|
|
 |
 |
 |
 |
|
|
A Review of Optic Neuritis
Digital Journal of Ophthalmology 1997
Volume 3, Number 4
May 1, 1997
|
Printer Friendly
|



Ken Graham, M.D. | Massachusetts Eye and Ear Infirmary, Harvard Medical School Joseph Rizzo, M.D. | Massachusetts Eye and Ear Infirmary, Harvard Medical School
|
|
|
| Abstract | Objective
Optic neuritis is inflammation of the optic nerve. The cause of the inflammation and the most appropriate treatment is a subject of debate. This article will review a typical case of optic neuritis, the clinicalmanifestations of optic neuritis, and the findings of the Optic Neuritis Treatment Trial. | | | Introduction | Optic neuritis is a serious condition which typically involves theyoung adult population. Years ago it was thought that one third ofoptic neuritis patients would go on to have neurological symptoms frommultiple sclerosis (MS). More recent long term studies indicate that over decades the risk of developing MS is much higher.(1) Ophthalmologists must be alert to the symptoms of optic neuritis andthey must be aware of the more serious complications to which these symptoms are linked
CASE PRESENTATION
A 30 year old caucasian man presented with 2 weeks of gradually worsening vision in his left eye.
History of present illness:
The patient had been seen once by a neurologist 2 years previously for flashes. At that time a head CT was normal. The patient was lost to follow up with the neurologist, but the flashes had continued for the 2 year period. The patient has a history of color blindness. The patient also reported posterior pressure and tightness with left eye movement for the past week. The patient reported his vision in the left eye worsened when showering. The patient did not experience visual changes with activity or movement. Patient denied a history of trauma, redness, discharge or headache.
Past medical history: negative
Social history: negative
Medications: none
No known drug allergies
Examination:
The exam revealed a vision of 20/20 OD and 20/30 OS. The patient was only able to get the control plate correct on the color plates in both eyes consistent with his history of color blindness. The external exam revealed no ptosis, and no resistance to retropulsion. His pupils were reactive to light, changing FROM 4 to 2mm symmetrically. There was a left afferent pupillary defect. Hertel measurement with a base of 102 was 19 OD and 18 OS. Extraocular movements were full OU, though the patient reported a "tight" feeling on OS abduction. Tension was 15 OU. Slit lamp exam was normal OU. Dilated exam was normal OU with no disc edema. Humphrey visual fields showed an inferior altitudinal defect OS ( Fig 1and 2).
One week follow up:
The patient reported continued decreasing vision OS. The exam revealed visual acuity of 20/20 OD and 20/400 OS. The OS afferent pupillary defect remained. The rest of the exam was the same. Goldmann visual fields were done and showed a central scotoma OS (slide 3).
A MRI was done at this time and showed inflammation of the left optic nerve (slide 4), and white matter hyperintensity of the left occipital (slide 5) and right frontal(slide 6) lobes. Possible treatment with corticosteroids was discussed with the patient. He chose to be observed with no corticosteroid treatment.
One month follow up:
The patient reported marked recovery of vision OS, but had some blurring in bright sunlight. The patient was on no medications. His vision was 20/20 OU. There was no afferent pupillary defect and no "tightness" on eye movement. The rest of the exam was unchanged. A Humphrey visual field showed improvement in the central scotoma . | | | Discussion | CLINICAL MANIFESTATION
Optic neuritis typically presents with a triad of symptoms: loss of vision, dyschromatopsia and eye pain. The initial attack is unilateral in 70% of adult patients and bilateral in 30%. The mean age of onset of optic neuritis is in the third decade of life, but can occur FROM the first to the seventh decades. The annual incidence of optic neuritis ranges FROM 1.4 to 6.4 new cases per 100,000 population. (2,3) Associated visual symptoms are reduced perception of light intensity and Uhthoff's symptom (visual deficit induced by exercise or increased body temperature).(4)
The visual loss may be subtle or profound. Complete loss of vision may be caused by a single plaque. In some cases the vision may be 20/20 with the only symptoms being blurred vision on exertion or other isolated symptoms.(5) The rate of visual decline varies. Visual loss may occur over hours (rarely) to days (most commonly). The nadir is usually about 1 week after the onset.(6)
The prognosis for visual recovery is usually good. The majority of patients (65-80%) recover visual acuity of 20/30 or better.(7,8) Most cases will recover visual acuity in a few months, although the patients will often report some residual visual defect. There have been reported residual abnormalities in contrast sensitivity, color vision, visual field loss, and light brightness.(9-12)
In a patient with optic neuritis, the vision may improve, but the risk for development of multiple sclerosis is high. This risk does not decrease over time.(1) In the past a number of patients have been treated with oral or intravenous corticosteroids in the hope of improving visual recovery and decreasing the incidence of multiple sclerosis. To help resolve the controversy of corticosteroids, the Optic Neuritis Treatment Trial was formed.
