|
|
 |
 |
 |
 |
|
|
Recurrent Orbital Retinoblastoma After Enucleation
Digital Journal of Ophthalmology 1997
Volume 3, Number 7
July 30, 1997
|
Printer Friendly
|



Carlo R. Bernardino | Thomas Jefferson Medical School Peter A.D. Rubin, M.D. | , Massachusetts Eye and Ear Infirmary, Harvard Medical School
|
|
|
| Abstract | Objective
This is a case presentation of a 3 year old boy who presented with orbital recurrence of retinoblastoma after enucleation and limited radiation therapy. Following the case presentation, a review of therapeutic modalities for retinoblastoma will be discussed, with particular focus on enucleation and the management of recurrence of tumor in the globe. | | | Introduction | | Chief Complaint: A 3 year old Honduran boy presented with a forty day history of increasing swelling of the lids, irritation, itchiness, and inflammation of the right orbit. The patient also had a fever. The patient had an enucleation of the right eye six months ago for ocular retinoblastoma. | | | Materials and Methods | Past Ocular History:
12/89 A physician in Honduras noted leukocoria of the right eye. A white lesion was observed in the anterior segment OD, that later filled the entire anterior chamber.
Six months later, the patient underwent enucleation of the right eye. Pathological diagnosis was retinoblastoma, which was present up to the surgical margin of the optic nerve.
One month after initial surgery, the patient received Cobalt 60 irradiation to the right orbit. However, the patient's family refused complete treatment, and the patient received only 10 Gy in five sessions. The patient's family also refused adjuvant systemic chemotherapy. Past Medical History: not contributory.
Physical Exam:
Visual Acuity: The patient had 23/30 vision by Allen-Card pictures, OS.
Extraocular muscles had full range of motion, OS.
Pupil was round and reactive to light, OS.
Hertel: A large proptotic mass was noted protruding FROM the right orbit, spreading the eyelids apart.
SLE: unremarkable, OS
Fundus: No tumor was visualized, OS.
Studies: CT of the orbits disclosed a 6 x 4 x 5 cm mass with small foci of calcification. The mass grew along the optic nerve stopping at the orbital apex. However, the optic nerve in the optic canal was not enlarged. The mass also engulfed the medial and inferior rectus muscles. CT of the head disclosed normal gray and white matter and no signs of intracranial masses.
A systemic metastatic examination including a lumbar puncture, body CT, and bone marrow biopsies disclosed no tumor involvement.
Admission History:
Six months after the initial enucleation, the patient was admitted for an exam under anesthesia and exenteration of the right orbit. The EUA did not disclose any tumor in the left eye. An exenteration of the right orbit was performed, and frozen sections of cutaneous and periosteal margins were sent perioperatively. All frozen section biopsies were negative for tumor. The exenteration was completed without any complications. The entire specimen was sent for pathologic evaluation.
Pathological Report:
The exenteration specimen measured 67 x 53 x 19 mm. Grossly it had edematous and erythematous eyelids. A large tumor invaded the connective tissue and muscle, and extended to the superior surgical margin. The tumor was not encapsulated, and it obliterated the lateral fornix. Histopathological examination disclosed an undifferentiated recurrent retinoblastoma.
All periosteal and cutaneous biopsies of the surgical margins were negative for tumor.
Post-hospitalization Course:
The orbit was allowed to granulate, and the patient was followed closely. Examination of the left eye showed no evidence of tumor.
Due to the large size of the tumor and the extension of the tumor to the superior surgical margin, radiation therapy was commenced one month postoperatively.
Four months later, the patient developed metastasis to the left mandible and left femur and was started on systemic chemotherapy. However, no orbital recurrence was noted. Subsequently, the patient required palliative radiation for metastatic bone pain.
