|
|
 |
 |
 |
 |
|
|
External dacryocystorhinostomy outcomes in patients with a history of dacryocystitis
Digital Journal of Ophthalmology 2015
Volume 21, Number 3
September 20, 2015
DOI: 10.5693/djo.01.2014.08.001
|
Printer Friendly
Download PDF |



Daniel R. Lefebvre, MD | Division of Ophthalmic Plastic Surgery, Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Boston, Massachusetts Department of Ophthalmology, Harvard Medical School, Boston Sonya Dhar, MD | Department of Ophthalmology, New York University / New York Harbor Healthcare System, New York, New York Department of Ophthalmology, Moran Eye Center, Salt Lake City, Utah Irene Lee, MD | Division of Ophthalmology, Rhode Island Hospital, The Warren Alpert Medical School at Brown University, Providence Felicia Allard, MD | Department of Pathology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston Suzanne K. Freitag, MD | Division of Ophthalmic Plastic Surgery, Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Boston, Massachusetts Department of Ophthalmology, Harvard Medical School, Boston
|
|
|
| Abstract | Purpose
To investigate nonidiopathic causes of external dacryocystorhinostomy (DCR) failure.
Methods
The medical records of all patients with acute or chronic dacryocystitis who underwent external dacryocystorhinostomy performed by the senior author over a 5-year period were retrospectively reviewed, with attention to microbiology, pathology, and associated medical and history.
Results
A total of 52 lacrimal systems of 49 patients were included, with a minimum follow-up of 2 months (average, 15.5 months). Surgical success was achieved in 42 systems (87%). Of 7 failures, 6 had a condition potentially associated with an increased risk of failure, including MRSA infection, Gram-negative infection, rhinosinusitis, lymphoma, inflammatory bowel disease, and early loss of lacrimal stents.
Conclusions
External DCR is a successful procedure for the treatment of nasolacrimal obstruction associated with dacryocystitis. Various factors may affect surgical success, and awareness of these factors may enable better patient counseling and surgical planning. | | | Introduction | Dacryocystitis is most often the result of an acquired nasolacrimal duct stenosis leading to outflow obstruction and subsequent infection and inflammation of retained stagnant contents within the lacrimal sac.(1) The etiology of most cases of dacryostenosis is idiopathic, although it has been hypothesized to occur secondarily to an ascending inflammation from the nose and sinuses.(2,3) The signs of acute dacryocystitis include sudden onset of erythema, edema, and tenderness in the medial canthal area surrounding the lacrimal sac, which itself may be distended. Chronic dacryocystitis is a more indolent form of dacryocystitis, characterized by persistent, low-grade inflammation associated with mucopurulent discharge from the puncta; it is differentiated from simple nasolacrimal obstruction, in which there is epiphora but no sign of low-grade inflammation or discharge. The diagnosis of dacryocystitis establishes the diagnosis of nasolacrimal duct obstruction (NLDO).(4) Untreated, dacryocystitis is capable of progressing to a vision or life-threatening condition, because the infection may evolve to preseptal cellulitis, orbital cellulitis, meningitis, and even cavernous sinus thrombosis and death.(5)
The initial treatment of acute dacryocystitis may include topical and systemic antibiotics, with possible incision and drainage of the lacrimal sac, which serves the function of relieving lacrimal sac pressure and discomfort, evacuating what is essentially an abscess cavity, and providing material for microbiologic culture and sensitivity testing.(6,7) Definitive treatment is surgical. Although there have been many revisions and modifications to surgical technique, the underlying principle of surgical treatment, reestablishing patent communication between the lacrimal sac and the nasal cavity, has not changed since dacryocystorhinostomy (DCR) was introduced over 100 years ago in 1904 by Toti.(8)
Success rates for DCR, whether performed externally or endonasally, range from 69.9% to 100%, depending on many variables.(9,10) These success rates generally reflect DCR performed for cases of obstruction both with and without a history of dacryocystitis. In the present study, we reviewed a series of subjects, all of whom were diagnosed specifically with dacryocystitis (either acute or chronic) and who were treated via external DCR (ext-DCR). Cases that failed postoperatively were evaluated for possible associations that may be related to surgical failure with the goal of highlighting a pathophysiology for surgical failure that is not idiopathic. | | | Materials and Methods | This study was conducted with the approval of the Boston University Institutional Review Board, with acknowledgement by the Massachusetts Eye and Ear Infirmary Institutional Review Board. The medical records of consecutive patients undergoing ext-DCR performed by a single surgeon (SKF) from July 1, 2002, to December 31, 2008, at Boston Medical Center were retrospectively reviewed. The primary surgeon’s log was queried for patients who had undergone external dacryocystorhinostomy with an associated diagnosis of acute dacryocystitis (ADC) or chronic dacryocystitis (CDC). Patients who underwent ext-DCR for reasons other than dacryocystitis (eg, NLDO with epiphora but without signs or history ADC or CDC) were excluded. ADC was defined clinically as symptoms of fulminant lacrimal sac inflammation/infection, erythema, pain, and discharge for <2 weeks’ duration prior to initial presentation. CDC was defined clinically as the presence of chronic low-grade inflammation and associated discharge that had been ongoing or intermittent for >2 weeks’ duration.
