|
|
 |
 |
 |
 |
|
|
Effects of augmented tenotomy and reattachment in the infantile nystagmus syndrome
Digital Journal of Ophthalmology 2016
Volume 22, Number 1
March 31, 2016
DOI: 10.5693/djo.01.2016.01.002
|
Printer Friendly
Download PDF |


 Louis F. Dell’Osso, PhD
Louis F. Dell’Osso, PhD | Daroff-Dell’Osso Ocular Motility Laboratory, Louis Stokes Cleveland Department of Veterans Affairs Medical Center, and Case Medical School, Cleveland, Ohio; Department of Neurology, Case Western Reserve University and University Hospitals, Case Medical Center, Cleveland, Ohio Faruk H. Orge, MD | Department of Ophthalmology, Case Western Reserve University and University Hospitals Case Medical Center, Cleveland, Ohio Jonathan B. Jacobs, PhD | Daroff-Dell’Osso Ocular Motility Laboratory, Louis Stokes Cleveland Department of Veterans Affairs Medical Center and CASE Medical School, Cleveland, Ohio; Departments of Neurology and Biomedical Engineering, Case Western Reserve University and University Hospitals Case Medical Center, Cleveland, Ohio
|
|
|
| Abstract | Purpose
To test the hypothesis that augmented tenotomy and reattachment surgery (AT-R), which involves placing an additional suture in each distal tendon during the 4-muscle tenotomy and reattachment (T-R) or other infantile nystagmus syndrome (INS) procedures, could increase the beneficial effects of many types of extraocular muscle (EOM) surgery to treat INS.
Methods
Both infrared reflection and high-speed digital video systems were used to record the eye movements in 4 patients with INS before and after AT-R surgery. Data were analyzed using the eXpanded Nystagmus Acuity Function (NAFX) that is part of the OMtools software.
Results
Placement of the augmentation suture did not interfere with Kestenbaum, Anderson, bilateral medial rectus muscle recession, or T-R surgeries. The therapeutic effects of AT-R were similar to but not equal to those from the traditional single-suture surgeries (ie, broadening longest foveation domain [LFD] but no improvement of NAFX peak). The average of the NAFX percent improvements after AT-R was within 31% of those estimated from NAFX values before T-R; the average of the percent broadenings of the LFD values after AT-R was within 16%.
Conclusions
The AT-R does not improve the foveation quality in INS above the traditional T-R surgery. It is not improved by an additional suture; indeed, some improvements may be diminished by the added suture. The hypothesized augmented-tendon suture technique (sans tenotomy) has been modified and remains to be tested.
| | | Introduction | | Our understanding of the surgical treatment of infantile nystagmus syndrome (INS) has benefitted from the past several decades of ocular motility studies and analyses.(1) Recently, two hypothetical modifications to the 4-muscle tenotomy and reattachment (T-R) procedure have been suggested: (1) an augmented T-R procedure (AT-R); and (2) the augmented tendon suture (ATS, sans tenotomy) procedure. It has been speculated that with the former modification the beneficial effects of the T-R procedure might be increased by placement of additional sutures in the distal tendon of each operated extraocular muscle; in the case of the latter modification, simply placing sutures in the distal tendons, without performing the tenotomies, might produce the same therapeutic improvements.(2) This preliminary study tests the first modification of the T-R procedure: values of peak eXpanded Nystagmus Acuity Function (NAFXpk) and longest foveation domain (LFD) before and after AT-R are compared to estimated values of the NAFXpk and LFD with the single-suture T-R procedure.(3) Based on our findings, the authors make suggestions for testing the second ATS procedure. | | | Materials and Methods | Protocol
This study was approved by the Case Western Reserve University Hospitals Institutional Review Board. Written consent was obtained from all subjects before testing. All procedures were carefully explained to subjects before the experiment began and were reinforced during the trials. Subjects were seated in a chair with a headrest and either a bite board or a chin stabilizer far enough from an arc of red light-emitting diodes (LED) to prevent convergence effects (>5 feet). At this distance, each LED subtended <0.1° of visual angle. The room light could be adjusted from dim to blackout in order to minimize extraneous visual stimuli. An experiment consisted of 1-10 trials, each lasting <1 minute, with time allowed between trials for the subject to rest. Trials were kept short to guard against boredom, because INS intensity is known to decrease with inattention.
