreous culture (n = 60).
|
|
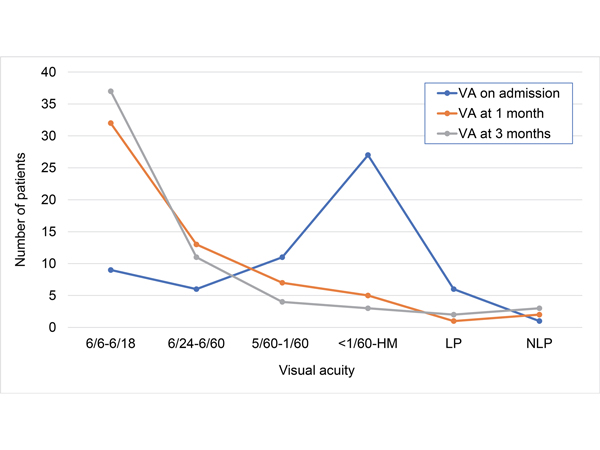
Figure 2.
Visual acuity trend during admission and at subsequent follow-up examinations.
|
|
| Discussion | Endophthalmitis is a rare but vision-threatening complication of cataract surgery. Of the different types of postoperative endophthalmitis, acute endophthalmitis accounts for most cases (88%) that occur within 6 weeks of surgery. The reported incidence is 0.1%.(4-6) Despite the advances in diagnostic techniques and treatment modalities, only around 28%-53% have obtained visual acuity of better than 6/12, as reported in various studies.(7-10) The Endophthalmitis Vitrectomy Study (EVS) reported that 15% of patients had a final visual acuity of 6/60.(11) In our study cohort, 32 patients (53%) had with a final vision of more than 6/12 and 11 (18.3%) patients with a visual acuity of worse than 6/60.
In our study, 42 patients (70%) presented with hypopyon. A study by Lalwani et al reported a higher proportion of (82%) patients presenting with hypopyon.(12) In a study by J-H Cheng et al, the presence of hypopyon was associated with worse outcome, and its presence signified infection with a fulminant organism and wound abnormalities.(13) We had 8 patients (13%) with wound infiltrate, but none of our patients had a wound leak. Only 2 patients (5%) in our study who presented with hypopyon had associated infection with virulent organisms. One with Staphylococcus aureus infection presented with a 3 mm hypopyon and suture abscess, and the final outcome for this patient was poor, with visual acuity of 1/60 at 3 months’ follow-up. Another patient with pseudomonas infection presented with corneal melt, which ultimately resulted in phthisis. The absence of hypopyon was independently associated with good visual outcomes in this study. The chance of a good outcome was 19 times higher in patients without hypopyon than in those present with hypopyon.
The presence of FM over IOL signifies severe infection leading to a breakdown of the blood-ocular barrier and disruption of coagulative and fibrinolytic pathways.(14) Also, the FM can lead to further ocular morbidities, such as posterior synechiae, pupillary block, and secondary angle-closure glaucoma, which can further worsen the visual outcome in patients with endophthalmitis.(15) In our study, absence of FM over IOL was associated with a 15 times higher chance of good visual outcome. We had 42 patients (70%) with FM over IOL as the initial clinical picture.
People with diabetes are known to have an impaired immune response and are prone to surgical infections. An exploratory analysis of the EVS study reported that 55% of patients without diabetes achieved visual acuity of at least 6/12 compared with 39% of diabetic patients.(16) In our study, 30 patients (60%) without diabetes achieved visual acuity of more than 6/12 compared with 2 patients (20%) with diabetes. Yet our analysis revealed an inverse association of diabetes with good outcome, probably because all diabetic patients included in our study had good glycemic control, and their presenting vision was also good. All patients who presented with a visual acuity of light perception or worse in our study were nondiabetic.
Identifying the causative organisms in infectious endophthalmitis plays a major role in deciding the treatment and visual outcome. Most previous studies reported less than half of patients with positive cultures, ranging from 38%-44%.(17,18) In our cohort there were 41 (68%) culture-negative cases and only 19 (31.7%) culture-positive cases. The negative microbiological culture was the only independent predictive factor of poor visual outcome in our study. This may be explained by the fact that the organisms may be multidrug-resistant or fastidious and difficult to grow in routine culture.