Statistical Analysis
Data from included cases were entered into a spreadsheet (Microsoft Excel, Microsoft, Redmond, WA) for management and statistical analysis, which involved the χ2 test for sex and the t test for comparison of age and differences of preoperative duration of disease and surgical outcomes.
Surgical Technique
A standard ext-DCR procedure under general anesthesia was performed in all cases. The nasal cavity of the operative side was packed with 4% cocaine solution–soaked cottonoids, and 2% lidocaine with 1:100,000 epinephrine was injected subcutaneously in the medial canthal area. The skin was then incised with a #15 Bard-Parker blade, and blunt dissection was performed until the periosteum of the frontal process of the maxilla was identified, which was incised with a #15 Bard-Parker blade. A periosteal elevator was used to elevate the periosteum over the anterior lacrimal crest and into the lacrimal sac fossa, elevating the lacrimal sac and exposing the lacrimal bone. The lacrimal bone was infractured with a closed hemostat, with care taken to avoid violation of the nasal mucosa. A Kerrison rongeur was used to create an osteotomy of approximately 1 cm to 1.5 cm in diameter. The nasal mucosa was incised and anterior and posterior flaps were created. Insertion of Crawford-style, bicanalicular, silicone stents (FCI Ophthalmics, Marshfield Hills, MA) was performed after the superior and inferior puncta were dilated. The stylets were used to tent the lacrimal sac, and a #11 Bard-Parker blade was used to incise the sac, creating anterior and posterior flaps. The silicone stents were exteriorized through the nose. The anterior nasal and lacrimal sac mucosal flaps were anastomosed with 4-0 chromic gut. The Crawford-tube stylets were then passed through a silicone retinal sponge segment cut to approximately 1.5 cm in length to serve as an intranasal bolster to prevent postoperative stent prolapse. The incision was closed in two layers.
Postoperative Course
All patients were prescribed an oral antibiotic to be taken 4 times daily for 5 days after surgery (cefalexin 250 mg, unless the patient had a beta-lactam allergy, in which case ciprofloxacin or clindamycin was prescribed). If there were known culture results, antimicrobial therapy was directed appropriately according to sensitivity results. Erythromycin ophthalmic ointment was applied to the skin incision 3 times per day until the first follow-up appointment. Patients were seen at 1 week, 1 month, and 2 months after surgery and subsequently according to clinical course. Silicone stents were removed at the 2-month follow-up appointment. No patients were prescribed steroids of any type. Surgical success was defined by resolution of infection and a lack of symptoms, such as epiphora. Surgical failure was defined as persistence or recurrence of dacryocystitis or epiphora. | | | Results | A total of 54 adult patients were identified who met the inclusion criteria. Of these, 4 underwent bilateral surgery, yielding a total of 58 nasolacrimal systems. Five patients (1 bilateral) were excluded for inadequate follow-up, bringing the total number of patients to 49, with 52 nasolacrimal systems. The average follow-up time was 15.5 months ± 17.6 (range, 2-74 months).
Of the 49 patients, 43 were female (88%; P = 0.00000013 [?2]). The average age for male patients was 50.8 years ± 23.0 (range, 31-78); for females, 61.5 ± 19.6 (range, 17-89). The average age for all patients combined was 60.2 years; there was no statistically significant difference between the age of males and females (P = 0.30).
Acute dacryocystitis was present in 14 patients (13 females). CDC was present in 30 females and 5 males, for an overall total of 35 patients with chronic disease (70%).
Bilateral cases occurred in 2 females and 1 male. Right-sided procedures were conducted in 28 females and 3 males; left-sided procedures, in 18 females and 3 males. There was no statistically significant difference in laterality among females (P = 0.14 [?2]) or males.