Recording
A high-speed digital video system was used for the eye-movement recording. The system (EyeLink II, SR Research, Mississauga, ON, Canada) has a linear range of ±30° horizontally and ±20° vertically. System sampling frequency was 500 Hz with 16-bit resolution, and gaze position accuracy error was 0.5° to 1° on average. The signal from each eye was calibrated with the other eye behind cover to obtain accurate position information; the foveation periods were used for calibration. Eye positions and velocities (obtained by analog differentiation of the position channels) were displayed on a strip chart recording system (Beckman Type R612 Dynograph). The total system bandwidth (position and velocity) was 0-100 Hz. The data were digitized at 400 Hz with 12-bit resolution. Some horizontal eye movement recordings were made using infrared reflection (Applied Scientific Laboratories, Waltham, MA). In the horizontal plane, the system was linear to ±20° and monotonic to ±25-30° with a sensitivity of 0.25°. Monocular primary position adjustments for both methods allowed accurate position information and documentation of small tropias and phorias hidden by the nystagmus. It also ensured that it was the fixating eye that was being analyzed, especially when the subject switched fixation from one eye to the other. All recordings were performed without refraction. In our experience the saccadic or smooth-pursuit gains of a bright laser spot are not affected by a subject’s refraction.
Analysis
Data were analyzed using the MATLAB environment (The MathWorks, Natick, MA) and OMtools software (available from http://www.omlab.org). Only eye position was sampled directly; velocity data for analysis was obtained from the sampled position data by a central-point differentiator with n = 3 (ie, using third points pre- and post-center). Position data were low-pass filtered with a 4th-order Butterworth filter, with the cutoff frequency of 50 Hz to reduce the noise while minimally affecting the saccades. Data were filtered forward and backward to eliminate phase distortion. Analysis was always done on the fixating eye. Segments recorded during inattention, changes in the fixating eye, or blinking were not used for this analysis.
The eXpanded Nystagmus Acuity Function (NAFX) was used to measure foveation changes induced by T-R in the nystagmus at primary position and various gaze angles to determine the peak value (NAFXpk) and the LFD (ie, the range of gaze angles between the 90%-NAFXpk points).(3-5) The NAFX is an objective and repeatable measure of INS waveform foveation quality that is directly proportional to potential Snellen decimal visual acuity in patients with no additional visual sensory deficits and the post-therapy changes of which are directly proportional to visual acuity changes in all INS patients, irrespective of the presence of afferent visual sensory deficits.(6-10) (As shown in the figures of Hertle and Dell’Osso, chapter 7,(11) the NAFX program provided age-corrected visual acuities as a comparison.) Details of the NAFX’s theory and application may be found elsewhere.(3) In the present study, each plotted NAFX point represents an average of several independent fixations, each consisting of 3-10 cycles (1-3 seconds) of steady foveation immediately following target acquisition.(12) All analyses adhered to long-established and refined procedures in our laboratory.
For subject 3, we estimated the postoperative improvements based on the NAFX during convergence required by a near target of about 14 prism diopters (PD) convergence (mimicking the 7 PD base-out prism) and also on the measured difference in the patient’s pre- and postoperative esophoria. The latter is a measure of the additional convergence that would be required by the surgery.
Patients’ Clinical and INS Characteristics
Four patients with INS received complete pre- and postoperative clinical examinations, including fundus examinations, refractions, strabismus evaluations, and best-corrected visual acuities. Table 1 summarizes the clinical findings.
Subject 1 was an 8-year-old boy with septo-optic dysplasia and bilateral optic nerve hypoplasia. His visual acuity was worse in the right (counting fingers at 5 feet) than in the left eye (20/80 = 0.25). He had a right head turn (left-gaze fixation) and no transillumination of the iridies. Eye movement recordings confirmed a biplanar INS (diagonal up-left and down-right), with a greater horizontal component. Left eye fixation was much better than right eye fixation at all gaze angles. Despite that, there were transient periods of right-eye fixation during binocular recordings. His INS waveforms were pendular (P), pendular with foveating saccades (Pfs), jerk (J), jerk with extended foveation (Jef), pseudocycloid (PC), pseudo-jerk (PJ), and pseudo-pendular with foveating saccades (PPfs). Superimposed on some of the INS waveforms was a high-frequency (4-5 Hz), low-amplitude, pendular nystagmus producing a dual-jerk (DJ) waveform. At one point, there was a large jerk left nystagmus, suggesting a long-period, very asymmetric aperiodic alternating nystagmus (APAN). However, he exhibited a right head turn and had better control of his nystagmus in left gaze. Using the Titmus stereopsis test, his stereoacuity was 140 arcsec, with a left eye preference, although it had previously been thought to be poorer than 1600?.
Because of the variable nature of the INS (sometimes 40°-50° peak-to-peak) and inability to maintain fixation with his left eye, a 2-plane 4-muscle approach with the possibility of an augmented suture technique was initially recommended to damp the INS and allow better foveation. A staged surgical approach was taken. First, the four horizontal rectus muscles would be performed (preferably a Kestenbaum but possibly a T-R procedure); if necessary after 4-6 months, the four vertical rectus muscles would receive similar treatment. This type of staged surgery has been performed on both canines and patients with INS without causing anterior segment ischemia. Because the main component of this patient’s INS was horizontal, and the surgery was performed on the horizontal rectus muscles, eye movement analysis was restricted to the horizontal component.
