|
|
 |
 |
 |
 |
|
|
Surgical approach to limiting skin contracture following protractor myectomy for essential blepharospasm
Digital Journal of Ophthalmology 2017
Volume 23, Number 4
November 5, 2017
DOI: 10.5693/djo.01.2016.11.001
|
Printer Friendly
Download PDF |



Jeremy Clark, MD | Department of Ophthalmology and Visual Sciences, Kentucky Lions Eye Center, University of Louisville, Louisville, Kentucky John Randolph, MD | Department of Ophthalmology and Visual Sciences, Kentucky Lions Eye Center, University of Louisville, Louisville, Kentucky Jason A. Sokol, MD | Department of Oculofacial Plastic and Reconstructive Surgery, University of Kansas Medical Center, Kansas City, Kansas Nicholas A. Moore, MD | Oculofacial Plastic and Orbital Surgery, Department of Ophthalmology, Indiana University, Indianapolis, Indiana Hui Bae H. Lee, MD | Oculofacial Plastic and Orbital Surgery, Department of Ophthalmology, Indiana University, Indianapolis, Indiana William R. Nunery, MD | Department of Ophthalmology and Visual Sciences, Kentucky Lions Eye Center, University of Louisville, Louisville, Kentucky; Oculofacial Plastic and Orbital Surgery, Department of Ophthalmology, Indiana University, Indianapolis, Indiana
|
|
|
| Abstract | Purpose
To report our experience with protractor myectomy in patients with benign essential blepharospasm who did not respond to serial botulinum toxin injection, and to describe intra- and postoperative techniques that limited skin contracture while also providing excellent functional and cosmetic results.
Methods
The medical records of patients with isolated, benign, essential blepharospasm who underwent protractor myectomy from 2005 to 2008 by a single surgeon were reviewed retrospectively. The technique entailed operating on a single eyelid during each procedure, using a complete en bloc resection of all orbicularis tissue, leaving all eyelid skin intact at the time of surgery, and placing the lid under stretch with Frost suture and applying a pressure dressing for 5-7 days.
Results
Data from 28 eyelids in 7 patients were included. Average follow-up was 21.5 months (range, 4-76 months). Of the 28 eyelids, 20 (71.4%) showed postoperative resolution of spasm, with no further need for botulinum toxin injections. In the 8 eyelids requiring further injections, the average time to injection after surgery was 194 days (range, 78-323 days), and the average number of injections was 12 (range, 2-23 injections). All but one eyelid had excellent cosmetic results, without signs of contracture; one eyelid developed postoperative skin contracture following premature removal of the Frost suture and pressure dressing because of concerns over increased intraocular pressure.
Conclusions
In our patient cohort, this modified technique resulted in excellent cosmetic and functional results and limited postoperative skin contracture. | | | Introduction | | Benign essential blepharospasm (BEB) is a rare disease, with a reported incidence of 1.2 persons per 100,000 annually and prevalence of 16-133 per million.(1-3) The first-line treatment for this condition is serial botulinum A toxin injections, which are effective for the rapid but temporary treatment of BEB.(4-13) In patients who fail to respond to this treatment, protractor myectomy, which has been performed routinely for decades, remains a highly effective treatment, with few complications.(14-23) Nevertheless, postoperative complications can arise, including hemorrhage, hematoma, lid edema, lagophthalmos, skin necrosis, and skin contracture.(24) This study describes intra- and postoperative techniques used to limit the development of skin contracture while simultaneously maintaining excellent functional and cosmetic results. | | | Materials and Methods | The medical records of patients who underwent protractor myectomies by a single surgeon (WRN) in an ambulatory setting for isolated BEB from 2005 to 2008 were reviewed retrospectively. Ethics consent was waived by the University of Louisville Institutional Review Board for this study, which complied with the US Health Insurance Portability and Accountability Act of 1996. The primary indication for protractor myectomy was poor response to serial botulinum A toxin injections. The goal of surgery in these patients suffering from blepharospasm was to perform careful and complete orbiculectomy of the upper and lower eyelids. Main outcome measures were complete resolution of spasm or need for continued botulinum toxin injections after orbiculectomy, length of time between botulinum toxin injections after orbiculectomy, and number of eyelids with cicatricial retraction with symptomatic lagophthalmos. Patients were excluded if they had undergone any previous eyelid surgery or if there was presence of preoperative eyelid retraction.