Microbial cultures were obtained from 19 lacrimal systems (39%) that were found to have purulence in the lacrimal sac at the time of surgery. Culture results were polymicrobial in 7 and monomicrobial in 11. A single case demonstrated no growth (an 83-year-old female with a preoperative diagnosis of CDC). There were 10 Gram-positive isolates (53% of total systems cultured) and 14 Gram-negative isolates (74% of total systems cultured), as well as a single identified yeast (Table 1). The most common Gram-positive pathogen was Staphylococcus aureus (5 cases), followed by Streptococcal species (3) and Propionibacterium acnes (2). The most common Gram-negative pathogen was Haemophilus influenzae (5 cases), followed by Proteus mirabilis (2), Pseudomonas aeruginosa (2), and others. Within the S. aureus isolates were 3 cases of methicillin-resistant Staphylococcus aureus (MRSA): (1) an 89-year-old institutionalized female with CDC, type 2 diabetes mellitus, polio, and psychiatric illness; (2) a 51-year-old female Palestinian immigrant with CDC of 5-years’ duration; (3) a 73-year-old male with CDC who underwent functional endoscopic sinus surgery approximately 1 year prior to presentation.
Tissue samples were obtained for histopathologic analysis in 30 lacrimal systems (61%). Chronic inflammation was seen in 26 samples (87%). Of these, 7 cases were specifically associated with dense fibrotic tissue, 1 case with a giant-cell foreign body reaction and 1 case with a dacryolith. Two specimens were of loose connective tissue, without evidence of inflammation. A single case showed mild acute inflammatory changes. One case demonstrated a lymphoid infiltrate consistent with lymphoma in a patient with known systemic lymphoma.
Of 52 lacrimal systems, 45 (87%) had a successful surgery, defined as postoperative absence of dacryocystitis and epiphora. Symptoms recurred in 7 cases (13% [6 females]). Laterality was split, with 3 right sides and 4 left sides. The details of the recurrent cases, including disease duration, microbiology, and histopathology when available, and relevant past medical, surgical, and social history are presented in Table 2 and detailed below.
Recurrent Cases
Case 1
An 89-year-old female nursing home resident with a history of type 2 diabetes mellitus, psychiatric illness, polio, and osteomyelitis, who had right-sided intermittent CDC of 4 months’ duration per history, developed an associated preseptal cellulitis and on presentation to the oculoplastics clinic was treated with incision and drainage. Culture revealed MRSA. She was treated with oral trimethoprim/sulfamethoxazole preoperatively and underwent ext-DCR approximately 4 months following presentation. Lacrimal sac biopsy demonstrated dense fibroconnective tissue with minimal chronic inflammatory changes. Two months postoperatively, she developed a recurrence of dacryocystitis. She underwent revision surgery 5 months after her initial operation; intraoperative cultures again returned MRSA. Following her second procedure, she has been without recurrence for 55 months postoperatively.
Case 2
A 40-year-old healthy woman with a 2-month history of left-sided epiphora followed by a 3-day history of discharge and redness was diagnosed with acute dacryocystitis. She received a 2-week course of cefalexin and underwent ext-DCR 3 months after initial presentation. Intraoperative cultures were not obtained and mucosal biopsy was not performed. The patient was without problems at postoperative month 6 and did not return for further follow-up until she developed tearing and discharge at 34 months postoperatively. Revision surgery was performed and the patient was without symptoms of tearing or infection at postoperative month 6. Intraoperative cultures and tissue samples were not obtained during the revision surgery.
Case 3
A 51-year-old female Palestinian immigrant with hypertension presented with a 5-year history of right-sided tearing and intermittent discharge and low-grade inflammation, consistent with CDC. Culture at presentation revealed MRSA and Strep. viridans. The patient received a course of Bactrim and ext-DCR was performed 2 months following presentation. Intraoperative cultures demonstrated no growth. Pathology specimens were not obtained. She presented at postoperative month 15 with recurrence of CDC and underwent revision surgery 20 months after initial DCR. Tissue samples showed chronic inflammation and intraoperative cultures revealed H. influenzae. She was without tearing or discharge at the time of silicone stent removal at postoperative month 2.
Case 4
A 59-year-old healthy woman presented with a 4-year history of left-sided tearing, discharge, and inflammation, consistent with CDC. Computed tomography (CT) revealed mild pansinusitis (mucosal thickening). She underwent evaluation with an otolaryngologist, who advised a steroid nasal spray. Ext-DCR was performed 5 months later. Cultures were not obtained. Histopathology was consistent with chronic inflammatory infiltrate. Epiphora returned 3 months postoperatively, but she deferred further surgical treatment.
Case 5
An 87-year-old woman with a history of right-sided endoscopic DCR performed by another surgeon 3 years previously had persistent epiphora and lacrimal sac enlargement, with intermittent punctal discharge and inflammation. Preoperative culture of the discharge revealed P. aeruginosa and E. coli. Histopathology following external revision DCR demonstrated dense fibrous tissue, with chronic inflammatory changes consistent with her presentation of CDC. Her symptoms returned within one month of surgery, and she opted for medical management only with oral antibiotic therapy.
