|
|
 |
 |
 |
 |
|
|
Adding access to a video magnifier to standard vision rehabilitation: initial results on reading performance and well-being from a prospective, randomized study
Digital Journal of Ophthalmology 2017
Volume 23, Number 1
March 31, 2017
DOI: 10.5693/djo.01.2017.02.001
|
Printer Friendly
Download PDF |


 Mary Lou Jackson, MD
Mary Lou Jackson, MD | Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, Massachusetts Kimberly A. Schoessow, OTD, OTR/L | Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, Massachusetts Alexandra Selivanova, BS | Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, Massachusetts Jennifer Wallis, PhD | Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, Massachusetts
|
|
|
| Abstract | Purpose
Both optical and electronic magnification are available to patients with low vision. Electronic video magnifiers are more expensive than optical magnifiers, but they offer additional benefits, including variable magnification and contrast. This study aimed to evaluate the effect of access to a video magnifier (VM) added to standard comprehensive vision rehabilitation (VR).
Methods
In this prospective study, 37 subjects with central field loss were randomized to receive standard VR (VR group, 18 subjects) or standard VR plus VM (VM group, 19 subjects). Subjects read the International Reading Speed Texts (IReST), a bank check, and a phone number at enrollment, at 1 month, and after occupational therapy (OT) as indicated to address patient goals. The Impact of Vision Impairment (IVI) questionnaire, a version of the Activity Inventory (AI), and the Depression Anxiety and Stress Scale (DASS) were administered at enrollment, 1 month, after OT, 1 month later, and 1 year after enrollment. Assessments at enrollment and 1 month later were evaluated.
Results
At 1 month, the VM group displayed significant improvement in reading continuous print as measured by the IReST (P = 0.01) but did not differ on IVI, AI, or DASS. From enrollment to 1 month all subjects improved in their ability to spot read (phone number and check; P < 0.01 for both). The VM group improved in their ability to find and read a number in a phone book more than the VR group at 1 month after initial consultation (P = 0.02). All reported better well-being (P = 0.02).
Conclusions
All subjects reported better well-being on the IVI. The VM group read faster and was better at two spot reading tasks but did not differ from the VR group in other outcome measures. | | | Introduction | It is estimated that reading is difficult for over 85% of patients who attend vision rehabilitation consultations.(1) Reading is a priority skill for most individuals and is considered to be an important part of maintaining independence.(2) Magnification plays a major role in addressing the goal of reading for patients with central field loss, such as those with age-related macular degeneration (AMD), which has been estimated to affect over 1.75 million individuals in the United States.(3) Emerging research shows benefits of multidisciplinary rehabilitation; however, it is not known what portion of rehabilitation success can be attributed to the various rehabilitation components: training, device acquisition, environmental modifications, education, visual skills, reading practice, patient motivation, and caring rehabilitation personnel.(4) Most previous research has reported pre- and post-rehabilitation function but has not quantified the benefit attributable simply to device acquisition. Addressing the question of optimal rehabilitation, including optimal reading device, is a priority in this research.