Subject 2 was a 23-year-old man who was previously recorded at the age of 14 along with his 11-year-old brother, who also had hereditary INS. He had a latent component, a small, variable strabismus, and a left head turn (right gaze fixation). His INS waveforms were Pfs, J, Jef, PC, PJ, and PPfs. There was no stereopsis. A Kestenbaum procedure was recommended to rotate his eyes 20° to the left, thereby shifting peak-foveation waveforms rightward to primary position.
Subject 3 was a 23-year-old man with INS who was about to enter law school. His waveforms were P and Pfs. His INS damped significantly with convergence. A trial with 7 PD base-out prisms and ?1.00 diopters added to his refraction was recommended prior to performing a bilateral medial rectus recession plus bilateral AT-R. After successfully using the trial prisms during his first semester in law school, he elected to have the surgery. Although we had concluded that a bilateral medial rectus recession alone (ie, without the bilateral T-R) would adequately change the proprioception-controlled muscle tension and provide all the therapeutic improvements possible, the T-R portion was retained to ensure maximal improvements.
Subject 4 was a 55-year-old woman who was originally seen when she was 49. She had oculocutaneous albinism and bilateral foveal hypoplasia in addition to her INS. Her waveforms were J, Jef, PC, PJ, and occasional P. There was no damping with convergence, and her neutral region (where the direction of the INS reverses) was at 5° left gaze. Clinically, she also was thought to have an intermittent right eye exotropia of 15 D. Because of the small amount of rotation needed, either a 2-muscle Anderson plus 2-muscle T-R or a 4-muscle T-R could be performed in addition to any strabismus correction.
All patients were given the augmented tendon sutures in addition to their INS surgeries. The sutures were made following the methodology outlined in 2009 as the “simple ATS method.”(2) The line of the extra suturing was placed 3–4 mm posterior and parallel to the usual suture line securing the muscle for the disinsertion-reattachment, recession, or resection. As a technical side note, the suture (double armed 6-0 polyglactin 910) was weaved partial thickness through the muscle with locking bites in both borders of the muscle. The suture was passed through the entire width of the muscle, and special care was given to make sure every part of the muscle was in contact with the suture along the line of suturing. Then the excess suture ends were cut close to the muscle border. This extra line of suture was not used to secure the muscle to the globe. Subjects 1 and 2 received 4-muscle Kestenbaum procedures, subject 3 received bilateral medial rectus recessions plus bilateral lateral rectus AT-R, and S4 received an Anderson with strabismus correction for an exotropia plus AT-R of one medial rectus muscle.
Thus, all patients received 4-muscle T-R with augmented tendon sutures, either included in their INS surgeries (Kestenbaum) or in addition to them (bilateral medial rectus recession or Anderson plus strabismus). Table 2 contains the surgical data. Unfortunately, subject 4 was lost to follow-up and no postoperative eye movement data were taken. | | | Results | INS Data and NAFX Analyses
As Figures 1-3 demonstrate, the augmented sutures did not interfere with the major effects of each surgery (ie, shifting the NAFX peak to primary position or increasing it with induced convergence); the therapeutic effects of the Kestenbaum and bilateral medial rectus recession procedures were achieved with AT-R. There was a large, variable preoperative nystagmus when subject 1 attempted to fixate targets to the right and a difficulty (including disrupted fusion) in doing so (Figure 1). Fixation of targets to the left was accomplished with lower amplitude nystagmus but with frequent reversals of the fixating eye that affected the variability of the NAFX values. The post-Kestenbaum plots demonstrate both the shifting of the damped-nystagmus region to primary position and damped, binocular fixation across the range of gaze angles tested.
The preoperative data from subject 2 show both the damping in right gaze and the variable esotropia (Figure 2). After the Kestenbaum procedure with AT-R, subject 2 had damped nystagmus across most of right gaze and well into left gaze. Also, there was only esotropia in far lateral gaze that diminished postoperatively. Unlike subject 1, subject2 had little trouble fixating targets at all gaze angles.
The preoperative damping of subject 3’s INS is evident whether convergence was accomplished by fixating at ever-nearer targets (Figure 3, top) or between far and near targets (bottom). After bilateral medial rectus recession with AT-R, subject 3 was already using convergence (to overcome the surgically induced divergence) for the far target and required additional convergence for the nearer targets. Depending on the amount of additional convergence required, further damping is possible or fusion could be lost and an increase in INS may occur.
Figure 4 shows the preoperative neutral zone of subject 4 at a left gaze of ?5°; closer examination of the INS waveforms revealed them to be jerk right at gaze angles to the right of that region and jerk left at more leftward gaze angles. Both sets of preoperative data (at ages 49 and 55) show the consistent characteristics of the INS and strabismus. She preferred to fixate with the left eye in right gaze and the right eye in left gaze (ie, adducting eye fixation) but occasionally switched her fixating eye. These preoperative data also demonstrated a fairly consistent esotropia; there was only one instance of the reported transient right eye exotropia.
