|
|
 |
 |
 |
 |
|
|
An eye center–wide burnout intervention: resilience program and burnout survey
Digital Journal of Ophthalmology 2019
Volume 25, Number 1
March 24, 2019
DOI: 10.5693/djo.01.2019.02.001
|
Printer Friendly
Download PDF |


 Jullia A. Rosdahl, MD, PhD
Jullia A. Rosdahl, MD, PhD | Department of Ophthalmology, Duke University, Durham, North Carolina Karen Kingsolver, PhD | Department of Ophthalmology, Duke University, Durham, North Carolina
|
|
|
| Abstract | Purpose
Burnout affects half of doctors in the United States. Programs to decrease burnout and foster resilience are needed to prevent loss of doctors in the workforce and maintain quality care. To ameliorate burnout at our eye center, we developed a resilience program and used a survey to identify additional groups with higher burnout for future interventions.
Methods
The eye center–wide resilience program consisted of the baseline burnout survey, short email wellness tips, a grand rounds presentation, short wellness presentations at faculty meetings, and a small group discussion series with clinical faculty. The anonymous burnout survey was performed prospectively online at the beginning of this program. The survey participants consisted of respondents at the Duke Eye Center, including all doctors, scientists, clinical and research staff, trainees, and administrative and educational staff, in June and July of 2017. The short, anonymous electronic survey consisted of 10 demographic questions, 2 validated burnout questions, and 1 validated work-life balance question.
Results
A total of 593 individuals were invited to participate, of whom 252 completed the survey. Overall, 37% of the respondents reported being emotionally exhausted, and 17% had experienced depersonalization. With regard to work-life balance, 43% of the respondents were satisfied and 34% were dissatisfied. Burnout was higher in respondents who participated in clinical care (P = 0.001), particularly among ophthalmic technicians (P = 0.044). Feedback from the doctors participating in the “Doctors Lounge” suggested perceived benefits, including enhanced collegiality, life skills, and improved self-management.
Conclusions
Our baseline burnout survey showed higher burnout in our clinical workers, particularly in our ophthalmic technicians. Planning for next year will include the providers identified in the survey.
| | | Introduction | “Burnout” is characterized by emotional exhaustion, depersonalization, and decreased sense of personal accomplishment;(1) in the health-care profession, it negatively affects not only the individuals experiencing burnout but also patients and colleagues. A large study of doctors showed that about half are experiencing burnout and struggle with work-life balance.(2) Burnout results from a mismatch between workload and control and between resources and support within an organizational culture;(3) factors at the national, state, and regional levels contribute to burnout, as do those related to the medical system and to the individual.(4)
Ophthalmology as a specialty is not immune to burnout, and the issue is being recognized by leaders interested in developing programs to decrease and prevent burnout and to foster resilience. Mindfulness-based programs can decrease burnout in doctors.(5) Mindfulness is a meditation practice based on focusing one’s attention on the present moment.(6) Practicing mindfulness improves attention, memory, and executive function.(7) Mindfulness-based interventions include small-group interventions,(8) mindfulness-based stress reduction courses,(6), and health coaching.(9)
We describe the resilience program that we have developed and implemented at our academic eye center, including doctors as well as nonclinical faculty, support staff, and administrative staff, with the recognition that doctors work within a community of caregivers, all of whom may be subject to symptoms of burnout. In addition, we present the results of an eye center–wide burnout survey, which was carried out using validated questions to help understand who, besides the doctors, may benefit from targeted interventions. To our knowledge, this is the first burnout survey involving an entire academic eye center. | | | Materials and Methods | This prospective survey study was reviewed by the Duke Institutional Review Board and exempted from approval. The research adhered to the tenets of the Declaration of Helsinki.
The short, online survey consisted of 10 demographic questions, 2 burnout questions,(10) and 1 work-life balance question,(2) and used the RedCAP electronic data capture tool.(11) See Appendix. The Duke Office of Clinical Research disseminated the survey and collected the responses, serving as an intermediary to ensure anonymity of the participants. The survey was emailed to 593 individuals at the Duke Eye Center, including all clinicians, scientists, clinical and research staff, trainees, administrative and educational staff, in June and July of 2017. The survey responses were analyzed with descriptive statistics: means and standard deviations for age and frequencies and proportions for categorical variables. To assess the significance of differences among the demographic groups’ scores, the χ2 test or the Fisher exact test was used for categorical variables and t test of difference between means for age, using SAS software version 9.4.