Video camera magnifiers are a simple combination of a video camera and a monitor; they allow magnification, enhanced image contrast, and a wide field for viewing text. They are more expensive than traditional optical devices but are often chosen by a patient in comprehensive vision rehabilitation. A 2013 Cochrane Review examined all available randomized and quasi-randomized studies relevant to magnifying reading aids for adults with low vision (10 studies were included) and concluded that the evidence was insufficient to assess the effect of low-vision devices on reading performance, although there was some evidence that electronic devices were associated with more improvement in reading speed than optical devices were.(5)
The present study compared patients who received standard visual rehabilitation (VR) with those who, in addition to VR, were provided with a video magnifier (VM) at their initial contact with a multidisciplinary vision rehabilitation service. VR included an initial consultation during which patients were educated about rehabilitation strategies, given information about remaining visual function, and shown a range of optical and electronic devices, which they could purchase. Our hypothesis was that access to an electronic video magnifier device would improve objective reading performance and patient-reported outcomes. This study evaluated results at enrollment, when all subjects used prerehabilitation devices, and at 1 month after enrollment, when subjects who had had access to a video magnifier completed reading assessment using the video magnifier. Those in the group without access to the VM used any device they may have acquired prerehabilitation or during the month since their initial consultation. | | | Materials and Methods | Study Design
This study was approved by the Massachusetts Eye and Ear Institutional Review Board. Written informed consent was obtained from all participants. This pilot study was a prospective, double-armed, randomized, controlled trial (Figure 1) comparing objective measurements of reading and patient-reported quality of life, including perceived reading ability, in subjects who had VM access in addition to standard VR (VM group) to subjects who only had VR (VR group). Randomization occurred after the initial consultation. All participants underwent an initial vision rehabilitation consultation, including visual function evaluation and discussion of rehabilitation principles and options. Patients in the VM group received a desk video magnifier when they presented for initial consultation. They were free to use this device as much or as little as they wished during the ensuing month. Patients in the VR group were free to purchase devices at any time, and they were advised that they would also receive a free video magnifier after the completion of rehabilitation training with an occupational therapist (Figure 1). All subjects returned after 1 month to begin an occupational therapy (OT) evaluation and subsequent training. The OT training consisted of evaluation of visual performance, assessment of goals and training with devices and task modification, as required. Subjects had objective reading assessments at three time points: enrollment, 1 month after enrollment, and at the conclusion of OT. Subjects completed questionnaires at five time points: enrollment, 1 month after enrollment, at the conclusion of OT, 1 month after OT discharge, and 1 year after enrollment. This study presents findings from the first two time points of the study: from enrollment to 1 month after enrollment.
Patient Selection
Patients attending a multidisciplinary outpatient vision rehabilitation clinic at the Massachusetts Eye and Ear from February 2010 to May 2011 were invited to participate in this study. Inclusion criteria included age ≥40 years, central visual field loss (defined as not responding to 1 or more targets on macular perimetry testing in the better-seeing eye), no disease affecting the peripheral retina, visual acuity worse than 20/40 in each eye and better than 20/400 in the better seeing eye, cumulative score of >20 (of 30) on the 6-question modified Mini Mental State Examination (MMSE) questionnaire for visually impaired, sufficient hearing to participate in interviews, and no previous experience with vision rehabilitation or video camera magnifiers.
Clinical Visual Function Tests
As part of the initial consultation all subjects had refraction and measurement of visual acuity using the Early Treatment Diabetic Retinopathy Study (ETDRS) chart or Snellen a projected chart. Contrast sensitivity was measured with the Pelli-Robson chart. All subjects underwent scanning laser ophthalmoscope macular perimetry to document fixation and the presence of central scotoma(s) using the commercially available OPTOS macular perimeter and a size III target testing the central 20° of visual field. The extent of the scotoma was estimated by viewing results from both monocular perimetry tests and determining the scotoma that would overlap, viewing binocularly. The size and location of the scotoma was then classified in five categories: (1) near normal, with scotoma only detected with a target smaller than Goldmann III size; (2) small scotoma, ≤1 disc diameter (DD); (3) moderate scotoma, >1 and ≤2 DD; (4) severe scotoma, >2 and ≤3 DD; and (5) very severe scotoma, >3 DD.
Visual Performance Measures
Reading speed was assessed in words per minute (wpm) using the International Reading Speed Texts (IReST), in which subjects read to the best of their ability a standardized paragraph of newspaper-sized text aloud.(6) Subjects also had objective assessment of ability to read the amount on a bank check and a phone number on a page from the phone book. The participants also were asked to identify the handwritten amount on the check. The same reading items were used at enrollment and after 1 month; there was no variation in print size and contrast. At enrollment, subjects could hold the material at any distance and use any devices they habitually used before rehabilitation. The reading tasks were videotaped and afterward scored by two investigators as correct (score = 3), correct but struggles (= 2), partly correct (= 1), or impossible to complete (= 0). For the 1-month assessment, those in the VR group could again use any device they wished and those in the VM group used the video magnifier.
