|
|
 |
 |
 |
 |
|
|
Exudative Neuroretinopathy and Coats'-like Response in Progressive Hemifacial Atrophy
Digital Journal of Ophthalmology 1997
Volume 3, Number 8
November 1, 1997
|
Printer Friendly
|



Anastasios John Kanellopoulos, MD | Massachusetts Eye and Ear Infirmary, Harvard Medical School, State University of New York at Stony Brook Fadi Z. El Baba, MD | Massachusetts Eye and Ear Infirmary, Harvard Medical School Leslie A. Bruce-Lyle, MD | University of California Thomas A. Ciulla, MD | Ophthalmic Consultants of Boston
|
|
|
| Abstract | Objective
Progressive hemifacial atrophy (also known as Parry-Romberg syndrome (PRS)), can be associated with ophthalmic manifestations that involve mainly the ipsilateral orbit, adnexae and intraocular structures. We present a patient with typical progressive hemifacial atrophy who demonstrated unusual posterior segment findings Results
This patient with progressive hemifacial atrophy developed a combination of exudative neuroretinopathy and optic nerve dysfunction resulting in visual loss Thorough ophthalmologic examination in patients with progressive hemifacial atrophy (PRS) is essential. | | | Discussion | A rare acquired progressive hemifacial atrophy that develops in the first decade of life, progresses rapidly, and may stabilize at any age is known as Parry-Romberg syndrome (PRS). It affects women more than men, and has unknown etiology 1.
A 27 year old Hispanic woman was referred with a history of loss of vision in the left eye of undetermined duration. She had no known medical problems, her past medical history was contributory only for left hemifacial atrophy that was first noted during her first decade of life. She denied any family history of similar problems and her social history was non-contributory as well. Examination revealed hemiatrophy of the left facial structures, alopecia of the left temporal skull and madarosis of the temporal aspect of the left eyebrow [Figures 1,2]. Ophthalmic examination of the right eye was normal. Visual acuity was 20/20 in the right eye without correction, and 20/70 in the left eye not improved with refraction.The intraocular pressures were normal. In the left eye, abnormalities included an irregular pupil that was enlarged to 6 mm in diameter which reacted sluggishly to light. An afferent pupil defect was present.The anterior chamber revealed a mild cellular reaction with posterior synechiae FROM the pupilary border to the crystalline lens.There were also trace cells in the anterior vitreous. On funduscopy, the optic nerve disc was flat with peripapillary atrophy of the retinal pigment epithelium and underlying choriocapillaris. Subretinal exudation and lipid deposition in a Coats' like response, were present over the nasal peripapillary retina, and inferiorly beyond the inferotemporal vascular arcade. Diffuse retinal pigment epithelial atrophy was noted inferiorly with areas of subretinal fibrosis, and vascular sheathing [Figures 3-7]. Fluorescein angiography revealed large areas of retinal pigment epithelial window defects, late staining in the area of subretinal fibrosis, and no staining of the optic nerve, or active vascular leakage [Figure 8].
Goldman perimetry was normal in the right eye and revealed a superior altitudinal defect in the left eye. Imaging evaluation included computed tomography of the head and brain, and X ray studies of the head that were normal, with the exception of enophthalmos on the left side. Laboratory evaluation included a normal blood count, serum electrolytes and urinalysis. AntiDNA antibodies, and other antinuclear antibodies were negative. Right and left supraorbital nerve conduction was of normal latency. Punch biopsy of the left hairline revealed only mild dermal fibrosis.
Ocular abnormalities with PRS, are reported in 15-40 % of patients. Enophthalmos, eyelid changes, madarosis, extraocular muscle imbalance, scleral melting, pupillary abnormalities, iris atrophy and uveitis have been encountered 1-3. Uveitis, retinal vasculitis, optic nerve swelling, stellate neuroretinopathy, have been previously described 4,5 Fundus changes include retinal striae, retinal telangiectasia and exudative retinal detachment simulating Coats' syndrome, and other chorioretinal abnormalities 1-3. Dysfunction of the autonomic nervous system, irritative neurotrophic disturbances related to trauma have been suggested as etiologies for PRS 1-5.
Our patient had hemifacial atrophy with onset at early age and slow progression. Linear scleroderma or "en coup de sabre", a circumscribed form of scleroderma, is a major clinical entity in the differential diagnosis of PRS. This was ruled out by the absence of marked dermal sclerosis on scalp biopsy, the lack of prolonged nerve conduction and the negative antinuclear antibody titers.
The posterior segment manifestations in this patient consisted of ipsilateral neuroretinopathy and diffuse exudative retinal changes, that had already led to optic nerve dysfunction and visual loss. These manifestations have been previously described in patients with PRS 4,5. Subretinal fibrosis and retinal pigment epithelial atrophy were suggestive of chronicity in PRS. These findings are related to the theory that the syndrome is caused by a primary blood vessel dysfunction and altered vascular permeability. It is likely that the natural course of the ocular exudative process in PRS includes a self-limited phase characterized by uveitis, neuroretinopathy and vasculopathy. The ocular process seems to run a course independent of the facial hemiatrophy, in onset and duration, and is not affected by treatment 5.
Better understanding of the pathogenesis in PRS may EXPLAIN the diverse clinical findings manifested. Thorough ophthalmologic examination in patients with progressive hemifacial atrophy (PRS) is essential. | |
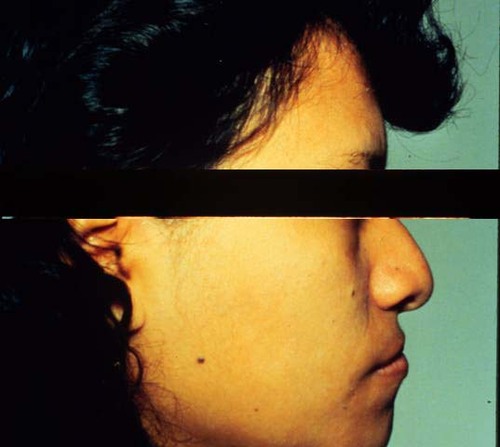
Figure 1
Right facial profile
|
|
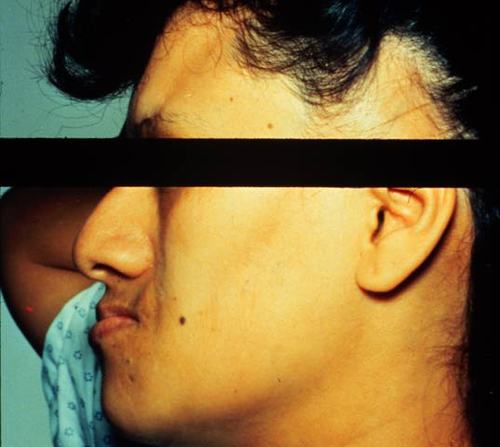
Figure 2
Left facial profile demonstrating left hemifacial atrophy more pronounced in the left inframaxillary facial soft tissues, and madarosis of the temporal aspect of the left eyebrow.
|
|
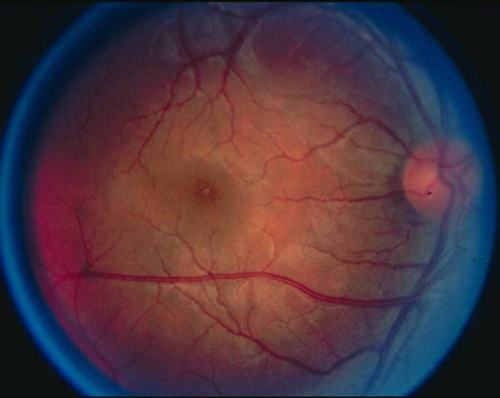
Figure 3
Color photograph of the right posterior pole
|
|