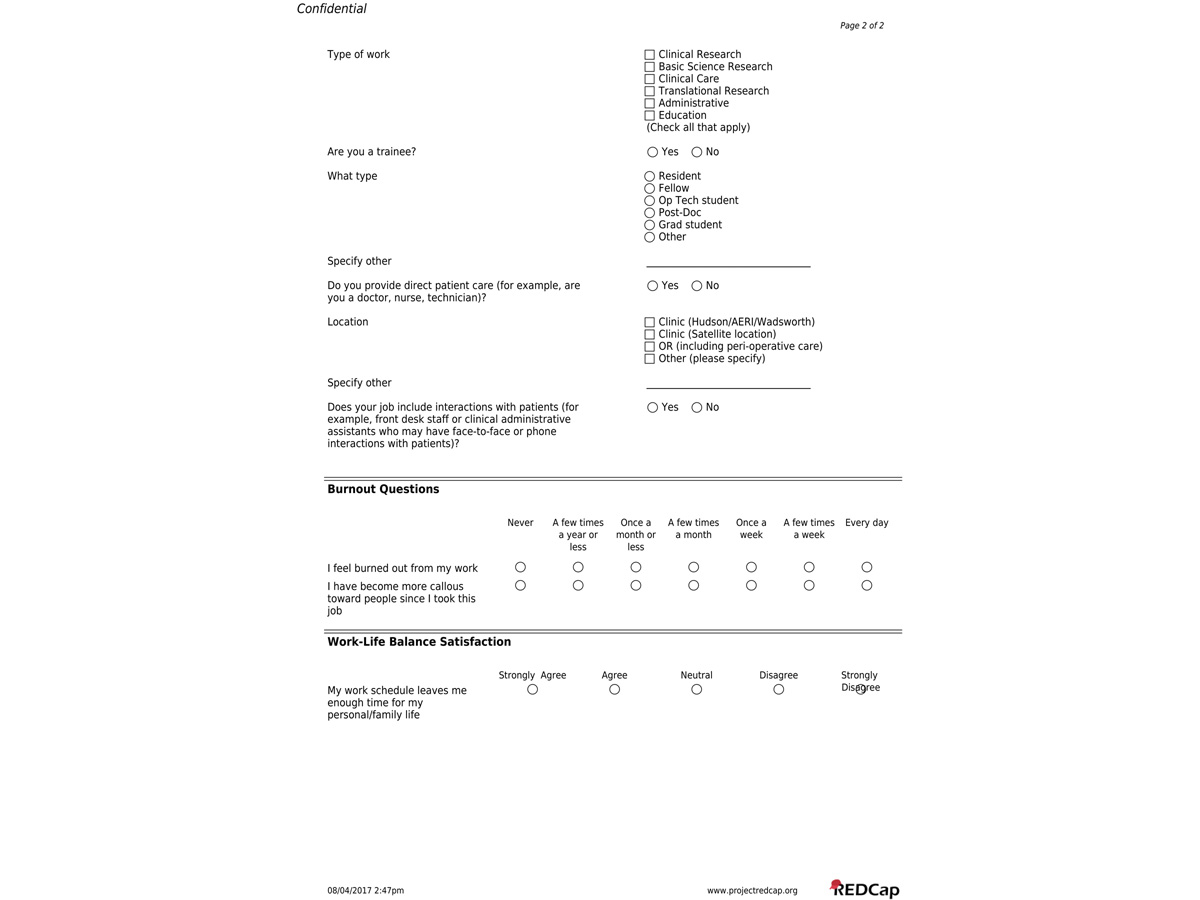
The resilience program was developed by the authors based on literature review and their extensive prior work in coaching and training doctors (KK) and residents (KK, JAR). The baseline survey, as described above, was implemented as the initial step of this plan, in preparation for future interventions. The resilience plan for 2017-2018 (Table 1) consisted of multiple parts: (1) wellness emails, (2) grand rounds presentation, (3) wellness presentations for faculty, and (4) “Doctors Lounge” discussion series. Clinical faculty were primarily targeted during this initial year based on literature showing increasing burnout in this group,(2) with plans to target groups identified by the survey in the future.