OPTIC NEURITIS TREATMENT TRIAL
The Optic Neuritis Treatment Trial (ONTT) was a multicenter study in which 389 patients with acute optic neuritis were randomly assigned to one of three treatment groups. The first GROUP was given oral prednisone (1 mg/kg daily) for 14 days. The second GROUP was given intravenous methylprednisolone, 250 mg four times daily for three days, followed by oral prednisone for 14 days. The third GROUP was given an oral placebo for 14 days.
The eligibility criteria for the ONTT selected for patients with typical clinical features of optic neuritis. These criteria were: age range of 18 to 46 years; acute unilateral optic neuritis with visual symptoms of 8 days or less; a relative afferent pupillary defect and a visual field defect in the affected eye; no previous episodes of optic neuritis in the affected eye; no previous corticosteroid treatment for optic neuritis or multiple sclerosis; and no systemic disease other than multiple sclerosis that might be associated with optic neuritis.(13)
All patients in the ONTT had blood testing to exclude collagen vascular disease (antinuclear antibody), syphilis (FTA-ABS), and a chest x-ray to detect sarcoidosis. A lumbar puncture was optional and was performed in 141 patients. Antinuclear antibody was positive in a titer 1:320 or greater in 3% of patients. Of these patients, only one developed a connective tissue disease in the first two years of follow up. FTA-ABS was positive in 1.3% of the patients, and none were judged to have syphilis. A chest x-ray did not SHOW evidence of sarcoidosis in any patients. CSF analysis never yielded unsuspected information. Based on these results, chest x-ray, blood tests, and lumbar puncture are deemed not to be necessary in evaluating patients with typical clinical features of optic neuritis.
The efficacy of corticosteroid therapy in optic neuritis has been controversial. The ONTT showed that intravenous methylprednisolone followed by oral prednisone speeds the recovery of visual loss, but there were no significant differences in visual acuity comparing the three groups at 6 months. Unexpectedly, oral prednisone was found to increase the risk of recurrent optic neuritis. Thus, treatment with oral prednisone in standard doses is no longer advised.
The ONTT also evaluated the relationship between optic neuritis and multiple sclerosis. A standardized detailed neurologic examination was performed at study entry, at 6 months, at 1 year and then yearly. Clinically definite multiple sclerosis was diagnosed when new neurologic symptoms developed that were attributable to demyelination in one or more regions of the central nervous system. Treatment with the intravenous followed by oral corticosteroid regimen reduced the rate of development of MS during the first 2 years. This was particularly evident in patients with three or more brain MRI signal abnormalities consistent with demyelination in locations characteristic of MS. By 3 years, this treatment effect had subsided.
The ONTT therefore recommends obtaining a brain MRI to assess the risk of developing MS. The MRI is used to assist in the decision of whether to use IV steroids. It is unknown if repeat IV steroids at 2 years would continue to affect the rate of development of MS. Other prospective studies using beta interferon are currently in progress.(14) | | | References | 1. Rizzo JF, Lessell S: Risk of developing multiple sclerosis after uncomplicated optic neuritis: A long term prospective study. Neurology 38:185-190, 1988.
2. Brewis M, Poskanzer DC, Rolland C, et al: Neurological disease in an English city. Acta Neurol Scand 42 (Suppl 24):1, 1965.
3. Wray SH: Optic Neuritis. Principles and Practice of Ophthalmology. Volume 4, 2539-2568.
4. Percy AK, Nobrega FT, Kurland LT: Optic neuritis and multiple sclerosis. Arch Ophthalmol 87:135,1972.
5. Nikoskelainen E: Symptoms, signs and early course of optic neuritis. Acta Ophthalmol 53:254, 1975.
6. Lillie WI: The clinical significance of retrobulbar and optic neuritis. Am J Ophtahlmol 17:110, 1934.
7. Perkin GD, Rose CF: Optic Neuritis and its Differential Diagnosis. Oxford, Oxford University Press, 1979, p 206.
8. Celesia GG, Kaufman DI, Brigell M, et al: Optic neuritis: A prospective study. Neurology 40:919, 1990.
9. Sanders EACM, Volkers ACW, van der Poel JC, et al: Estimation of visual function after optic neuritis: A comparison of clinical tests. Br J Ophthalmol 70:918, 1986.