Case 6
An 83-year-old woman with a history of lymphoma and breast cancer had undergone radiation therapy and tamoxifen treatment. She presented with left-sided, acute dacryocystitis and was treated preoperatively with amoxicillin/clavulanate empirically. One month after presentation, she underwent ext-DCR. Cultures grew Citrobacter freundii and P. aeruginosa, and histopathology demonstrated chronic inflammation despite the patient’s apparent acute presentation. The patient did well until 35 months postoperatively, when she developed epiphora and mild purulent punctal discharge bilaterally. She declined further intervention.
Case 7
A 33-year-old man with a history of Crohn disease and lymphoma presented with a many-year history of left-sided tearing and discharge. Initial cultures and subsequent intraoperative cultures obtained several weeks later demonstrated no growth. The bicanalicular silicone stents placed at the time of ext-DCR “fell out” at postoperative week 4. He had a recurrence of symptoms and underwent surgical revision at postoperative month 8. Intraoperative cultures from the second surgery revealed Strep. pneumoniae. Biopsied lacrimal sac tissue demonstrated signs of chronic inflammation. The silicone stenting remained in place until removal at postoperative month 2. He remained without symptoms or signs of recurrence at postoperative month 3. | | | Discussion | The overall 87% success rate of ext-DCR in this series and the high proportion of female patients with NLDO and dacryocystitis (88%) are comparable to previous reports.(9,11-15) Of the 7 cases of recurrent dacryocystitis after DCR, 2 were associated with MRSA infection, 2 were associated with Gram-negative bacteria, 2 carried an associated diagnosis of lymphoma, 2 demonstrated very dense fibrosis of the lacrimal sac on histopathology, 1 had background pansinusitis demonstrated on CT, 1 had a history of inflammatory bowel disease; 1 had a history of prior endoscopic DCR performed 3 years previously; and 1 had a loss of canalicular stents relatively early in the postoperative course. Only case 2 had no associated systemic illnesses or perioperative events to possibly explain an increased risk of recurrence, although this case did not have cultures or biopsy performed, and it is therefore possible that an underlying causative pathology could have been missed.
Dacryocystitis represents an infection within the lacrimal sac. Although postoperative DCR wound infection is quite rare, such infection is associated with an increased risk of surgical failure.(14,12) The final postoperative intranasal ostium size following ext-DCR averages 1.8 mm in diameter.(16) The primary anatomic cause of DCR failure has been observed to be the formation of intranasal soft tissue adhesions.(17) It therefore seems reasonable that the presence of bacterial colonization and increased inflammation may contribute to closure of the nasal ostium via stenosis and adhesion formation.
Evidence has shown that postoperative DCR patients treated with antibiotic therapy have significantly lower rates of postoperative wound infections.(12,18) Whether all patient undergoing DCR require systemic antibiosis is debated. A recent large study of 697 external DCRs found that prophylactic intravenous antibiotic therapy at the time of surgery may be of benefit only in cases associated with a history of mucocele, mucopyocele, or frank dacryocystitis, because these cases were found to have a higher rate of positive intraoperative culture.(19)
It is the preference of the senior author to treat all cases of acute dacryocystitis medically with oral antibiotics for 2 weeks prior to any surgical intervention to reduce the underlying infection and quiet inflammation prior to embarking on surgery. Some authors have proposed dacryocystorhinostomy, most recently using endoscopic dacryocystorhinostomy, as a direct treatment for acute dacryocystitis.(20) In their multicenter retrospective review of 18 patients with acute dacryocystitis treated via endo-DCR, Madge et al reported a 94.4% success with an average of 12 months’ follow-up.(20) It should be noted, though, that all patients received either oral or intravenous antibiotics for an average of 5 days prior to surgery, with 66.7% having documented clinical improvement prior to surgery.