Short texts (about 50-100 words) with wellness tips were formatted for monthly email distribution to the entire eye center (approximately 600 people). The short size optimized viewing on a mobile device. Tips included easy and practical strategies for individuals to use in their daily lives. Topics included mindfulness, stress and anxiety, and transitioning between work and home. Techniques included mindful breathing, appreciative inquiry, guided imagery, and positivity. See Figure 1.
At the beginning of the academic year (August 2017), a grand rounds presentation was made to the department (approximately 60 faculty and trainees attended), given by the authors and an additional university wellness expert (Sharon Hull, MD, MPH, Director of Duke University School of Medicine Executive Coaching Program). The presentation was prefaced with an outline of the 2017-18 resilience plan. An overview of the problem of burnout in doctors was presented and followed by potential solutions,(12) which included 8 practical skills for well-being (Figure 2). A question-and-answer discussion followed.
To follow-up on the grand rounds, the resilience plan included short presentations at faculty meetings further exploring the 8 practical skills: mindfulness, boundaries, strengths, activation, reality, positivity, effectiveness, and commitment.
Finally, the resilience plan included a small group discussion series, “Doctors Lounge.” Individual email invitations were sent to all clinical faculty to identify a small group of participants; the initial goal was a group of 6-8 clinical faculty, which was increased in number and capped at 12 based on high interest. Eight group meetings were held with those 12 faculty members. Each meeting included dinner (provided by departmental funds) and a facilitated discussion (led by KK and JAR) on one of the mindfulness-based physician wellness skills (Figure 1, additional materials available on request). The small group format was used to develop relationships between the participating doctors. Feedback was collected after the last session via anonymous paper surveys.
| |

Figure 1
Example of wellness tips emailed monthly to the entire eye center.
|
|

Figure 2
Wheel of skills for physician well-being. This diagram summarizes the 8 skills for well-being. The core skill is mindfulness, or being present. “Boundaries” refers to the skill of creating and maintaining healthy boundaries. “Strengths” refers to skills for identifying and working from one’s strengths. “Activation” refers to the skill of assessing one’s own level of activation to see one’s patterns of stress and resiliency. “Reality” refers to the skill of letting go of what cannot be controlled in one’s life. “Positivity” refers to the skills based on positive psychology, such as appreciation and gratitude. “Effectiveness” is the skill of assessing one’s own effectiveness, of one’s vulnerabilities and triggers, to help promote positive behaviors. “Commitment” refers to making a commitment to one’s own personal and professional growth to enhance well-being. Each of these “wedges” of our wheel is explored with interactive and self-reflective exercises, during the “Doctors Lounge” sessions.