To determine if the augmented sutures provided greater improvements in NAFX values than the single sutures used to attach the muscles, the pre- and postoperative NAFX and LFD values of subjects 1, 2, and 3 were examined and compared to those from estimation curves derived from single-suture T-R procedures. (9,10)
Subject 1 had pre-Kestenbaum values of NAFXpk = 0.565 at 15° left gaze and LFD = 15°. Figure 5 shows pre- and post-Kestenbaum plots of NAFX versus gaze angle and the pre-Kestenbaum estimated plot. Equivalent, age-corrected visual acuity values(8) are also shown in this and the following three figures. As expected, NAFXpk was shifted rightward 15° from 15° left gaze to 0°. After the Kestenbaum procedure with AT-R, subject 1 exhibited a 6% decrease in NAFXpk to 0.530 and a 127% broadening of the LFD to 34°. Based on our single-suture T-R curves, the preoperative estimated improvements in NAFXpk were 0.667 (18%) and 36.5° (143%) in LFD. These and the values for all subjects are summarized in Table 3, the final column of which contains the percent error between the preoperative estimated values of NAFXpk and LFD and those measured postoperatively. For subject 1, these values were ?24% and ?16%, respectively.
Subject 2 had pre-Kestenbaum values of NAFXpk = 0.770 at 25° right gaze and LFD = 18°. Figure 6 shows pre- and post-Kestenbaum with AT-R plots of NAFX versus gaze angle and the pre-Kestenbaum estimated plot. As expected, NAFXpk was shifted leftward 15° from 25° right gaze to 10°. Post-Kestenbaum with AT-R, S2 exhibited a 9% decrease in NAFXpk to 0.700 and a 122+% broadening of the LFD to 40+°. Based on our single-suture T-R curves, the preoperative estimated improvements in NAFXpk were 0.793 (3%) and 39° (115%) in LFD. The respective percent errors in estimation were ?12% and 7+%, respectively.
Subject 3 had pre–bilateral medial rectus muscle recession plus bilateral rectus AT-R values of NAFXpk = 0.340 at 10° right gaze and LFD = 33°. Figure 7 shows pre- and postoperative plots of NAFX versus convergence (Figure 7A) and gaze angle (Figure 7B), and the preoperative estimated plot based on our prior study of the effects of induced convergence on INS.(13) As the estimated curve in Figure 7A shows, applying the approximate 14 PD convergence to far targets results in an increased NAFX (here, to 0.530) and an upward, clockwise rotation of the NAFX curve about the 60 PD point. However, the postoperative downward shift in NAFX values (especially at far) prevented the increase in distance NAFX usually found despite the retained vergence damping of the INS waveforms. Postoperatively, subject 3 exhibited an unchanged NAFXpk of 0.340 and a 12+% broadening of the LFD to 37+°. The preoperative estimated improvements with T-R in NAFXpk were 0.530 (56%) and 50° (52%) in LFD. The respective percent errors in estimation were ?56% and ?40%, respectively.
Subject 4 underwent pre-Anderson recession plus medial rectus AT-R plus strabismus recessions, with values of NAFXpk = 0.590 and LFD = 30°. Based on our single-suture T-R curves, the preoperative estimated improvements in NAFXpk and LFD were 0.684 (16%) and 48° (18%), respectively. Unfortunately, we were unable to record her postoperative eye movements to document the apparent nystagmus improvements indicated by her postoperative comments (see below). Figure 8 shows both the pre-operative NAFX and estimated postoperative NAFX versus gaze angle curves.
The achieved NAFXpk and LFD values fell close to those estimated based on single-suture data but were not uniformly greater (and in some cases, decreased) as a result of the additional sutures. The individual data points from which the curves were derived were from 22 patients with INS, with and without associated afferent visual deficits or strabismus and of all ages, and from some with acquired nystagmus.(9,10,14,19,20) The average percent errors between the values achieved using augmented sutures and those estimated from single sutures(11) were ?31% for NAFXpk and ?16% for LFD (see Table 3). Also shown in Table 3 are the changes in subject 3 compared to that produced by vergence data from patients whose INS damped with convergence.
Patient Impressions
Despite the obvious bias for a patient to view surgery as successful, the authors felt that the patient’s own descriptors were integral to understanding the postsurgical experience and were correlated to the types of visual function improvements predicted by the data.
Subject 1’s mother reported a “very definite change in vision,” “definitely improved,” “now looks straight on,” and “can recognize faces faster” after surgery with improved behavior showing “increase in confidence.” Subject 1 said he “sees bigger and clearer” and “can now see out of the corner of his eyes.” His mother definitely noted less movement on his best days currently.