Knowledge of the most common organisms associated with dacryocystitis is helpful in directing empiric therapy. In the present series, among surgical failures with available bacterial culture results, there were 2 cases with Gram-negative bacteria and 2 with MRSA. A national multicenter prospective study of 89 patients examined the microbiologic spectrum of acute and CDC.(10) The majority of isolates were Gram-positive species; the most common pathogen isolated was Staphylococcus aureus (28.8%). Of these, 21% were MRSA. Further, a significant proportion of cases (28.9%) were not sensitive to the initial empiric antibiotic agent chosen. Lacrimal surgery was performed in 93% of all cases, and a success rate of 100% was reported, although the follow-up time was not stated.(10) There are other examples of successful DCR performed in the setting of MRSA, which is notable because the incidence of MRSA is ever increasing.(6,21,22) Freidlin et al reported an increase in the proportion of S. aureus eye infections that were MRSA, starting from 4.1% in 1998 and increasing to 16.7% in 2005.(23) A case series by Kotlus et al examined MRSA-associated dacryocystitis specifically.(22) Patients were treated preoperatively with combinations of oral linezolid and topical fortified vancomycin eyedrops. With this therapy, the authors reported 100% success in the 3 patients who underwent DCR and 100% failure in 4 patients who were unable to have surgery. Certainly there can be successful DCR outcomes in the presence of MRSA, and even in the present study there was a case associated with MRSA that was successful. It is likely, however, that in most cases of MRSA, empiric antibiotics are not effective, allowing a subclinical infection to persist in the immediate postoperative period that incites inflammation and contributes to adhesion formation, ostium closure, and subsequent surgical failure. There are known associations that increase a person’s risk for MRSA colonization, including recent hospitalization or recent outpatient clinic visit, nursing home residence, history of intravenous drug usage, history of antibiotic usage, and chronic illness.(24) By noting these associated risk factors, it may be possible to identify patients who may be more appropriately treated with a nonstandard empiric antibiotic regimen or patients who should be screened for MRSA and considered for direct early antibiotic coverage early (either clindamycin or trimethoprime/sulfamethoxazole). We advise allowing sufficient time for antibiotic treatment to be effective and for all active inflammation to settle prior to lacrimal surgery in these patients.
There may also be an increase in the prevalence of Gram-negative bacteria associated with dacryocystitis, particularly outside the US. Hartikainen et al showed a 16.7% Gram-negative prevalence in their studied samples from patients with lacrimal duct obstructions in Finland, the most common Gram-negative bacterium being H. influenza.(11) Badhu et al found 18.7% Gram-negative prevalence in their cross-sectional study of CDC in Nepal.(25) CDC was associated with Gram-negative bacteria 26% of the time in a study from Saudi Arabia, with one-third of the Gram-negative isolates being H. influenza.(26) The most significant Gram-negative presence has been reported by Briscoe et al, with 61% Gram-negative isolates in patients with purulent dacryocystitis in Israel.(27) In that study, the most common bacterium was P. aeruginosa, accounting for 22% of all isolates (ie, including Gram positive and Gram negative combined).(27) The authors noted frequent resistance of the Gram-negative bacteria to the antibiotic agents routinely selected for empiric therapy in dacryocystitis.(26,27) US data from Mills et al showed a 28.7% prevalence of Gram-negative bacteria, with P. aeruginosa being the most frequent.10 In the present study, Gram-negative bacteria were found in 74% of the lacrimal systems cultured, with the most frequent being Haemophilus influenzae, followed by P. aeruginosa and P. mirabilis. Case 3 was associated with H. influenzae (after previously being MRSA positive at the time of initial surgery). Case number 5 was associated with the Gram negatives P. aeruginosa and E. coli. Cephalexin was the most commonly empirically prescribed antibiotic in the present series, and this first-generation cephalosporin has broad Gram-positive coverage (excluding MRSA) and does have some activity against H. influenzae, the most commonly encountered Gram-negative bacterium in this series. Cephalexin has little activity against pseudomonas species and E. coli, however. Therefore, it is reasonable to prescribe cephalexin (or alternatively amoxicillin / clavulanate) as a first-line empiric agent to treat dacryocystitis; however, cultures should be routinely obtained (either from punctal discharge or from incision and drainage of the lacrimal sac for acute dacryocystitis) and antimicrobial therapy expediently altered if indicated based on culture results.
Selection bias may have contributed to the relatively high proportion of Gram-negative isolates identified in the present study. Cases that appeared “worse” or had more discharge may have prompted culture over cases without such a clinical picture. Hartikainen et al showed that there is a qualitative difference in the purulent discharge found in Gram-negative cases of dacryocystitis (being more copious and thicker) in comparison to Gram-positive infections.(11) It is possible that this thicker discharge may contribute to the surgical site milieu and could potentially cause persistent inflammation and adhesion formation during the postoperative period following DCR. Another aspect of Gram-negative infection is that frequently empiric antibiotics (first-generation cephalosporin in the present study) are relatively ineffective against Gram-negative organisms. The presence of a relatively thick and copious discharge could therefore direct the clinician to potentially select an empiric antimicrobial with greater Gram-negative coverage while awaiting culture results.