|
|
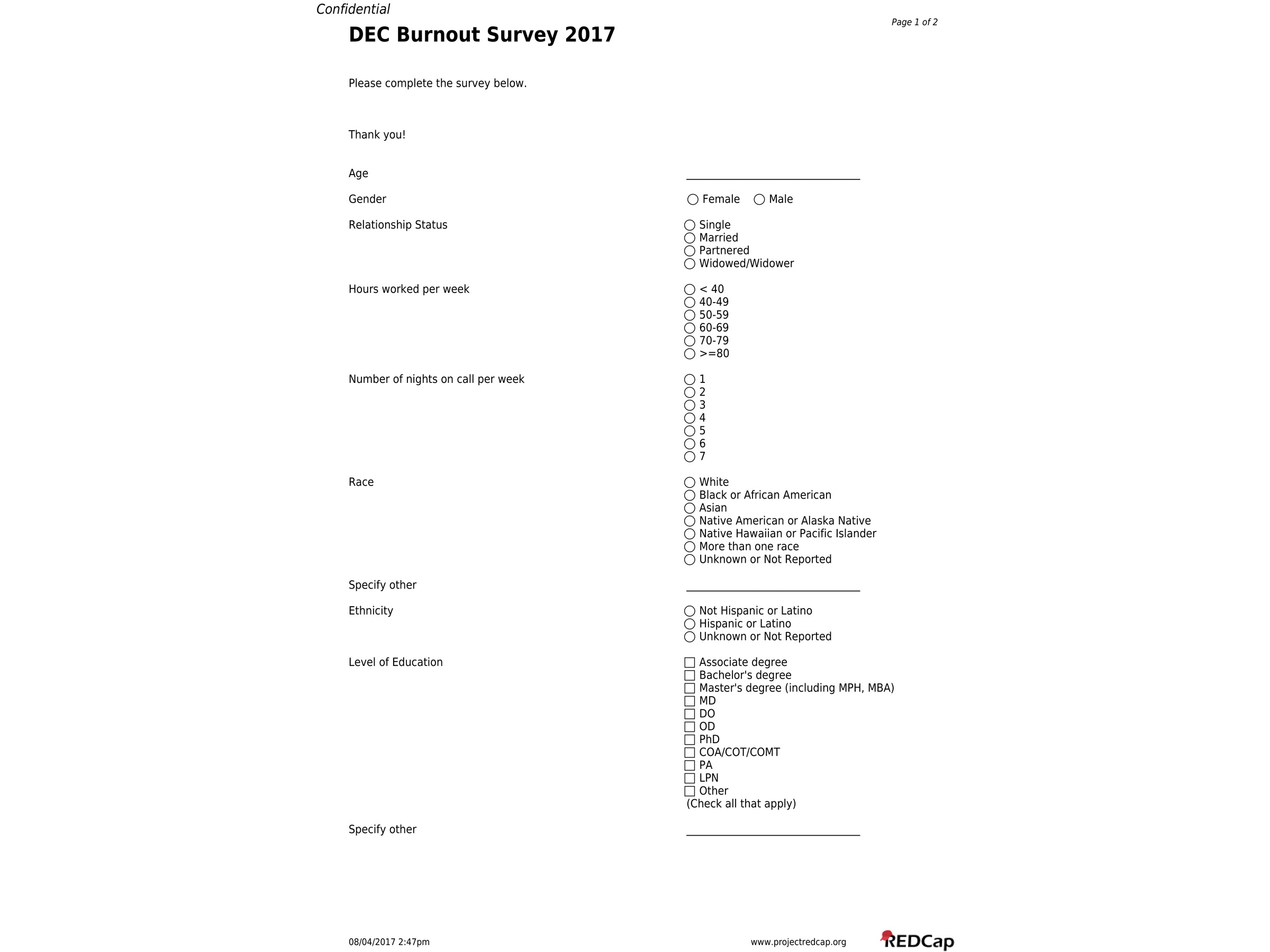
Appendix
Duke Eye Center Burnout Survey (page 1)
|
|
Appendix
Duke Eye Center Burnout Survey (page 2)
|
|
| Results | The response rate to the survey was 42%. The demographics of the participants are summarized in Table 2.
Overall, 37% of the respondents reported being emotionally exhausted, and 17% reported suffering depersonalization (Table 3); burnout in subset who were physicians was similar: 39%, emotional exhaustion, and 17%, depersonalization. This rate is similar to the 33 percent burnout in our department reported in June 2016 on a work culture survey (Edward Buckley, MD, personal communication). Burnout (Table 4) was higher in respondents who participated in clinical care (P = 0.001). Differences in race and ethnicity were seen, with higher burnout in blacks and lower burnout in whites and Asians (P = 0.030) and higher burnout in Hispanics than non-Hispanics (P = 0.005). Respondents with master’s degrees (P = 0.029) and PhDs (P = 0.025) had lower burnout, whereas the certified ophthalmic assistants/technicians/medical technicians had higher burnout (P = 0.044). Among the trainees, fellows had higher burnout than the residents at the time of the survey (P = 0.028).
