|
|
 |
 |
 |
 |
|
|
Treatment of Retinitis Pigmentosa with Vitamin A
Digital Journal of Ophthalmology 1998
Volume 4, Number 7
October 1, 1998
|
Printer Friendly
|
|
|
|
|
| Abstract | Objective
While studying the course of retinitis pigmentosa with the computer-averaged electroretinogram (ERG) FROM 1979 to 1983, we observed that patients self-treating with a separate capsule of vitamin A or vitamin E seemed to be losing less ERG amplitude annually than those not on these supplements. Intake/response relationships suggested that a total intake of greater than 15,000 IU of preformed vitamin A or greater than 200 IU of vitamin E or the combination was potentially therapeutic. This prompted us to conduct a randomized, controlled, double-masked trial with a 2x2 factorial design FROM 1984 to 1991 to determine whether vitamin A or vitamin E, alone or in combination, would halt or slow the progression of retinitis pigmentosa as monitored by the computer-averaged ERG. We calculated that 601 patients would be needed to detect a significant treatment effect over 5 years when comparing the two groups receiving 15,000 IU per day of vitamin A with the two groups not receiving this dose or when comparing the two groups receiving 400 IU per day of vitamin E with the two groups not receiving this dose. The main outcome variable was the 30 Hz cone flicker ERG. This study and further discussion of its results are described in the June and November, 1993 issues of the Archives of Ophthalmology [1-3].
Methods
In broad outline, patients were evaluated twice over a 6-week interval prior to the institution of vitamin supplementation. The screening visit was used to determine eligibility and the baseline visit to determine intervisit variability. The average of screening and baseline was used to provide pretreatment values. Patients were randomly assigned to one of four treatment groups, as follows: vitamin A, 15,000 IU/day plus vitamin E, 3 IU/day (Group A); vitamin A, 75 IU/day plus vitamin E, 3 IU/day (Group Trace); vitamin A, 15,000 IU/day plus vitamin E, 400 IU/day (Group A+E); and vitamin A, 75 IU/day plus vitamin E, 400 IU/day (Group E). The procedure for randomization took INTO account the estimated dietary intake of vitamins A and E as well as the genetic type recorded at the screening examination. ERGs were monitored annually. Visual field areas and visual acuities were also followed as additional measures of visual function, although we had no expectation that we could detect significant treatment effects with these measures over the course of this study. An outside DATA and Safety Monitoring Committee selected by the National Eye Institute met with us prior to the onset of the trial and annually thereafter.
Results
We found that mean annual rates of decline of remaining ERG amplitude were slowest for the GROUP taking 15,000 IU per day of vitamin A and fastest for the GROUP taking 400 IU per day of vitamin E. These rates were observed among all randomized patients as well as among a subgroup of 354 patients with slightly higher initial ERG amplitudes who could be followed more reliably and whom we designated as "the higher amplitude cohort." Mean annual rates of decline of remaining 30 Hz ERG amplitude among this cohort were as follows: GROUP A, 8.3%; GROUP Trace, 10%; GROUP A+E, 8.8%; and GROUP E, 11.8%. Rates of decline for visual field area showed similar trends, although the differences were not statistically significant. No significant differences were observed among groups with respect to rates of decline of visual acuity. These results are summarized in TABLE 1. | | | Discussion | The mean declines in 30 Hz cone ERG amplitude FROM baseline for the higher amplitude cohort by year are plotted in Figure 1.
The greatest separation among treatment groups occurred at years five and six. Mean change analyses revealed the two groups receiving 15,000 IU of vitamin A per day had, on average, significantly smaller declines FROM baseline than those not receiving this dose at years one, two, five and six (p <0.01 in each of these years) while the two groups receiving vitamin E at 400 IU per day had, on average, significantly greater declines in retinal function than those not on this dose at years one, three, and six (p <0.03 in each of these years).
The mean declines FROM baseline in 30 Hertz cone ERG amplitude by quintile of total vitamin A intake (diet + supplement) irrespective of randomization assignment for the higher amplitude cohort are illustrated in Figure 2.
The average decline in amplitude was greatest for those with a daily vitamin A intake lower than 2428 units, intermediate for those with intake between 2428 and 16,946, and least for those with intake of 16,947 units or greater. A significant difference was found among these groups by analysis of variance. These DATA are presented to SHOW that the optimal total intake of vitamin A appeared to be around 18,000 units per day; that is, a supplement of 15,000 units plus a regular diet of about 3500 units of vitamin A per day resulted in the smallest ERG decline. Vitamin A intake greater than 18,380 units provided no greater benefit. Vitamin A intake of 25,000 IU/day or greater is potentially toxic over the long term [4–6].