Surgical Technique
The protractor myectomy was performed in multiple phases, in which the orbicularis was segmentally resected at each operation. The upper protractor muscles were approached through an upper lid crease incision, similar to that used in blepharoplasty and ptosis surgery (Figure 1A). The skin was meticulously dissected from the underlying muscle in a plane extending superiorly to the junction of the frontalis and orbicularis muscles, medially to the canthus and laterally to the inferior aspect of the horizontal raphe. The orbital, preseptal, and majority of pretarsal divisions of the orbicularis were then removed en bloc to limit disruption of the underlying neurovascular structures (Figure 1B). The remaining pretarsal orbicularis muscle was carefully excised exposing the base of the underlying eyelashes (Figure 1C), thus ensuring complete removal of all orbicularis muscle tissue. There was no removal of any excess upper or lower eyelid skin, and corrugator supercilli and procerus muscles were left intact in all cases.
In the lower eyelid, the overlying skin was dissected from the orbicularis muscle down to the inferior orbital rim. All visualized portions of the orbicularis were removed in a similar procedure to the upper eyelid. Additional eyelid deformities, such as lid malposition, brow ptosis, blepharoptosis and dermatochalasis, were addressed at a later time, once the patient had fully recovered from myectomy surgery. To avoid postoperative skin contracture, the incision was reapproximated using 6-0 fast-absorbing gut sutures. Subsequently, a Frost suture and pressure dressing were applied to the lid in the immediate postoperative period (Figure 1D). Both were kept in place for 5-7 days to ensure that constant pressure and stretch were exerted on the eyelid. Because this surgical technique involves the use of a Frost suture and pressure patch, a single eyelid was operated on with each procedure. | |

Figure 1. Surgical technique of protractor myectomy
A, The upper eyelid protractor muscles are approached through a lid crease incision. B-C, The orbital, preseptal and pretarsal divisions of the orbicularis are removed en bloc, exposing the base of the underlying eyelashes. D, Frost suture is applied to the eyelid in the immediate postoperative period.
|
|
| Results | | A total of 28 eyelids of 7 patients (median age, 63 years; range, 50-93 years) were included. Average follow-up time was 21.5 months (range, 4-76 months). Of the 28 eyelids, 20 (71.4%) showed resolution of spasm and no longer required treatment with botulinum toxin following orbiculectomy (Figure 2). Of the 8 eyelids that required further treatment with botulinum toxin postoperatively, the average time to injection after surgery was 194 days (range, 78-323 days), and the average number of injections each eye received was 12 (range, 2-23 injections). All but one eyelid had excellent cosmetic results without signs of contracture. One eyelid developed postoperative contracture following premature removal of the Frost suture and pressure dressing two days after surgery due to concerns over increased intraocular pressure (Figure 3). This contracture resulted in persistent lagophthalmos and corneal exposure requiring upper eyelid retraction repair with a full-thickness skin graft. | |

Figure 2. Demonstration of improvement of blepharospasm after protractor myectomy
A, Preoperative photograph showing severe blepharospasm. B, Marked improvement 6 months after bilateral upper and lower eyelid myectomy surgery.
|
|
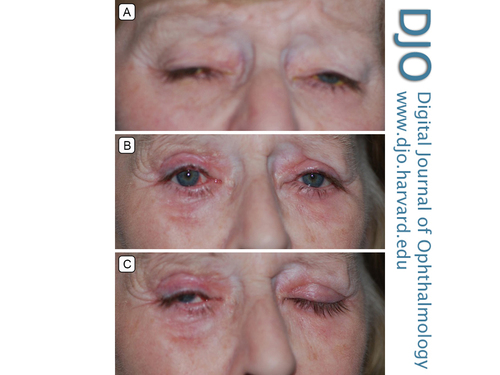
Figure 3. Demonstration of postoperative skin contracture
A, Preoperative picture demonstrating severe blepharospasm that was unresponsive to serial botulinum toxin injections. B, Improvement of blepharospasm 3 months following bilateral upper and lower eyelid myectomy surgery. C, The right upper eyelid developed postoperative contracture following premature removal of Frost suture and pressure dressing 2 days after surgery.