Overall, 43% of the respondents were satisfied with their work-life balance, and 34% were dissatisfied (Table 3); in the subset who were physicians, there was a high percentage who were dissatisfied, 43%, but this difference was not statistically significant (P = 0.126). A statistically significant difference was noted for relationship status: married or partnered respondents were more likely to be dissatisfied than single respondents (P = 0.006).
Our preliminary experience with the doctors participating in the “Doctors Lounge” has been extremely positive, with participants traveling 30-60 miles after long clinical days, on account of the benefits that they perceive regarding collegiality, life skills, and improved self-management. | | | Discussion | In our eye center-wide survey on burnout, we found that staff who are providing clinical care are more likely to have burnout. Similar to national studies, the rate of burnout in doctors we surveyed was 39%. The respondents with master’s degrees and PhDs had a lower burnout rate (17% and 12%, resp.); given the small numbers (24 with master’s and 17 with PhDs) and lack of comparative data from other studies, the significance of these data is not clear.
We found that 49% of ophthalmic technicians had burnout at the time of the survey, higher than other groups, including medical doctors. The high burnout in this group may be due in part to administrative changes occurring when the survey was distributed; however, these workers are also “at the front lines” in patient care: answering phone calls, responding to electronic medication requests and queries, explaining delays in clinic flow, and navigating the needs of multiple ophthalmic specialties and providers. Although there is no comparative data from other studies to confirm this finding at other centers, these data suggest that this group of professionals may benefit from targeted resilience interventions at the individual level as well as participation at the system level to decrease burnout in health-care workers.
We anticipate that our next resilience plan will include a second “Doctors Lounge” small group for faculty, based on the initial high interest in this program and ongoing positive feedback from the current group; in addition, based on the survey results, the plan will include interventions targeted at our ophthalmic technicians. In order to assess the effectiveness of the resilience plan overall, a combination of qualitative feedback and quantitative survey data will be used annually.
In the case of our resilience program, we made several practical concessions (short but validated survey, targeted and center-wide implementation) in order to reach many of our workers via multiple modalities (email tips, electronic survey, departmental presentation, faculty meetings, small groups). As a result, rigorous scientific assessment of the plan’s efficacy is difficult to assess. However, the combination of qualitative and quantitative data offers timely and practical guidance for the administration and continued development of a meaningful resilience program. | | | Acknowledgements | | We gratefully acknowledge the financial support of Dr. Edward Buckley, the statistical support of Dr. Sandra Stinnett, and the survey administrative support Ms. Ebony Burns, as well as the Duke Eye Center doctors and staff who participated in the survey and resilience activities. | | | References | 1. Maslach C JS, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto: Consulting Psychologists Press; 1996.
2. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clinic Proceedings 2015;90:1600-13.
3. Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clinic Proceedings 2017;92:129-46.
4. Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA 2017;317:901-2.
5. Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009;302:1284-93.
6. Paulson S, Davidson R, Jha A, Kabat-Zinn J. Becoming conscious: the science of mindfulness. Ann N Y Acad Sci 2013;1303:87-104.
7. Jha AP, Krompinger J, Baime MJ. Mindfulness training modifies subsystems of attention. Cogn Affect Behav Neurosci 2007;7:109-19.
8. Marchand WR. Mindfulness-based stress reduction, mindfulness-based cognitive therapy, and Zen meditation for depression, anxiety, pain, and psychological distress. J Psychiatr Pract 2012;18:233-52.
9. Schneider S, Kingsolver K, Rosdahl J. Physician coaching to enhance well-being: a qualitative analysis of a pilot intervention. Explore (NY) 2014;10:372-9.
10. West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med 2009;24:1318-21.
11. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81.
12. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016;388(10057):2272-81.
| |
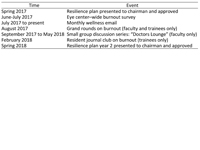
Table 1
Resilience plan with timeline
|
|

Table 2
Demographic characteristics of survey respondents
|
|
Table 3
Overall burnout and work-life balance
|
|
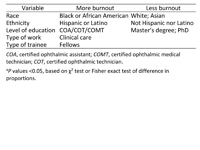
Table 4
Univariable analysis for burnout(a)
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in