Subject 2 reported improvements in color vision and diplopia and “everything seems so much bigger” and “huge difference—nice difference.” He noted “great vision” within the first 4 postoperative days. After the postsurgical improvement in subject 2’s visual acuity, the use of contact lenses provided further improvement (from 0.4+2 to 0.5, as shown in Table 1). Unfortunately, eye movement data with contact lenses that might allow differentiation of their effect from a possible, albeit improbable, late effect of the surgery is unavailable.
Subject 3, having struggled throughout college due to the visual function limitations caused by his INS, hoped to improve his vision enough to facilitate successful completion of his upcoming entrance into law school. The trial prisms during his first semester and the surgery for the remaining semesters helped him to do so.
Subject 4 initially stated that the changes were “slight,” and she “would not do it again.” However, others noticed and commented on a reduction in her nystagmus, and she “now had better vision at distance,” saw things “a little brighter” and “faster” as was “now able to recognize faces in a crowd faster.” Despite her better distance vision and new ability to scan a crowd and recognize faces (all, well-documented therapeutic benefits of the T-R procedure), she did not feel her field of clear vision was wider. She was unavailable for postoperative to verification of NAFX and LFD improvements (see estimated improvements in Table 3) that would have produced her reported improvements or to investigate her problems with close vision that she attributed to her surgery. However, given her reported improvements in visual function, it is likely that this was due to her strabismus rather than the INS portion of the combined surgery. | |
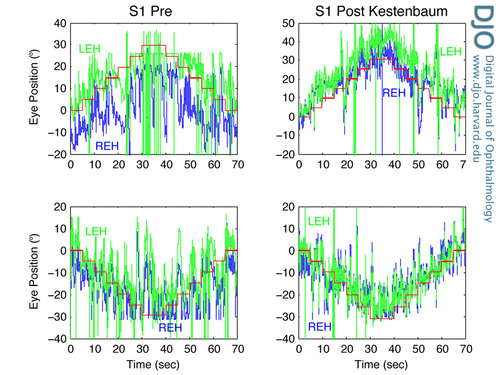
Figure 1
The pre- and post-Kestenbaum horizontal eye movements of S1 demonstrating the overall damping of the INS as well as the improvement in maintaining binocular fixation at targets stepping across the ±30° range. The post-Kestenbaum plots also show the shifted and broadened range of damped INS across the central ±15°-20°. In Figures 1-4, target positions appear in red, REH-right eye horizontal, and LEH-left eye horizontal. Large spikes indicate either dropped data points or blinks and flat lines at extreme gaze, saturation. To reduce clutter and maximize the data presentations, the nystagmus amplitude and time axes are shown to the left of the left-column and below the bottom-row plots respectively. Similarly, titles are shown above their respective columns.
|
|

Figure 2
The pre- and post-Kestenbaum eye movements of subject 2 demonstrating the overall damping of the INS as well as the improvement in maintaining binocular fixation at targets stepping across the ±30° range. The post-Kestenbaum plots also show the shifted (from right gaze) and broadened range of damped INS across the central ±15°-20°.
|
|
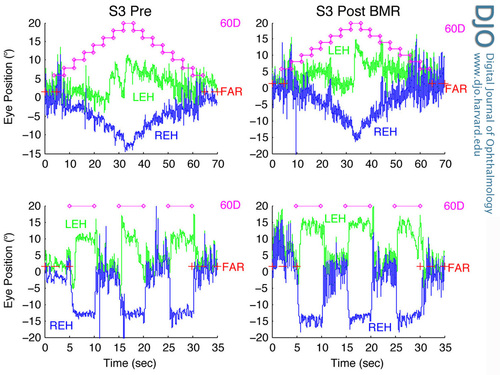
Figure 3
The eye movements of subject 3 before and after bilateral medial recession showing INS damping with convergence to stepped targets (top) or from far to near targets (bottom); 60 PD required for convergence with nearest target.
|
|

Figure 4
The preoperative eye movements of subject 4 at ages 49 and 55 demonstrating the stability of INS characteristics over this 6-year period. The neutral zone of this INS was at 5° left gaze. Both records also document the stability of a 10° esotropia over the same time period.
|
|
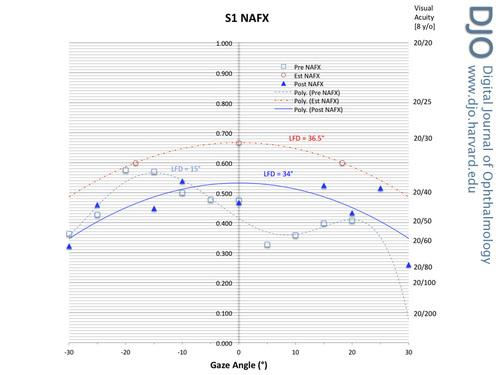
Figure 5
Pre- and post-Kestenbaum with additional sutures plots of NAFX versus gaze angle for subject 1 showing both the shifted peak NAFX value and the broadened LFD. The dash-dot estimated plot, based on single-suture procedures, is shown for comparison. In Figures 5-8, the LFD values of each curve and the equivalent, age-corrected, potential visual acuities are shown.