These DATA support the hypothesis that a 15,000 unit supplement of vitamin A taken daily will slow the progression of the common forms of retinitis pigmentosa as monitored by ERG testing. The findings also suggest that a 400 unit supplement of vitamin E taken daily may have an adverse effect on the course of the common forms of this disease. With respect to rates of decline of remaining 30 Hz cone ERG amplitude, the beneficial effect of vitamin A was shown for all randomized patients at the p=0.01 level and for the higher amplitude cohort at the p<0.001 level. The possible adverse effect of vitamin E was shown for the higher amplitude cohort (p=0.04) but was not shown for all randomized patients.
Based on these ERG results, it is recommended that most adults with the common forms of RP should take 15,000 units of vitamin A daily under the supervision of their ophthalmologist and avoid high dose supplements of vitamin E such as the 400 units used in this trial. It is also recommended that patients continue on a regular diet without specifically selecting foods containing high levels of preformed vitamin A.
As a precaution we advise patients to have a pretreatment assessment of fasting serum vitamin A and liver function and annual evaluations thereafter. Because of the potential for birth defects, women who are pregnant or planning to become pregnant are advised not to take this dose of vitamin A. Since patients under age 18 were not evaluated, we could not make a formal recommendation for patients under this age.
We observed no toxic side effects attributable to this vitamin A supplement over 4–6 years. Furthermore, we know of no reported case of toxicity in adults in good general health on this dose. We noted no significant differences in treatment effects among different genetic types. The precise mechanism by which vitamin A supplementation provides its benefit is not known; we have speculated that vitamin A may rescue remaining cones, thereby explaining how one supplement may help a GROUP of patients some of whom have different rod-specific gene defects. We have recommended the palmitate form of vitamin A as this was the form used in this study. Other forms might be suitable, but some are probably not, for example beta-carotene, which is not predictably converted to vitamin A FROM one patient to another.
In our study, the rate of decline for the GROUP taking 15,000 IU of vitamin A daily was about 20% slower than the rate of decline for the Trace group. It should be noted that the majority of patients in this trial who had a 30 Hertz ERG near 0.05 microvolt were legally blind. Assuming that the rates of decline observed during the course of this study are sustained over the long-term, the estimated time to reach 0.05 microvolts for an average patient with 1.3 microvolts who starts supplementation at age 32 would be age 70 for GROUP A, 63 for GROUP Trace, 67 for GROUP A+E, and 58 for GROUP E. Thus, vitamin A supplementation can be estimated to provide 7 additional years of useful vision for the average patient in this trial. If a patient has twice the amplitude or 2.6 microvolts and starts vitamin A at age 32, then the time to reach 0.05 µV would be age 78. Although not a cure, for some patients with RP with larger pretreatment ERGs, vitamin A supplementation may make the difference whereby these patients retain some vision for their entire lives.
Since the publication of our paper, we have been asked whether we can detect any treatment effect of vitamin A with respect to visual field area. We have subdivided our study population according to their intervisit variability with respect to field area between the screening and baseline examinations. In our population intervisit variability (as defined by the absolute difference between screening and baseline divided by screening) was £ 5% for 22%; ³ 25% for 25%; with intermediate values for the remainder. For the subset with the lowest intervisit variability (i.e., £ 5%; 125 patients) (see Figure 3), mean rates of decline of remaining visual field area per year were: GROUP A, 3.4%; GROUP Trace, 7.3%; GROUP A+E, 4.0%; and GROUP E, 5.3%. The two groups receiving 15,000 IU/day of vitamin A lost on average significantly less visual field area than those not receiving this dose (p<0.05). The two groups receiving 400 IU/day of vitamin E did not differ significantly FROM those not receiving this dose. Comparisons of specific groups showed that the rate of decline of visual field area for GROUP A differed significantly (p=0.03) FROM the Trace group, whereas the A+E and E groups did not differ significantly FROM that for the Trace group. Therefore for this subset of 125 patients representing all genetic types we could detect a significant beneficial effect of vitamin A supplementation on visual field area.
In summary, based on ERG results, the course of the common forms of RP can be slowed on average among adults on vitamin A supplementation, while the course appears to be hastened by high-dose supplementation with vitamin E, leading to the recommendation that most adults with the common forms of this disease should take a supplement of 15,000 IU of vitamin A palmitate daily under medical supervision and avoid high-dose vitamin E supplements. | |

Figure 1
Mean change FROM baseline over six years in 30 Hz ERG amplitude in the higher amplitude cohort by treatment GROUP (Top), by vitamin A main effect (Center); and by vitamin E main effect (Bottom). Sample sizes for years 1 through 6 respectively were n=171, n=167, n=168, n=164, n=123 and n=59 for patients receiving vitamin A, 15,000 IU/day, and n=178, n=182, n=172, n=171, n=125 and n=64 for patients receiving vitamin A, 75 IU/day. Sample sizes for years 1 through 6 respectively were n=178, n=177, n=173, n=168, n=122 and n=61 for the patients on vitamin E, 400 IU/day and n=171, n=172, n=167, n=167, n=126 and n=62 for patients receiving vitamin E, 3 IU/day. (From: Berson EL, Rosner B, Sandberg MA, Hayes KC, Nicholson BW, Weigel-DiFranco C, Willett W: A randomized trial of vitamin A and vitamin E supplementation for retinitis pigmentosa. Arch Ophthalmol 111:761–772, 1993; copyright 1993, American Medical Association.)