Patient-reported Measures
The Impact of Vision Impairment questionnaire (IVI) and 10 reading questions from the Activity Inventory (AI) were used as patient-reported measures.(7,8) The IVI is a validated 28-item questionnaire designed to identify vision-specific limitations in activities that affect patients’ quality of life. The 28 questions fall into three domains: mobility and independence (mobility), emotional well-being (well-being), and reading and accessing information (reading). The AI first requires the participant to rate the importance of a goal (eg, read newspaper), and then rate the difficulty of the tasks nested under that goal (eg, read headlines) as “not difficult” (= 0), “slightly difficult” (= 1), “moderately difficult” (= 2), “very difficult” (= 3), “impossible to do without someone else’s help” (= 4) or “not applicable” (= 5).(9) If a goal was not rated as important to the individual, then it was not included in the final scoring. The Depression, Anxiety and Stress Scale (DASS) was administered to assess subjective well-being.(10) The individual administering the questionnaires was not masked to group assignment.
Procedure
All patients had a consultation with an ophthalmologist (MLJ) who discussed the remaining visual function, the impact of the visual deficit on visual performance, including reading, the advantages and drawbacks of the various device categories, options to acquire devices, and the recommendation of subsequent occupational therapy evaluation to address training to use devices, evaluation of success with devices, and opportunities to modify tasks and strategies to improve visual performance. Randomization to receive a VM at enrollment or at the end of vision rehabilitation was according to a computer-generated numerical series. After half of the patients had been enrolled, an adaptive design was adopted to ensure that the two groups were comparable in visual acuity.
At enrollment, all subjects completed the questionnaires and were videotaped completing the reading tasks using their usual prerehabilitation devices or glasses. Patients randomized to the video magnifier group were shown basic operation and set-up of the desk model video magnifier (Optelec, ClearView+, 2.6× to 50× magnification, 17" display). All subjects were able to purchase handheld magnifiers or reading glasses at any time during the rehabilitation process (standard VR). Subjects were aware that their reading performance would be tested 1 month later.
All subjects returned 1 month after their initial consultation and study enrollment. During the 1-month interval the subjects who had had access to the VM had been using it as much as they wished, for whatever purpose they chose. Objective and subjective reading performance measures were repeated. The VM group now used the video magnifier for reading assessments. The VR group used their usual devices for reading tasks, which may have differed from the aids used at enrollment.
Statistical Analysis
Standard descriptive statistics were reported, mean (standard deviation) for continuous variables and frequency count (%) for categorical variables. A two-sample t test, χ2 test, or Fisher exact test were used to compare baseline characteristics between the two groups and between patients who withdrew and those who completed the study from T1 to T2. Repeated measures analysis of variance (ANOVA) was performed to examine the effect of time, effect of VM acquisition and interaction between them on IReST, IVI, AI, and DASS scores. In addition, Wilcoxon signed rank tests were used to examine whether there was significant improvement of check and phone number reading task scores from T1 to T2. Wilcoxon rank-sum tests were used to determine whether there was significant difference in the change in scores for the same tests from T1 to T2 between the VM and VR groups. Statistical analyses were performed using SAS 9.3 (SAS Institute Inc, Cary, NC) and MATLAB 2012a (MathWorks, Natick, MA).
For each question in the IVI questionnaire the answers were rated as “not at all” (= 0), “a little” (= 1), “a fair amount” (= 2), “a lot” (= 3) or “do not do for other reasons” (= 4).(8) Total and domain scores were calculated as arithmetic averages. Although the number of participants who responded “do not do for other reasons” was recorded for each question, these answers were not included in the calculation of the domain scores. Rasch analysis was used to assess the psychometric properties of the IVI and its three subscales using the Andrich rating scale model,(11) with Winsteps 3.75 (Chicago, IL).(12)
Rasch analysis is a form of item response theory where ordinal raw questionnaire scores are transformed to estimates of interval measures (expressed in log of the odds units, or logits) that demonstrate the essential features of measurement, thus allowing subsequent parametric analyses to be performed.(13) A high person measure (in logits) indicates that a person possesses a high level of the assessed latent trait (eg, vision-related quality of life) and vice versa.(14). Rasch analysis also provides significant insight into the psychometric properties of the scale.(14)
The AI was scored using an Excel spreadsheet (provided by the author of the AI, Robert W. Massof). For correct Rasch scoring of all subscales the full AI questionnaire is required, and in this study only a shortened version of the AI questionnaire was administered. As a result, overall “goals” were Rasch scored for further analysis.