|
|
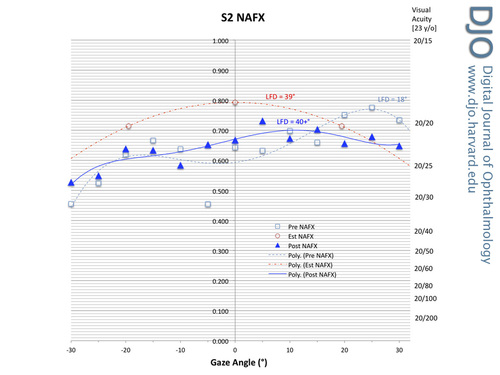
Figure 6
Pre- and post-Kestenbaum with additional sutures plots of NAFX versus gaze angle for subject 2 showing both the shifted peak NAFX value and the broadened LFD. The dash-dot estimated plot, based on single-suture procedures, is shown for comparison.
|
|

Figure 7
Before and after bilateral medial recession with additional sutures plus bilateral AT-R plots of NAFX versus (A) convergence angle and (B) gaze angle for subject 3. Figure 7A shows the NAFX decrease at far and its effects on convergence damping; Figure 7B shows the slightly shifted peak NAFX value and the slightly broadened LFD. The dash-dot estimated plots, based on the effects of vergence on INS, are shown for comparison.
|
|

Figure 8
Before T-R and estimated after T-R with additional sutures plots of NAFX versus gaze angle for subject 4 showing the estimated improved peak NAFX value and the estimated broadened LFD. The dash-dot estimated plot, based on single-suture T-R procedures, is shown for comparison.
|
|
| Discussion | Clinical and eye movement data are objective and do provide specific, albeit limited, indications of the quality of the visual experience; however, it is often the real-world reports of patients that provide the most important insights into improvements in visual function. The impressions noted above are consistent with our data and illustrate how much improvement in one’s life is possible despite what may seem like limited improvements in measured clinical and eye movement data. Obtaining 20/20 vision may not be possible in patients with either severe afferent deficits, INS, or both; however, that should not deter the physician from maximizing visual function for each patient without compromising other important ocular motor functions (ie, making accurate saccadic and smooth pursuit movements and vestibulo-ocular and optokinetic reflexes as well as maintaining ocular alignment to prevent diplopia). Any small incremental improvement in visual function could be the one that allows for significantly enhanced quality of life.
The postoperative visual acuity increase in subject 2 with the addition of contact lenses is both interesting and potentially significant. It is consistent with the postoperative damping and increased NAFX documented with the use of memantine in acquired nystagmus.(15) Both result from additional nystagmus damping via pathways independent from EOM proprioception. Memantine works centrally on the nystagmus signal and contact lenses act on that signal using exteroceptive (relating to stimuli that are external to an organism) information from the ophthalmic division of the trigeminal nerve.(16) Thus it appears that INS therapies using different pathways may also have beneficial multiplicative effects similar to that of memantine in acquired nystagmus. The “take-home” message is that the physician should always investigate additional postsurgical therapies in INS patients in an effort to further improve visual function.
The comments of subject 4 illustrate the importance of clearly explaining the expectations for improvements (which, based on her specific comments about improved visual function, appear to have been achieved) and avoiding unrealistic expectations on the part of the patient. They also illustrate how concurrent strabismus can complicate and overshadow the INS improvements that are achieved.
Although the two earlier hypotheses regarding augmented sutures put forth in 2009 were related,(2) they are not necessarily interdependent. It was hypothesized that additional sutures might increase the beneficial therapeutic effects of the T-R procedure (hypothesis 1, namely, the AT-R procedure) and that would support the second hypothesis, concerning the ATS procedure (sans tenotomy). However, even if the initial suture proved sufficient to provide the therapeutic improvements with no increase from additional sutures, the second hypothesis remains valid and subject to testing. If, as we have speculated, the key factor in changing the proprioceptive tension–control feedback loop and damping nystagmus is due to the effects of the distortion of the proprioceptive sensors produced by the suture and the resulting scarring and not the tenotomy per se, the latter may not be necessary.(17,18) Why additional sutures interfered with NAFXpk improvements but not LFD improvements is currently unknown.
