|
|
 |
 |
 |
 |
|
|
Upper Eyelid Shape and Position in the Association of Graves' Disease and Myasthenia Gravis
Digital Journal of Ophthalmology 2000
Volume 6, Number 1
December 1, 2000
|
Printer Friendly
|


 Antonio A.V. Cruz, M.D., Ph.D.
Antonio A.V. Cruz, M.D., Ph.D. | School of Medicine of Ribeirao Preto, University of Sao Paulo, Sao Paulo, Brazil Roberto P. Coelho, M.D. | School of Medicine of Ribeirao Preto, University of Sao Paulo, Sao Paulo, Brazil Maria C. Lucchesi, M.D. | School of Medicine of Ribeirao Preto, University of Sao Paulo, Sao Paulo, Brazil
|
|
|
| Abstract | Objective
To describe the upper eyelid changes of a patient who presented with Graves' disease and myasthenia gravis.
Methods
Digital image processing techniques were used to quantify palpebral fissure images.
Results
Upper eyelid position shifted FROM ptosis to frank retraction in both eyes. Eyelid elevation was not coordinated between the eyes and it was more significant laterally than medially.
Conclusion
Fibrosis of the lateral horn of the levator muscle is not a valid explanation for the enhanced lateral upper eyelid retraction presented by the patient.
Keywords
GRAVES' DISEASE, MYASTHENIA GRAVIS | | | Introduction | | Myasthenia gravis is an autoimmune disorder of the skeletal muscles, characterized by the blockage of the postsynaptic acetylcholine receptors on the end-plates of the myoneural junction.l Levator palpebrae involvement is extremely frequent in myasthenia and eyelid drooping is an important ocular sign of the disease. Graves' disease is also an autoimmnune disease that has the opposite effect on the upper eyelid. Instead of eyelid drooping, Graves' disease typically induces upper eyelid retraction where the etiologic mechanism is not fully understood and is probably multifactorial.2 | | | Discussion | Multiple autoimmune diseases are a well known phenomenon and 5% of the myasthenic patients also present with dysthyroidism.1 We have examined a 63-year-old woman who had myasthenia gravis and Graves' disease. The patient reported that she could not control her eyelids. Examination disclosed bilateral external ophthalmoplegia and Hertel measurements of 30 mm OU. Because the interpalpebral fissure heights were extremely variable, several pictures of her palpebral fissures with different upper eyelid positions could be taken within minutes of consultation. The pictures showed that the upper eyelids were moving independently FROM each other. Complete ptosis could quickly become retraction (figure 1).
Using a slide scanner, images of the pictures were transferred to a microcomputer and processed using the public domain NIH Image program 1.55. Three variables were then analyzed: a) the displacement of the peak of the upper eyelid contour relative to the palpebral fissure midline, b) the palpebral fissure area and c) the ratio between the temporal and nasal areas of the palpebral fissure (T/N ratio).
The palpebral fissure area of the right eye increased 639% FROM figure 1A to IF. This increment was mainly due to the expansion of the lateral part of the palpebral fissure. The T/N ratio more than tripled increasing 210 % FROM figure 1A to IF. At the same time, the peak of the upper eyelid contour moved FROM 8.62-mm medial to midline to 4-mm lateral to the midline (figure 2). The left eye showed similar changes but in a different temporal order.
The typical laterally enhanced retraction seen in Graves' disease is displayed in figure 1 FROM D to F (right eye). This sign, also called "lateral lid flare", is assumed by some authors to be an indication of eyelid inflammation and fibrosis of the lateral levator horn.2 This explanation clearly is not true for our case. The upper eyelids moved freely FROM ptosis to retraction without any sign of restriction. When the upper eyelid was ptotic, the upper contour was almost flat, with its peak displaced medially to the midline. However, when the levator muscle started to work, the extreme elevation of the lateral part of the eyelid caused the peak of the upper contour to be displaced laterally FROM the midline. All of this took place, probably, just because the levator muscle is stronger laterally than medially. | |

Figure 1
|
|
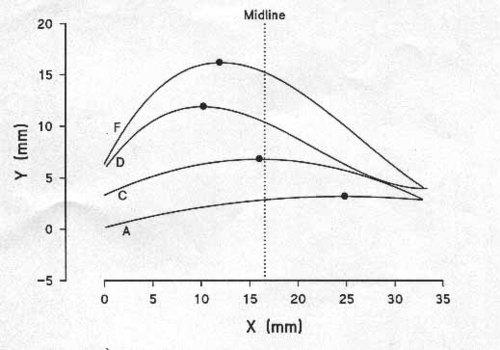
Figure 2
|
|
| References | 1 - GlaserJ. Infranuclear disorders of eye movements. In: Tasman W, Jaeger. E A, editors. Duane's Clinical Ophthalmology. Philadelphia: Lippincott-Raven, 1995:1-56
2- Ceisler EJ, Bilyk JR, Rubin PAD, Burks WR, Shore JW. Results of Mullerectomy and levator aponeurosis transposition for the correction of upper eyelid retraction in Graves Disease. Ophthalmology 1995; 102:483-492. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in