The sum of all DASS-21 scores for each participant was multiplied by 2, according to recommended analysis methods, and this was used for analyses.
Two independent reviewers scored the videotaped patients performance on reading the amount on a bank check and on reading a phone number. | |
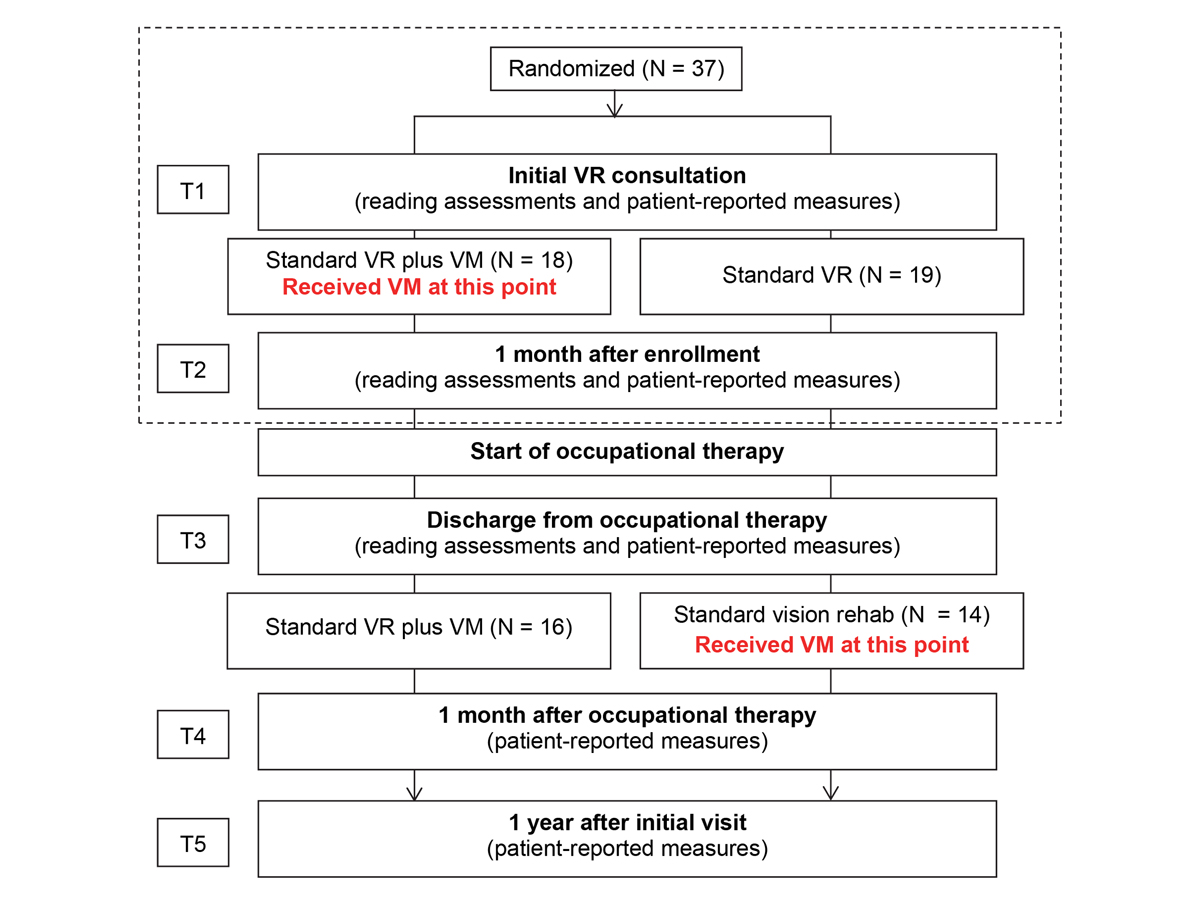
Figure 1
Study flowchart. Results presented in this study are from enrollment to 1 month after enrollment (dashed box).