Based on the findings of this paper (albeit, in a small number of patients), we conclude that the single suture in each tendon (inherent in the 4-muscle T-R procedure) is sufficient to produce the positive therapeutic effects documented elsewhere and that an additional suture does not appreciably increase those effects. Because increases in NAFXpk were found in single-suture studies of many patients (INS and acquired nystagmus), the additional sutures could have a slightly detrimental effect on NAFXpk, but such a conclusion would require further study. All patients did achieve results close to those estimated by their LFD values before AT-R and were within the patient variation data that were used to produce the estimation curves.(9,10,11,14,19,20) However, in the absence of demonstrable improvements of extra sutures over the single-suture T-R procedure, their use was discontinued.
How do our findings impact the second, ATS, hypothesis? Since additional sutures appear unnecessary, the hypothesis may be modified by deleting the word, “augmented” and simply describing it as “the tendon suture (TS, sans tenotomy) procedure.” That is, place a single suture in the distal tendons of the 4 horizontal rectus muscles without performing the T-R surgery.
It has been shown that fusion maldevelopment nystagmus syndrome (FMNS) is also damped by the T-R procedure.(7,15,19,20) Therefore, the efficacy of the hypothesized TS procedure in treating INS can be tested in FMNS patients as an adjunct to their strabismus surgery. That is, perform the recessions and/or resections necessary to correct the strabismus and then place a single suture in the distal tendons of the remaining (unoperated) horizontal muscles. Comparisons of the changes in NAFX values found using the 4-muscle TS procedure in FMNS with the curve of estimated NAFX improvement versus NAFX before T-R will determine whether the TS procedure is as effective as the 4-muscle T-R. As explained elsewhere,(20) the NAFX values should be those measured during abduction of the fixating eye, because they will be the lowest and most expected to improve; that corresponds to the off-peak NAFX values in INS, which also improve more than the peak NAFX. Also, the slopes of the NAFX versus gaze angle lines should decrease after TS; that corresponds to broadening the LFD in INS. Comparing pre- and post-TS visual acuities for each eye in both abduction and adduction should provide clinical measures of these effects.
Another and more direct method of testing the TS sans tenotomy procedure is on INS patients with small, lateral nulls requiring Anderson recessions of 2 muscles. Instead of the recommended T-R of the 2 unoperated muscles, a TS sans tenotomy can be substituted. Again, comparisons to the estimated improvements from a T-R will determine the efficacy of the TS sans tenotomy procedure.
In conclusion, placing additional sutures in the distal tendons did not achieve the improvements in both NAFXpk and LFD that have been documented using single-suture techniques; moreover, in some patients it decreased NAFXpk. Therefore, it is not recommended. The reason that LFD values were increased but not NAFXpk values is unknown and would require further study; however, that is an unlikely endeavor, given the poor results obtained by additional sutures. | | | References | 1. CEMAS_Working_Group. A National Eye Institute Sponsored Workshop and Publication on the Classification of Eye Movement Abnormalities and Strabismus (CEMAS). In The National Eye Institute Publications. 2001. www.nei.nih.gov/news/statements/cemas.pdf.
2. Dell’Osso LF, Tomsak RL, Thurtell MJ. Two hypothetical nystagmus procedures: augmented tenotomy and reattachment and augmented tendon suture (sans tenotomy). J Pediatr Ophthalmol Strabismus 2009;46:337-344.
3. Dell’Osso LF, Jacobs JB. An expanded nystagmus acuity function: intra- and intersubject prediction of best-corrected visual acuity. Doc Ophthalmol 2002;104:249-276.
4. Dell’Osso LF. Using the NAFX for eye-movement fixation data analysis and display. OMLAB Report 2005;111005:1-7.
5. Jacobs JB, Dell’Osso LF. Extending the expanded nystagmus acuity function for vertical and multiplanar data. Vision Res 2010;50:271-278.
6. Wang ZI, Dell’Osso LF. A review of the tenotomy nystagmus surgery: origin, mechanism, and general efficacy. Neuro-Ophthalmol 2007;31:157-65.
7. Dell’Osso LF. New treatments for infantile and other forms of nystagmus. In: Leigh RJ, Devereaux MW, eds. Advances in Understanding Mechanisms and Treatment of Congenital Forms of Nystagmus. New York: Oxford University Press, 2008:87-98.
8. Wang ZI, Dell’Osso LF. Eye-movement-based assessment of visual function in patients with infantile nystagmus syndrome. Optom Vis Sci 2009;86:988-95.
9. Dell’Osso LF. Predicting Treatment Outcomes in Infantile Nystagmus: NAFX analysis of ocular motor data. Chapter 21. In: C. Harris IG, Sanders J, eds. The Challenge of Nystagmus: Proceedings of the Nystagmus Network Research Workshop, Abingdon, UK, 2-5 September 2009. London: Nystagmus Network, 2012:325-38.
10. Hertle RW, Dell’Osso LF. Nystagmus in Infancy and Childhood. Current Concepts in Mechanisms, Diagnoses, and Management. Oxford: Oxford University Press, 2013:324.