|
|
| Discussion | Botulinum A toxin is a widely accepted treatment for BEB.(4-13) Although many patients experience rapid symptomatic relief, the effects of botulinum toxin are temporary, and many patients develop resistance to its effects with repeated injections. Thus, there are patients whose symptoms are poorly controlled with botulinum toxin injections alone.(25) Complications of botulinum toxin injections are well documented and include ptosis, corneal exposure, lagophthalmos, symptomatic dry eye, lid malposition, epiphora, photophobia, diplopia, ecchymosis, and lower facial weakness.(24-26) In addition, BEB is associated with many eyelid deformities, including lid malposition, brow ptosis, dermatochalasis, blepharoptosis, and blepharophimosis, all of which may become more pronounced following botulinum toxin injections.(24) Furthermore, many patients are unwilling or unable to undergo long-term serial injections. Therefore, in patients who experience side effects, are unable to undergo serial injections, or develop relative resistance to injections the use of protractor myectomy is seen as a definitive treatment for BEB.(14-23)
In a long-term study of patients with botulinum toxin resistant BEB in whom subtotal myectomy was preformed, Chapman et al showed that myectomy provided subjective improvement and decreased the long-term need for injections in over 50% of patients.(15) Anderson et al reported that in 330 patients who received upper eyelid myectomy or upper and lower eyelid myectomy, 88% noted improvement with only 38% requiring injections after full myectomy.(24) McCord et al comparing facial nerve avulsion to an eyebrow-eyelid muscle stripping procedure reported that secondary procedures were required 4.5 times more often with the facial nerve avulsion and that patients’ subjective response to and acceptance of myectomy was much greater.(17)
Studies have also suggested that patients who require botulinum toxin after myectomy often require fewer injections overall, and experience longer periods of relief between injections.(27) In a study of 14 patients who underwent myectomy for BEB, Mauriello et al found that the average duration of effect of injections increased from 122.1 days in the patients prior to undergoing eyelid surgery to 210.5 days after surgery.(27) In concordance with these studies, our results revealed that 71.4% (20 of 28) of eyelids did not, within the study period, require additional botulinum toxin treatments following myectomy surgery. Additionally, in those patients requiring reinjection after surgery, the average time to repeat injection was approximately 6 months (194 days). We attribute these encouraging results to our new treatment paradigm and the associated intra- and postoperative techniques used in these patients.
We recognize that this study is not without limitations. The small sample size and retrospective nature limit our ability to report on the long-term effect of the myectomy procedure described above.
Given that myectomy has been successfully preformed for decades with favorable results, debate still exists as to the extent of muscle removal (partial vs complete), the timing and sequence of myectomy (simultaneous vs staged), on which lid to operate (upper vs lower), and whether removal of eyelid skin is necessary.(14-16,24,28) The technique we describe represents a new perspective on the protractor myectomy procedure. We view the surgery as creation of an in situ full-thickness skin graft and approach our postoperative care accordingly. The complete separation of the orbicularis oculi from the overlying epidermis and dermis disrupts normal perfusion to the overlying skin. Disruption of this process can lead to partial or total necrosis and scar contracture. Furthermore, the natural course of full-thickness skin grafts is to undergo primary contraction during healing. Therefore, measures must be taken to ensure appropriate neovascularization occurs to reduce the occurrence of contracture. We achieve this through the use of Frost sutures and pressure dressings for 5-7 days to place tension on the eyelid and limit primary contraction. In addition, concurrent excess skin removal procedures are delayed until a later date if needed. Because a Frost suture and pressure dressing are used, only a single eyelid is operated on at each procedure, and the muscle is removed en bloc to ensure complete resection of the entire orbicularis. | | | Acknowledgements | This study was supported by an unrestricted grant from Research to Prevent Blindness, Inc (New York, NY). The funding party had no role in the study design, collection of data, analysis of data, writing of the manuscript, or decision to submit the manuscript.
Presented at the 40th Annual Scientific Symposium of the American Society of Ophthalmic Plastic and Reconstructive Surgery (San Francisco, California, October 2009). | | | References | 1. Bradley EA, Hodge DO, Bartley GB. Benign essential blepharospasm among residents of Olmsted County, Minnesota, 1976 to 1995: an epidemiologic study. Ophthal Plast Reconstr Surg 2003;19:177-81.
2. Defazio G, Livrea P, De Salvia R, et al. Prevalence of primary blepharospasm in a community of Puglia region, Southern Italy. Neurology 2001;156:1579-81.
3. Defazio G, Livrea P. Epidemiology of primary blepharospasm. Mov Disord 2002;17:7-12.
4. Barnes MP, Best D, Kidd L. The use of botulinum toxin type-B in the treatment of patients who have become unresponsive to botulinum toxin type-A—initial experiences. Eur J Neurol 2005;12:947-55.
5. Bhidayasiri R, Cardoso F, Truong DD. Botulinum toxin in blepharospasm and oromandibular dystonia: comparing different botulinum toxin preparations. Eur J Neurol 2006;13:21-9.