Inflammation may also be associated with lacrimal obstruction as well as with lacrimal surgery failure. Inflammatory bowel disease (IBD)—either Crohn disease or ulcerative colitis—has been documented to have an increased association with lacrimal drainage obstruction. McNabb et al showed a higher prevalence of IBD (2%) in a cohort of patients with lacrimal drainage obstruction compared to the estimated prevalence in the general Australian population (0.3%).(28) When the outcomes of 9 post-DCR patients with IBD were assessed, there was 1 case with partial success and 1 with recurrence of symptoms within the first postoperative year.(28) There was also a high prevalence of sino-nasal disease among these patients, 2 of whom showed significant sinus disease on CT.(28) In fact, granulomatous inflammatory changes have been directly observed in the conjunctiva and nasal mucosa of patients with Crohn disease.(29,30) The overall prevalence of sinonasal disease has been reported to be as high as 48% in patients with IBD.(31) It is plausible that since increased sinonasal inflammation appears to play a role in the development of lacrimal system obstruction, it may also play a role in post-DCR failure. In the present study there was a failed surgery in a patient with chronic pansinusitis identified on CT and a patient with Crohn disease.
The lacrimal drainage system functions as a mucosal-associated lymphoid tissue and is thus capable of harboring malignant hematologic neoplasms and lymphoid infiltrates.(32) Such infiltration can cause lacrimal drainage system obstruction.(33) Obstruction may be unilateral or bilateral, as occurred during the post-DCR time-period for case 6 in the present study. Slonim and Older documented a case of bilateral DCR failure in a patient with a history of chronic lymphocytic leukemia; the case was peculiar in that the patient with leukemia had the development of biopsy-proven solid lymphoma at both DCR sites.(34) It is important to maintain vigilance in patients with a history of such malignancy. A biopsy of the lacrimal tissue at the time of DCR may reveal active disease in someone thought to be in remission.
There is debate regarding whether routine biopsy of lacrimal sac or nasal mucosal tissue is indicated at the time of DCR. Anderson et al analyzed 377 DCR lacrimal sac specimens and found 85% non-granulomatous inflammation.(35) The next most common pathology was sarcoidosis (2.1%), followed by lymphoma (1.9%).(35) More unusual neoplasms occurred in isolation. Previously undiagnosed malignancies were diagnosed in 2.1% of cases, and the authors concluded that routine biopsy of lacrimal sac tissue ought to be performed during all cases of DCR surgery.(35) A later prospective study of 193 consecutive endoscopic DCR lacrimal sac specimens found non-specific inflammation in 76% and normal results in 23%; only 1.2% had a specific pathology. The authors concluded that routine biopsy should not be performed.(36) The present study had similar rates of bland inflammatory changes in lacrimal sac samples, with only a single, specific pathology identified (lymphoma); interestingly, not in one of the recurrent dacryocystitis cases. Specific pathologies, while rare in relation to the majority of lacrimal system stenosis cases, do exist and can be found on tissue biopsy performed during DCR, such as a recently reported case of bilateral nasopharyngeal amyloidosis.(37) It therefore seems prudent to leave the decision of whether or not to biopsy to the discretion of the operating surgeon, who can relate the clinical picture to the patient’s history.
Lacrimal intubation in DCR surgery has a varied history and is also the subject of some debate.(38) The senior author prefers to place a silicone lacrimal stent at the time of DCR in all cases, and this is routinely removed at postoperative month 2. Case 7 in the present study, associated with Crohn disease and lymphoma, was further confounded by an early loss of bicanalicular stenting. Sodhi et al reviewed 25 cases of patients at high-risk for DCR failure; all cases were stented, and 100% postoperative success was achieved when the stents remained in place for at least 6 months, while there were 2 failures occurring with loss of stents at postoperative week 3 and 1 failure with loss of stents at postoperative month 3.(39) Case 7 in our study could have been considered at high risk for DCR failure given his past medical history, and it is possible that his early loss of lacrimal stenting contributed to the failure.(3)
The present study is limited by the relatively short follow-up period and by other weaknesses inherent to a retrospective review (eg, selection bias, nonuniform interventions, etc). Postoperative lacrimal irrigation was not performed in all subjects, because it is the senior author’s practice to not instrument lacrimal systems in patients who are without complaint or signs of epiphora because doing so exposes them to unnecessary procedural intervention. Intraoperative tissue biopsy was not performed in all cases in this retrospective study; however, 100% tissue analysis may be considered advisable in a future prospective study.