|
|
| Results | A total of 37 patients (18 females; mean age, 72.9 [range, 40-91]) were enrolled, 18 in the VM group and 19 in the VR group (Figure 1). Demographic characteristics and visual function of these patients are provided in Table 1. The groups were not significantly different in age, sex, visual acuity, contrast sensitivity, or MMSE, and the groups were roughly balanced in the type of central field loss (P = 0.11; see Table 2). One month after enrollment, 6 subjects withdrew from the study (3 from each group), and those who withdrew from the study did not significantly differ from those who continued in age, sex, visual acuity, contrast sensitivity, and MMSE (Table 3). The most common diagnosis was AMD or juvenile-onset macular degeneration (73%). The remaining subjects had optic nerve disease (16%) and macular dystrophy or other maculopathy (11%).
At enrollment, the reading speed was 0-125 wpm in the VM group and 0-96 wpm in the VR group (Table 4). This increased to 22-168 wpm in the VM group at 1 month. In the VR group the range was 0-108 wpm at 1 month. Subjects in the VM group read the IReST continuous print significantly faster at 1 month (interaction between time and group, P = 0.01; Figure 2).
Phone Number and Check Reading Tasks
After two raters had scored the videotaped reading performance of subjects, an inter-rater reliability analysis using the kappa statistic was performed to determine rater consistency. The inter-rater reliability was substantial for both measures at enrollment and 1 month later. The kappa coefficient was 0.80 for the check reading task and 0.72 for the phone number reading task at enrollment and was 0.63 and 0.85, respectively, at 1 month (P < 0.001). An average score for each patient’s performance based on the scores from the two reviewers was used for further analyses. At enrollment, the two groups did not differ in their ability to find and read a phone number in a phone book and the amount on a handwritten check (P = 0.36 and P = 0.67, resp.; Table 5). From enrollment to 1 month, all subjects improved in their ability to find and read a phone number (P < 0.01 for both), but the VM group improved their ability to find and read a number more than the control group at 1 month (P = 0.02; Figure 3). When all subjects were considered, there was also improvement in ability to read the amount on a check (P < 0.001), but neither group improved significantly better than the other at 1 month (P = 0.17).
Patient-reported Measures
Overall, the composite IVI scale displayed suboptimal fit to Rasch model parameters. Although scale precision and targeting of person ability to item difficulty were excellent, there was evidence of multidimensionality in the scale. Specifically, the unexplained variance in the first contrast was >2.0 eigen values and three items exhibited misfit (infit MnSq >1.30). Inspection of the standardized residual loadings for items (>0.4) indicated the possibility of at least two separate dimensions within the scale—“visual functioning” and “emotional.” DIF for gender was also found. DIF indicates that a particular subgroup (eg, sex, age) systemically responds differently to an item despite having the same underlying ability level and therefore indicates the presence of bias. In our sample, males systematically found the question that enquired about feeling lonely or isolated because of eyesight (question 23 on IVI) more difficult than females, even though they shared the same level of ability. Taken together, this evidence suggested that the composite score of the IVI should not be used in further statistical analyses, and the three subscales of the IVI were subsequently analyzed separately. Both the reading and the mobility subscales displayed excellent psychometric properties, with good precision and targeting, and no evidence of multidimensionality or DIF. Each scale had two misfitting questions, but as these only marginally exceeded the acceptable infit MnSq cut-off of 1.30 logits these questions were retained so as not to lose important item content. Initial analysis of the well-being subscale revealed good fit to Rasch model parameters, with ordered thresholds, adequate precision, good targeting and no evidence of multidimensionality. However, questions 23 (“Have you felt lonely or isolated because of your eyesight?”) and 25 (“In the past month, how often have you worried about your eyesight getting worse?”) displayed DIF for sex and visual impairment, respectively. Therefore, questions 23 and 25 were iteratively removed to resolve the DIF, which resulted in excellent psychometric properties of the remaining 6 questions of the well-being subscale.