11. Hertle RW, Dell’Osso LF. Chapter 7. Treatment. In: Nystagmus in Infancy and Childhood. Current Concepts in Mechanisms Diagnoses, and Management. Oxford: Oxford University Press, 2013:237-43.
12. Wang ZI, Dell’Osso LF. Being “slow to see” is a dynamic visual function consequence of infantile nystagmus syndrome: model predictions and patient data identify stimulus timing as its cause. Vision Res 2007;47:1550-60.
13. Serra A, Dell’Osso LF, Jacobs JB, Burnstine RA. Combined gaze-angle and vergence variation in infantile nystagmus: two therapies that improve the high-visual acuity field and methods to measure it. Invest Ophthalmol Vis Sci 2006;47:2451-60.
14. Wang Z, Dell’Osso LF, Jacobs JB, Burnstine RA, Tomsak RL. Effects of tenotomy on patients with infantile nystagmus syndrome: foveation improvement over a broadened visual field. J AAPOS 2006;10:552-60.
15. Tomsak RL, Dell’Osso LF, Rucker JC, Leigh RJ, Bienfang DC, Jacobs JB. Treatment of acquired pendular nystagmus from multiple sclerosis with eye muscle surgery followed by oral memantine. DJO 2005;11:1-11.
16. Taibbi G, Wang ZI, Dell’Osso LF. Infantile nystagmus syndrome: broadening the high-foveation-quality field with contact lenses. Clin Ophthalmol 2008;2:585-90.
17. Wang Z, Dell’Osso LF, Zhang Z, Leigh RJ, Jacobs JB. Tenotomy does not affect saccadic velocities: Support for the “small-signal” gain hypothesis. Vision Res 2006;46:2259-67.
18. Dell’Osso LF, Wang Z, Leigh RJ, Jacobs JB. Hypothetical explanation for the role of proprioception in the damping of infantile nystagmus by tenotomy surgery: the small-signal gain hypothesis. In: Callaos N, ed. Proceedngs of the WMSCI 2006 Conference. Orlando, FL; 2006:39-44.
19. Wang ZI, Dell’Osso LF, Tomsak RL, Jacobs JB. Combining recessions (nystagmus and strabismus) with tenotomy improved visual function and decreased oscillopsia and diplopia in acquired downbeat nystagmus and in horizontal infantile nystagmus syndrome. J AAPOS 2007;11:135-41.
20. Dell’Osso LF, Orge FH, Jacobs JB, Wang ZI. Fusion maldevelopment (latent/manifest latent) nystagmus syndrome: effects of four-muscle tenotomy and reattachment. J Pediatr Ophthalmol Strabismus 2014;180-8.
| |
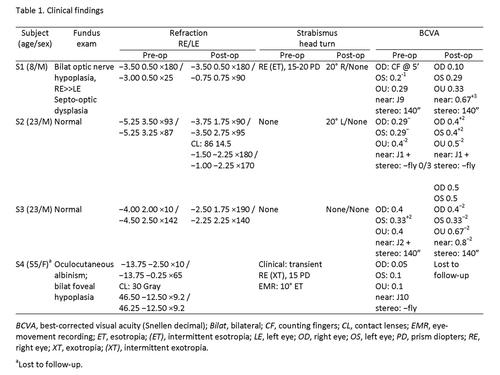
Table 1
Clinical findings
|
|
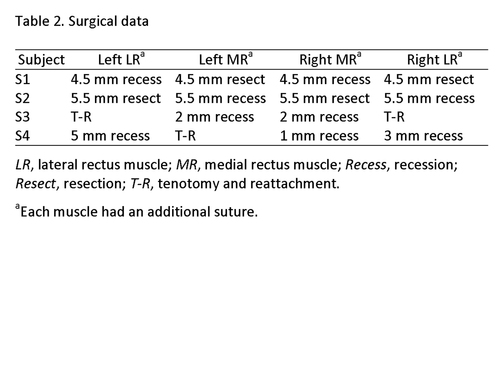
Table 2
Surgical data
|
|
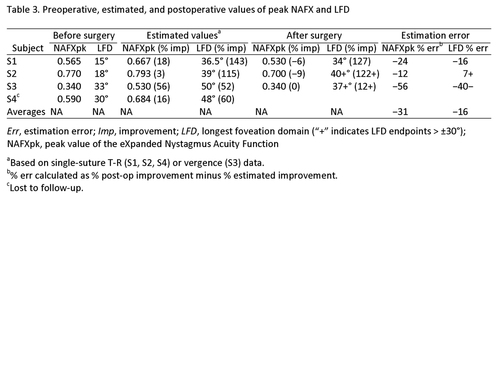
Table 3
Preoperative, estimated, and postoperative values of peak NAFX and LFD
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in