Negative cultures do not rule out infectious cause; this had been proved in studies using molecular tools, such as polymerase chain reaction and Next Generation Sequencing, to show the presence of organisms in 14 (73%) culture-negative cases.(19,20) Clinicians should be vigilant in treating culture-negative cases and consider an immediate change in treatment modality if the response to regular treatment is static or poor.
The limitations of our study include a small sample size composed of a homogenous population and restriction to conventional culture methods to identify the causative organisms. Further prospective studies with a larger sample size would be helpful in confirming our results.
In conclusion, the absence of both hypopyon and FM over the IOL is significantly related to good visual outcomes. Also, diabetic patients with good glycemic control can have good visual outcomes comparable with nondiabetic patients. This result cannot be generalized, however, and we recommend future studies to investigate in detail the relationship between glycemic control and visual outcome in endophthalmitis. Negative culture in endophthalmitis does not necessarily mean absence of infecting organism, and newer methods can be adapted to identify the causative organism. More aggressive treatment might be needed in such cases to prevent poor visual outcomes even if the organism is not identifed. | | | References | 1. Lalitha P, Sengupta S, Ravindran RD, et al. A literature review and update on the incidence and microbiology spectrum of post cataract surgery endophthalmitis over past two decades in India. Indian J Ophthalmol 2017;65:673-7.
2. Yospaiboon Y, Intarapanich A, Laovirojjanakul W, et al. Factors affecting visual outcomes after treatment of infectious endophthalmitis in northeastern Thailand. Clin Ophthalmol 2018;12:765-72.
3. Jeong SH, Cho HJ, Kim HS, et al. Acute endophthalmitis after cataract surgery: 164 consecutive cases treated at a referral center in South Korea. Eye (Lond) 2017:1456-62.
4. Keay L, Gower EW, Cassard SD, Tielsch JM, Schein OD. Postcataract surgery endophthalmitis in the United States: Analysis of the complete 2003 to 2004 Medicare database of cataract surgeries. Ophthalmology 2012;119:914-22.
5. Olson Jc, Flynn HW, Forster RK, Culbertson WW. Results in the treatment of postoperative endophthalmitis. Ophthalmology 1983;90:692-9.
6. Jambulingam M, Parameswaran SK, Lysa S, Selvaraj M, Madhavan HM. A study on the incidence, microbiological analysis, and investigations on the source of infection of postoperative infectious endophthalmitis in a tertiary care ophthalmic hospital: an 8-year study. Indian J Ophthalmol 2010;58:297-302.
7. Kim HW, Kim SY, Chung IY, et al. Emergence of Enterococcus species in the infectious microorganisms cultured from patients with endophthalmitis in South Korea. Infection 2014;42:113-8.
8. Eifrig CW, Flynn Jr HW, Scott IU, Newton J. Acute-onset postoperative endophthalmitis: review of incidence and visual outcomes (1995-2001). Ophthalmic Surg Lasers 2002;33:373-8.
9. Lertsumitkul S, Myers PC, O’Rourke MT, Chandra J. Endophthalmitis in the western Sydney region: a case-control study. Clin Exp Ophthalmol 2001;29:400-5.
10. Friling E, Lundstrom M, Stenevi U, Montan P. Six-year incidence of endophthalmitis after cataract surgery: Swedish national study. J Cataract Refract Surg 2013;39:15-21.
11. Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study: a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol 1995;113:1479-96.
12. Lalwani GA, Flynn HW, Scott IU, et al. Acute-onset endophthalmitis after clear corneal cataract surgery (1996–2005): clinical features, causative organisms, and visual acuity outcomes. Ophthalmology 2008;115:473-6.
13. Cheng J-H, Chang Y-H, Chen C-L, et al. Acute endophthalmitis after cataract surgery at a referral center in Northern Taiwan: review of the causative organisms, antibiotic susceptibility, and clinical features. Eye (Lond) 2010;24:1359-65.
14. Mehta JS, Adams GG. Recombinant tissue plasminogen activator following paediatric cataract surgery. Br J Ophthalmol 2000;84:983-6.
15. Wu T, Wang H. Intracameral recombinant tissue plasminogen activator for the treatment of severe fibrin reaction in endophthalmitis. Eye 2009;23:101-7.