6. Cheng CM, Chen JS, Patel RP. Unlabeled uses of botulinum toxins: a review, part 2. Am J Health Syst Pharm 2006;63:225-32.
7. Cheng CM, Chen JS, Patel RP. Unlabeled uses of botulinum toxins: a review, part 1. Am J Health Syst Pharm 2006;63:145-52.
8. Dutton JJ, White JJ, Richard MJ. Myobloc for the treatment of benign essential blepharospasm in patients refractory to botox. Ophthal Plast Reconstr Surg 2006;22:173-7.
9. Seiff SR, Zwick OM. Botulinum toxin management of upper facial rhytidosis and blepharospasm. Otolaryngol Clin North Am 2005;38:887-902.
10. Silveira-Moriyama L, Goncalves LR, Chien HF. Botulinum toxin a in the treatment of blepharospasm: a 10-year experience. Arq Neuropsiquiatr 2005;63:221-4.
11. Truong D, Comella C, Fernandez HH, Ondo WG. Efficacy and safety of purified botulinum toxin type A (Dysport) for the treatment of benign essential blepharospasm: a randomized, placebo-controlled, phase II trial. Parkinsonism Relat Disord 2008;14:407-14.
12. Kenney C, Jankovic J. Botulinum toxin in the treatment of blepharospasm and hemifacial spasm. J Neural Transm 2008;115:585-91.
13. Roggenkamper P, Jost WH, Bihari K. Efficacy and safety of a new Botulinum Toxin Type A free of complexing proteins in the treatment of blepharospasm. J Neural Transm 2006;113:303-12.
14. Gillum WN, Anderson RL. Blepharospasm surgery. An anatomical approach. Arch Ophthalmol 1981;99:1056–62.
15. Chapman KL, Bartley GB, Waller RR, Hodge DO. Follow-up of Patients With Essential Belpharospasm Who Underwent Eyelid Protractor Myectomy at the Mayo Clinic From 1980 to 1995. Ophthal Plast Reconstr Surg 1999;15:106-10.
16. Kennedy RH, Waller RR, Henderson JW, Kesty KR. Management for Blepharospasm. Ophthal Plast Reconstr Surg 1985;1:253-61
17. McCord CD, Coles WH, Shore JW, Spector R, Putnam JR. Treatment of essential blepharospasm: comparison of facial nerve avulsion and eyebrow eyelid muscle stripping procedure. Arch Ophthalmol 1984;102:266–73.
18. Frueh BR, Musch DC, Bersani TA. Effects of eyelid protractor excision for the treatment of benign essential blepharospasm. Am J Ophthalmol 1992;113:681-86.
19. Bates AK, Halliday BL, Bailey CS, Collin JR, Bird AC. Surgical management of essential blepharospasm. Br J Ophthalmol 1991;75:487–90.
20. Grivet D, Robert PY, Thuret G. Assessment of blepharospasm surgery using an improved disability scale: study of 138 patients. Ophthal Plast Reconstr Surg 2005;21:230-4.
21. Patel BC. Surgical management of essential blepharospasm. Otolaryngol Clin North Am 2005;38:1075-98.
22. Georgescu D, Vagefi MR, McMullan TF, McCann JD, Anderson RL. Upper eyelid myectomy in blepharospasm with associated apraxia of lid opening. Am J Ophthalmol Mar 2008;145:541-7.
23. Garland PE, Patrinely JR, Anderson RL. Hemifacial spasm: results of unilateral myectomy. Ophthalmology 1987;94:288-94.
24. Anderson RL, Patel BCK, Holds JB, Jordan DR. Blepharospasm: past, present and future. Ophthal Plast Reconstr Surg. 1998;14:305-17.
25. Cote TR, Mohan AK, Polder JA. Botulinum toxin type A injections: adverse events reported to the US Food and Drug Administration in therapeutic and cosmetic cases. J Am Acad Dermatol 2005;53:407-15.
26. Grandas F, Elston J, Quinn N, Marsden CD. Blepharospasm: a review of 264 patients. J Neurol Neurosurg Psychiatry 1988;51:767-72.
27. Mauriello JA Jr, Keswani R, Franklin M. Long-term enhancement of botulinum toxin injections by upper-eyelid surgery in 14 patients with facial dyskinesias. Arch Otolaryngol Head Neck Surg. 1999;125:627-31.
28. De Groot V, De Wilde F, Smet L, Tassignon MJ. Frontalis suspension combined with blepharoplasty as an effective treatment for blepharospasm associated with apraxia of eyelid opening. Ophthal Plast Reconstr Surg 2000;16:34-38.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in