No further documentation was available on the patient's course, but it was reported that the patient passed away due to metastatic disease. | |

Figure 1
Clinical photo of the patient six months after enucleation.
|
|
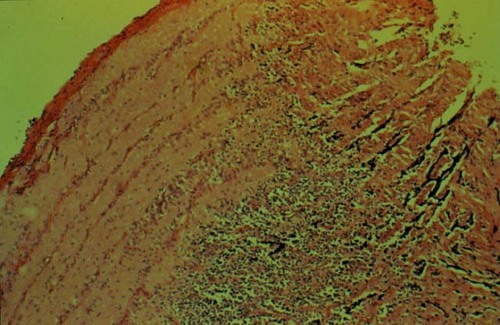
Figure 2
Pathologic specimen of the patient's optic nerve showing the surgical margin of optic nerve positive for retinoblastoma.
|
|
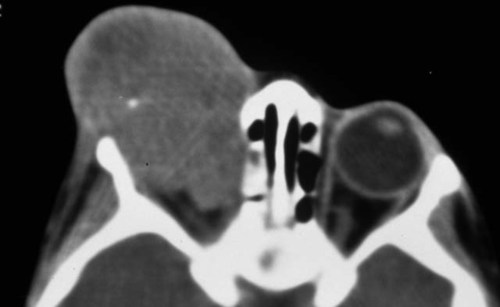
Figure 3
Orbital CT disclosing soft tissue with calcification
|
|
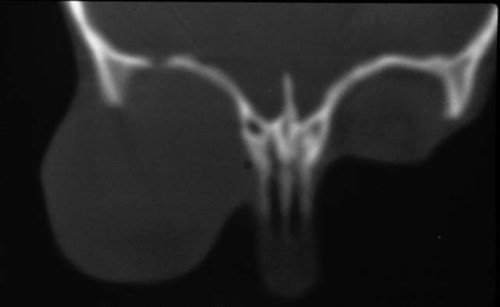
Figure 4
Orbital CT of the bone window shows superior temporal erosion.The superior temporal region of the right orbital roof showed focal areas of thinning, without overt bony destruction.
|
|

Figure 5
Intraoperative photo shows bony defect of superior temporal orbit. This correlates with the erosion in figure #4.
|
|

Figure 6
Photo of orbit shows postoperative granulation.
|
|
| Discussion | Retinoblastoma is the most common intraocular malignant neoplasm of childhood affecting 1:20,000 to 1:34,000 children (1). Although most retinoblastomas are unilateral, up to 25% of sporadic cases and most inherited retinoblastomas are bilateral. Management of these tumors includes photocoagulation, cryosurgery, cobalt plaques, external beam radiation, and less often diathermy. These various modalities will not be discussed below. However, the goals of treatment should be to maintain life, to retain the eye, to preserve vision, and to facilitate good cosmetic results (2).
More invasive modalities include enucleation and exenteration. The decision to enucleate a globe is based on a clinical assessment, whether the disease is too far advanced to salvage useful vision in the affected eye, or when other treatments have failed. If the tumor affects two thirds of the retina, if optic nerve invasion is evident, or if extension to the ciliary body is present, enucleation is warranted (3).
When an eye surgeon decides to enucleate a globe, special care must be taken not to spread tumor INTO the orbit during surgery and to obtain a long section of optic nerve. Traction sutures through the severed medial and lateral rectus insertions (4) or a hemostat applied to the medial rectus stump (5) can be used to pull the globe anteriorly. Long enucleation scissors with a lesser curvature should be pressed along the orbit to extract a section of optic nerve larger than 15 mm. A standard lateral canthotomy can facilitate enucleation in a tight orbit (5). The use of clamps or snares on the nerve is discouraged as they can leave crush artifact.
Exenteration is the removal of all orbital structures including lids, eyes, extraocular muscles, nerves and orbital fat. In the past exenteration was a primary treatment modality for ocular retinoblastoma. However it is now reserved for treatment of a primary orbital mass or orbital recurrence of retinoblastoma (4).
Orbital retinoblastoma can present with proptosis, a palpable orbital mass, or lid swelling with echymosis. Sometimes the extrusion of a prosthesis may be the presenting sign (6). Radiologic evidence of an enlarged optic canal may signify central nervous system extension, even if a proptotic mass is not present (7).