Figure 4
Color phograph of the left posterior pole displaying diffuse inferior pigment epithelial atrophy and areas of subretinal fibrosis.
|
|
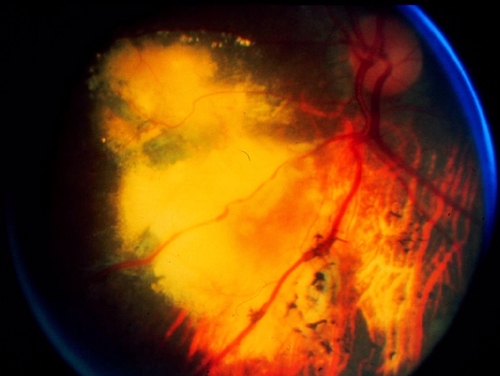
Figure 5
Inferonasal view of the fundus OS displaying the extent of the previews findings.
|
|

Figure 6
Inferior view of the fundus OS demonstrating the extent of the Coat's-like exudative response.
|
|
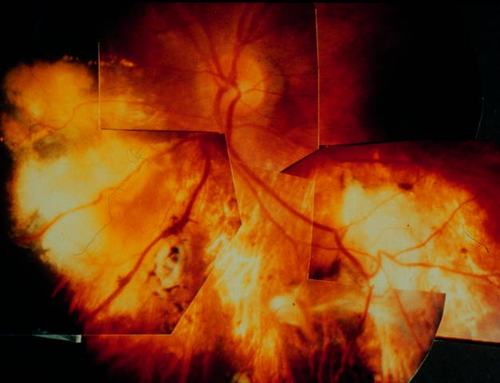
Figure 7
Composite reconstruction of the left fundus displaying diffuse inferior pigment epithelial atrophy and areas of subretinal fibrosis. Subretinal exudates are noted in the nasal peripapillary area.
|
|
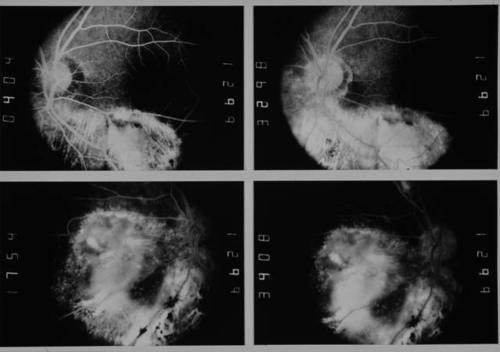
Figure 8
Early and late frames of the fluorescein angiography of the left eye. The top and bottom right frames demonstrate the extensive window defect of the inferior and inferonasal, respectively, posterior pole. The top and bottom left are late frames of the respective areas demonstrating late staining without the presence of vascular or optic nerve leakage.
|
|
| References | 1) Wartenberg R. Progressive hemifacial atrophy. Arch Neurol Psychiatr 1945; 54: 75-96.
2) Muchnick RS, Aston SJ, Rees TD Ocular manifestations and treatment of hemifacial atrophy. Am J Ophthalmol 1979; 88: 889-97.
3) Hoang-Xuan T, Foster CS, Jakobiec FA, Tauber J, de la Maza MS, Krebs W :Romberg's Progressive Hemifacial Atrophy: An Association with Scleral Melting. Cornea 1991;10(4): 361-366.
4) Ong K, Billson FA, Pathirana DSJ, Clifton-Bligh P. A case of progressive hemifacial atrophy with uveitis and retinal vasculitis. Australian and New Zealand J Ophthalmol 1991;19(4): 295-298.
5) Gass JDM, Harbin TS, Del Piero EJ Exudative stellate neuroretinopathy and Coats' syndrome in patients with progressive hemifacial atrophy. Europ J Ophthalmol 1991; 1(1): 2-10. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in