In conclusion, ext-DCR is a successful treatment for patients with acute or chronic dacryocystitis; however, there are certain identifiable factors that may affect the surgical outcome. Furthermore, there is still debate regarding optimal surgical technique and the effect of various perioperative factors on surgical outcome. One problem is that the literature displays a wide range in outcome assessments and follow-up timeframes. There is a significant inverse correlation between DCR success-rate and length of follow-up.(15) Variables have been highlighted in the present study that surgeons may wish to consider when counseling and treating patients with dacryocystitis, and these topics deserve further review. | | | References | 1. Olver J, ed. Color Atlas of Lacrimal Surgery. Oxford: Butterworth-Heinemann; 2001:2-23.
2. DeAngelis D, Hurwitz J, Oestreicher J, Howarth D. The pathogenesis and treatment of lacrimal obstruction: the value of lacrimal sac and bone analysis. Orbit 2001;20:163-72.
3. Traquair H. Chronic dacryocystitis: its causation and treatment. Arch Ophthalmol 1941;26:165-80.
4. Nerad, JA. Techniques in Ophthalmic Plastic Surgery with DVD: A Personal Tutorial. Philadelphia: Saunders; 2010:267.
5. Mauriello JA, Wasserman BA. Acute dacryocystitis: an unusual cause of life-threatening orbital intraconal abscess with frozen globe. Ophthal Plast Reconstr Surg 1996;12:2945.
6. Cahill KV, Burns JA. Management of acute dacryocystitis in adults. Ophthal Plast Reconstr Surg 1993;9:38-41; discussion 42.
7. Barrett RV, Meyer DR; ASOPRS Acquired Lacrimal Fistula Study Group. Acquired lacrimal sac fistula after incision and drainage for dacryocystitis: a multicenter study. Ophthal Plast Reconstr Surg 2009;25:455-7.
8. Toti A. Nuovo metodo cormervatore di cad/tale suppttrazioni croniehe de1 8a? o lacrimale (dacrioeis—toriocotomla). Clin Mod Pisa; 1904.
9. Yigit O, Samancioglu M, Taskin U, Ceylan S, Eltutar K, Yener M. External and endoscopic dacryocystorhinostomy in chronic dacryocystitis: comparison of results. Eur Arch Otorhinolaryngol 2007;264:879-85.
10. Mills DM, Bodman MG, Meyer DR, Morton AD; ASOPRS Dacryocystitis Study Group. The microbiologic spectrum of dacryocystitis: a national study of acute versus chronic infection. Ophthal Plast Reconstr Surg 2007;23:302-6.
11. Hartikainen J, Lehtonen OP, Saari KM. Bacteriology of lacrimal duct obstruction in adults. Br J Ophthalmol 1997;81:37-40.
12. Walland MJ, Rose GE. Factors affecting the success rate of open lacrimal surgery. Br J Ophthalmol 1994;78:888-91.
13. Heindl LM, Junemann A, Holbach LM. A clinicopathologic study of nasal mucosa in 350 patients with external dacryocystorhinostomy. Orbit 2009;28:7-11.
14. Dolman PJ. Comparison of external dacryocystorhinostomy with nonlaser endonasal dacryocystorhinostomy. Ophthalmology 2003;110:78-84.
15. Erdöl H, Akyol N, Imamoglu HI, Sözen E. Long-term follow-up of external dacryocystorhinostomy and the factors affecting its success. Orbit 2005;24:99-102.
16. Linberg JV, Anderson RL, Bumsted RM, Barreras R. Study of intranasal ostium external dacryocystorhinostomy. Arch Ophthalmol 1982;100:1758-62.
17. Warren JF, Seiff SR, Kavanagh MC. Long-term results of external dacryocystorhinostomy. Ophthalmic Surg Lasers Imaging 2005;36:446-50.
18. Hurley LD, Westfall CT, Shore JW. Prophylactic use of antibiotics in oculoplastic surgery. Int Ophthalmol Clin 1992;32:165-78.
19. Pinar-Sueiro S, Fernández-Hermida R-V, Gibelalde A, Martínez-Indart L. Study on the effectiveness of antibiotic prophylaxis in external dacryocystorhinostomy: a review of 697 cases. Ophthal Plast Reconstr Surg 2010;26:467-72.
20. Madge SN, Chan W, Malhotra R, et al. Endoscopic dacryocystorhinostomy in acute dacryocystitis: a multicenter case series. Orbit 2011;30:1-6.
21. Kubo M, Sakuraba T, Arai Y, Nakazawa M. Dacryocystorhinostomy for dacryocystitis caused by methicillin- resistant Staphylococcus aureus: report of four cases. Jpn J Ophthalmol 2002;46:177-82.
22. Kotlus BS, Rodgers IR, Udell IJ. Dacryocystitis caused by community-onset methicillin-resistant Staphylococcus aureus. Ophthal Plast Reconstr Surg 2005;21:371-5.