In the treatment of orbital retinoblastoma, exenteration, local irradiation and systemic chemotherapy can be used, historically alone, and more recently in combination. In a study by Rootman et al, they found that in their population of patients with orbital retinoblastoma, 5% survived when treated with exenteration alone, while 38% survived with adjuvant chemotherapy (6). In another study by Ellsworth, the `cure' rate of retinoblastoma with exenteration and local irradiation was 30.9% versus 9% with exenteration alone (7). Hungerford et al describes a case series of 16 children with orbital recurrence of retinoblastoma in which not a single child survived when treated with exenteration or radiation alone (8). However, they had one long term survivor who was treated with radiation and systemic chemotherapy.
All the studies agree that local radiation and systemic chemotherapy in conjunction with exenteration or excisional biopsy are effective in decreasing the mortality in orbital retinoblastoma. Exenteration alone may not be effective in removing all the recurrent tumor, but in combination with radiation may affect a more complete local cure (9). The role of chemotherapy is to treat any microscopic systemic metastasis. However, the effects of changing the ORDER of combination treatment should be investigated. In certain tumors elsewhere in the body, preoperative radiation is used to decrease the tumor mass before surgery. Orbital retinoblastoma may be sensitive to this.
In a recent case series, Goble et al demonstrated the effectiveness of aggressive combination therapy; they presented a series of five children with long term survival after treatment with excisional biopsy of tumor, radiation, and systemic chemotherapy (9). They conclude that aggressive therapy for orbital retinoblastoma should include local surgical biopsy, radical orbital radiotherapy, and systemic chemotherapy.
In conclusion, when a child presents with ocular retinoblastoma, one has to first decide if the affected eye can be saved with the non-invasive procedures listed above. If however, the eye cannot be saved, then careful enucleation with extraction of a long optic nerve sample is advisable. If after careful enucleation, the surgical margin of the optic nerve is positive, or if an orbital recurrence is present, surgical removal of any tumor mass with local irradiation and system chemotherapy is the treatment of choice.
In review of our case presentation, it is hard to comment on the enucleation that took place. It is unknown whether the optic nerve was extracted with as much length as possible. Nevertheless, the patient certainly should have completed his course of initial radiation. When the patient presented with a large proptotic mass, the combination therapy of exenteration, radiation, and chemotherapy was appropriate. Unfortunately, the patient succumbed to a disease which still has a high mortality rate even with aggressive treatment. | | | References | 1) Klintworth, GK. The Eye. In: Rubin, E, Farber, JL, ed. Pathology. Philadelphia: J. B. Lippincott, Chapter 29,1994: 1480-1482.
2) Abramson, DH. Treatment of Retinoblastoma. In: Blodi, FC, ed. Contemporary Issues in Ophthalmology, Vol. 2, retinoblastoma. New York: Churchill Livingstone; Chapter 4, 1985: 63-93.
3) Shields, JA, Shields, CL, DePotter P. Enucleation Technique for Children with Retinoblastoma. Journal of Pediatric Ophthalmology & Strabismus. 1992; 29, 4:213-215.
4) Abramson, DH, Ellsworth, RM. The Surgical Management of Retinoblastoma. Ophthalmic Surgery. 1980; 11, 9: 596-598.
5) Shields, JA. Misconceptions and Techniques in the Management of Retinoblastoma. Retina. 1992; 12, 4: 320-329.
6) Rootman, J, Ellsworth, RM, Hofbauer, J, and Kitchen, D. Orbital Extension of Retinoblastoma: A Clinicopathological Study. Canadian Journal of Ophthalmology. 1978; 13:72-78.
7) Ellsworth, RM. Orbital Retinoblastoma. Transactions of the American Ophthalmologic Society. 1974; 62: 79-88.
8) Hungerford, JL, Kingston, JE, and Plowman, PN. Orbital Recurrence of Retinoblastoma. Ophthalmic Paediatrics and Genetics. 1987; 1: 63-68.
9) Goble, RR, McKenzie, J, Kingston, JE, Plowman, PN, Hungerford, JL. Orbital Recurrence of Retinoblastoma Successfully Treated by Combined Therapy. British Journal of Ophthalmology. 1990; 74: 97-98. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in