10. Griffin JF, Wray SH: Acquired color vision defects in retrobulbar neuritis. Am J Ophthalmol 86:193, 1978.
11. Van Dalen JTW, Greve EL: Visual field defects in multiple sclerosis. Neuro-ophthalmology 2:93, 1981.
12. Hess RF, Plant GT: The psychophysical loss in optic neuritis: spatial and temporal aspects. In Optic Neuritis. Cambridge, Cambridge University Press, 1986, p 109.
13. Beck RW, Cleary PA, et al: Optic Neuritis Treatment Trial. Arch Ophthalmol 3:773-775, 1993.
14. Beck RW, Trobe JD: What we have learned FROM the Optic Neuritis Treatment Trial. Ophthalmology 10:1504-1509, 1995. | | | Clinical Pictures | | | |

Figure 1
Humphrey visual field OD.
|
|

Figure 2
Humphrey visual field OS
|
|
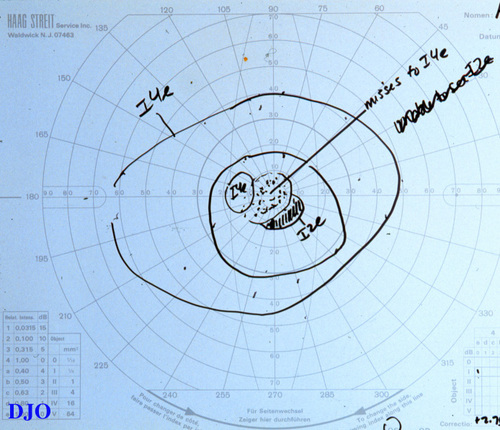
Figure 3
Goldmann Visual Field OS
|
|
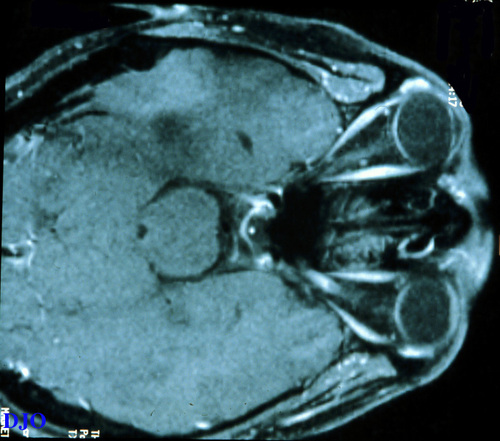
Figure 4
MRI demonstrating optic nerve white matter hyperintensity
|
|
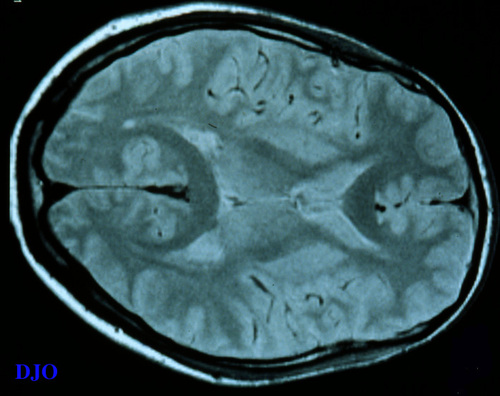
Figure 5
MRI demonstrating left occipital lobe hyperintensity
|
|
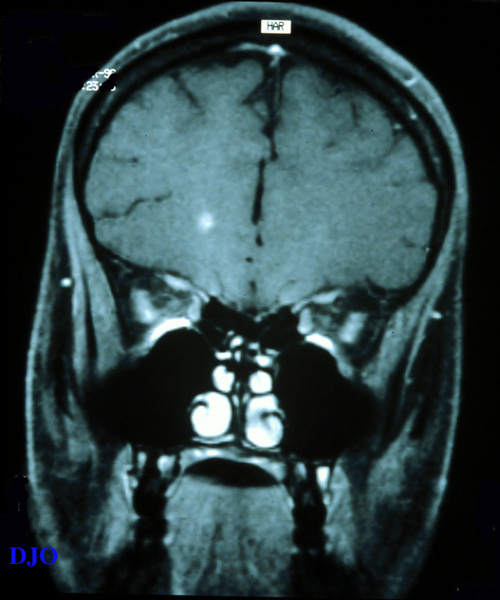
Figure 6
MRI demonstrating right frontal lobe hyperintensity
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in