23. Freidlin J, Acharya N, Lietman TM, Cevallos V, Whitcher JP, Margolis TP. Spectrum of eye disease caused by methicillin-resistant Staphylococcus aureus. Am J Ophthalmol 2007;144:313-5.
24. Salgado CD, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis 2003;36:131-9.
25. Badhu BP, Karki BS, Khanal B, Dulal S, Das H. Microbiological patterns of chronic dacryocystitis. Ophthalmology 2006;113:2377.e1-2.
26. Chaudhry IA, Shamsi FA, Al-Rashed W. Bacteriology of chronic dacryocystitis in a tertiary eye care center. Ophthal Plast Reconstr Surg 2005;21:207-10.
27. Briscoe D, Rubowitz A, Assia EI. Changing bacterial isolates and antibiotic sensitivities of purulent dacryocystitis. Orbit 2005;24:95-8.
28. Satchi K, McNab AA. Lacrimal obstruction in inflammatory bowel disease. Ophthal Plast Reconstr Surg 2009;25:346-9.
29. Blase WP, Knox DL, Green WR. Granulomatous conjunctivitis in a patient with Crohn's disease. Br J Ophthalmol 1984;68:901-3.
30. Kinnear W. Crohn’s disease affecting the nasal mucosa. J Otolaryngol 1985.
31. Book DT, Smith TL, McNamar JP, Saeian K, Binion DG, Toohill RJ. Chronic sinonasal disease in patients with inflammatory bowel disease. Am J Rhinol 2003;17:87-90.
32. Linberg JV ed. Lacrimal Surgery. Contemporary Issues in Ophthalmology. Vol. 5.New York, Churchill Livingstone; 1988:348.
33. Yip C-C, Bartley GB, Habermann TM, Garrity JA. Involvement of the lacrimal drainage system by leukemia or lymphoma. Ophthal Plast Reconstr Surg 2002;18:242-6.
34. Slonim CB, Older JJ. Bilateral lymphocytic infiltrates causing dacryostenosis after bilateral successful dacryocystorhinostomies. Ophthal Plast Reconstr Surg 1988;4:105-8.
35. Anderson NG, Wojno TH, Grossniklaus HE. Clinicopathologic findings from lacrimal sac biopsy specimens obtained during dacryocystorhinostomy. Ophthal Plast Reconstr Surg 2003;19:173-6.
36. Merkonidis C, Brewis C, Yung M, Nussbaumer M. Is routine biopsy of the lacrimal sac wall indicated at dacryocystorhinostomy? A prospective study and literature review. Br J Ophthalmol 2005;89:1589-91.
37. Geller E, Freitag SK, Laver NV. Localized nasopharyngeal amyloidosis causing bilateral nasolacrimal duct obstruction. Ophthal Plast Reconstr Surg 2011;27:e64–7.
38. Madge SN, Selva D. Intubation in routine dacryocystorhinostomy: why we do what we do. Clin. Experiment. Ophthalmol 2009;37:620-3.
39. Sodhi PK, Pandey RM, Malik KPS. Experience with bicanalicular intubation of the lacrimal drainage apparatus combined with conventional external dacryocystorhinostomy. J Craniomaxillofac Surg 2003;31:187-90. | |
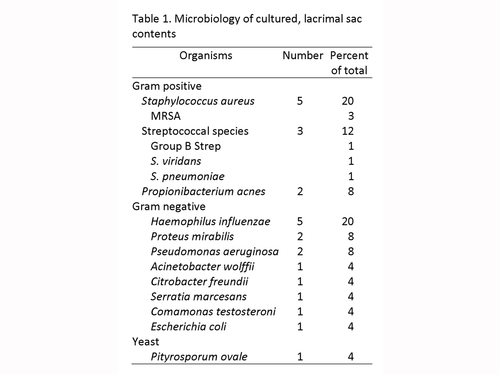
Table 1
Microbiology of cultured, lacrimal sac contents
|
|
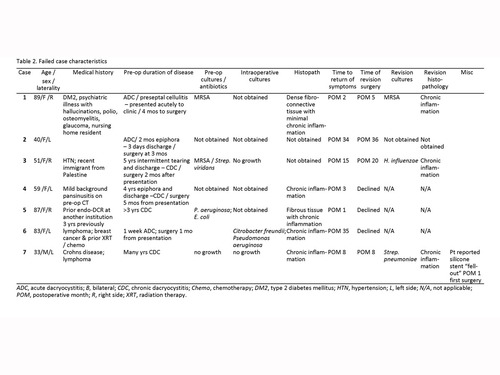
Table 2
Failed case characteristics
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in