16. Doft BH, Wisniewski SR, Kelsey SF, Groer-Fitzgerald S; Endophthalmitis Vitrectomy Study Group. Diabetes and postcataract extraction endophthalmitis. Curr Opin Ophthalmol 2002;13:147-51.
17. Anand AR, Therese L, Madhavan HN. Spectrum of etiological agent of postoperative endophthalmitis and antibiotic susceptibility of bacterial isolates. Indian J Ophthalmol 2000;48:123-8.
18. Kunimoto DY, Das T, Sharma S, et al. Microbiologic spectrum and susceptibility of isolates: Part I. Postoperative endophthalmitis. Am J Ophthalmol 1999;128:240-2.
19. Chiquet C, Lina G, Benito Y, et al. Polymerase chain reaction identification in aqueous humor of patients with postoperative endophthalmitis. J Cataract Refract Surg 2007;33:635?41.
20. Deshmukh D, Joseph J, Chakrabarti M, et al. New insights into culture negative endophthalmitis by unbiased next generation sequencing. Sci Rep 2019;9:844. | |
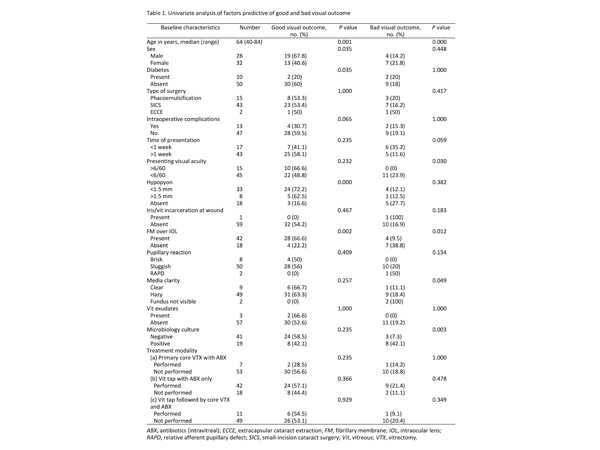
Table 1.
Univariate analysis of factors predictive of good and bad visual outcome
|
|
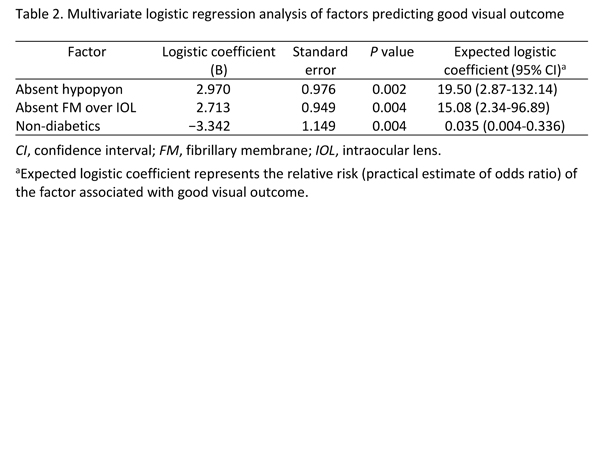
Table 2.
Multivariate logistic regression analysis of factors predicting good visual outcome
|
|
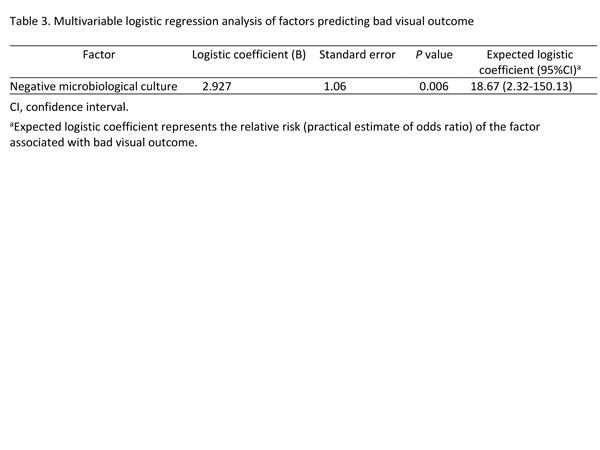
Table 3.
Multivariable logistic regression analysis of factors predicting bad visual outcome
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in