|
|
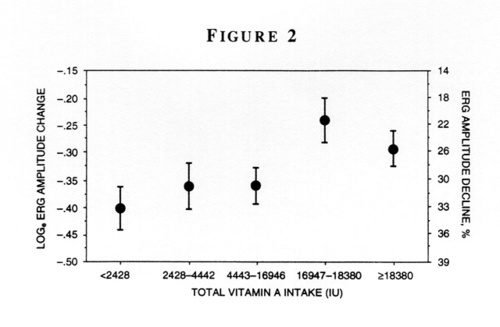
Figure 2
Mean (±SE) decline FROM baseline in 30 Hz electroretinogram (ERG) amplitude by total vitamin A intake (diet plus capsules) irrespective of randomization assignment for all patients in the higher amplitude cohort. The mean decline was calculated as the mean of screening and baseline minus the mean of follow up visits by quintile of total vitamin A intake averaged over all visits. Sample sizes were 69, 72, 74, 65, and 74 for the lowest to highest quintiles of total vitamin A intake. Vertical bars indicate SEs. (From: Berson EL, Rosner B, Sandberg MA, Hayes KC, Nicholson BW, Weigel-DiFranco C, Willett W: A randomized trial of vitamin A and vitamin E supplementation for retinitis pigmentosa. Arch Ophthalmol 1993; 111:761–772; copyright 1993, American Medical Association.)
|
|

Figure 3
Mean (±SE) change per year in visual field area by treatment GROUP (Top) to a V-4e white test light based on longitudinal regression analysis for patients with retinitis pigmentosa with intervisit variability between screening and baseline of no more than 5% (n=125). Sample sizes were as follows: GROUP A, 29; GROUP Trace, 30; GROUP A+E, 28; and GROUP E, 38. Those receiving vitamin A, 15,000 IU/d are compared with those receiving vitamin A, 75 IU/d (bottom left), and those receiving vitamin E, 400 IU/d are compared with those receiving vitamin E, 3 IU/d (bottom right). Vertical bars indicate SEs. (From: Berson EL, Rosner B, Sandberg MA, Hayes KC, Nicholson BW, Weigel-DiFranco C, Willett W: Vitamin A supplementation for retinitis pigmentosa (correspondence). Arch Ophthalmol 111:1456–1458, 1993; copyright 1993, American Medical Association.)
|
|
| Acknowledgements | | This research was supported by grant U10–EYO2014 FROM the National Eye Institute, Bethesda MD and in part by The Foundation Fighting Blindness, Baltimore MD. | | | References | 1. Berson, EL., Rosner, B., Sandberg, MA., Hayes, KC., Nicholson, BW., Weigel-DiFranco, C., Willett, W., A randomized trial of vitamin A and vitamin E supplementation for retinitis pigmentosa. Archives of Ophthalmology 111:761–772 (1993)
2. Massof, RW., Finkelstein, D., Supplemental vitamin A retards loss of ERG amplitude in retinitis pigmentosa (editorial). Archives of Ophthalmology 111:751–754 (1993)
3. Correspondence relating to reference (1). Archives of Ophthalmology 111:1456–1466, (1993)
4. Bauernfeind, JC., The Safe Use of Vitamin A: A Report of the International Vitamin A Consultative GROUP (IVACG). Washington, DC: The Nutrition Foundation; (1980)
5. Hathcock, JN., Hattan, DG., Jenkins, MY., et al., Evaluation of vitamin A toxicity. American Journal of Clinical Nutrition 52:183–202 (1990)
6. Geubel, AP., De Galocsy, C., Alves, N., et al., Liver damage caused by therapeutic vitamin A administration: Estimate of dose-related toxicity in 41 cases. Gastroenterology 100:1701–1709 (1991) | | | Tables |
Table 1: Mean Rates of Decline in Visual Function by Treatment
Group
|
All Randomized Patients |
Higher Amplitude Cohort |
|---|
Test |
A |
Trace |
A+E |
E |
A |
Trace |
A+E |
E |
|---|
30 Hz * |
6.1 |
7.1 |
6.3 |
7.9 |
8.3 |
10.0 |
8.8 |
11.8 |
0.5 Hz * |
8.7 |
9.6 |
9.1 |
10.6 |
8.1 |
9.4 |
8.4 |
10.9 |
Field Area * |
5.6 |
5.9 |
6.2 |
6.3 |
6.3 |
7.2 |
7.3 |
7.8 |
Visual Acuity † |
1.1 |
0.9 |
0.7 |
0.9 |
0.8 |
0.8 |
0.7 |
0.7 |
* Percent decline in remaining function per year
† Letters lost per year
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in