Repeated measures ANOVA was performed to examine the effect of group, time, and interaction among them on IVI Rasch domain scores (well-being, reading, and mobility) while controlling for age, Geriatric Depression Scale, visual acuity, contrast sensitivity, and central visual field. There was no significant interaction effect for all three IVI Rasch domain scores (P = 0.77, 0.06, and 0.10, resp.). IVI well-being domain score changed significantly over time considering all subjects (main effect of time, P = 0.02; Table 6). The IVI reading and mobility domain scores did not significantly change over time (main effect of time, P = 0.30 and 0.07, resp.; Table 6). The AI person measures for “goals” did not significantly change from enrollment to 1 month later. No significant changes in mood as measured with the DASS were observed. | |
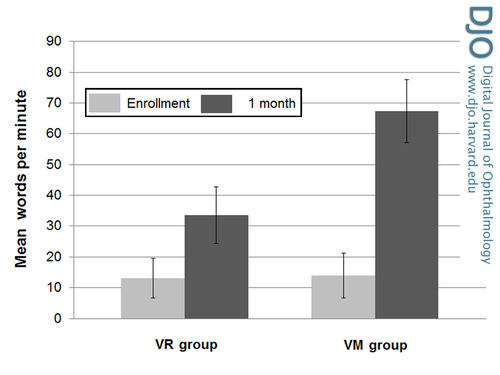
Figure 2
Mean changes in reading speed (IReST) in words per minute. The most significant improvement in reading speed was observed at 1 month in the video magnifier (VM) group, adjusted for age, Geriatric Depression Scale, visual acuity, contrast sensitivity, and central visual field (interaction between time and group, P = 0.01). Error bars represent standard error of the mean (SEM).
|
|
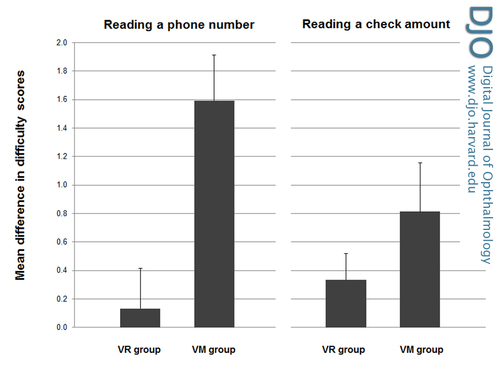
Figure 3
Difficulty scores for reading tasks (change from enrollment to 1 month later). For ease of viewing, individual difficulty scores at enrollment were subtracted from 1 month later to give a difference in individual difficulty scores, and the averages of the difference scores are represented below. The VM group improved more than the control group in reading a phone number at 1 month (P = 0.02). Error bars represent SEM.
|
|
| Discussion | This study assessed the impact of adding access to a VM from the first day that a patient had contact with the vision rehabilitation clinic to standard comprehensive VR. Those in the VM group did read continuous print faster after 1 month and did spot read more accurately; however, patient-reported outcomes were not statistically different in this group compared to those in the VR group.
Reading rehabilitation is part of comprehensive VR. Based on the American Academy of Ophthalmology Preferred Practice Pattern Guidelines, comprehensive VR addresses five areas that may be affected by vision impairment: reading, activities of daily living, safety, participation in activities despite vision loss, and psychosocial well-being.(15) Rehabilitation includes a variety of strategies, psychological supports, education, devices and training. The patient is an active participant in the rehabilitation process. Devices are recommended to the patient, depending on a patient’s visual function and unique goals. Limited previous research has shown that vision rehabilitation improves function and subjective well-being and that reading performance, in particular, improves with vision rehabilitation.(4) Stelmack et al found significant improvement in reading ability in a group of visually impaired veterans who received intensive VR compared to a waitlist control group.(16) The intervention included vision examination, counseling, and provision of low vision devices as well as six weekly training sessions. Reading performance was measured at baseline and 4 months later. Jackson et al observed smaller reading improvement 1 year after comprehensive rehabilitation using the same measure as Stelmack et al.(17) One difference between the two studies is in the provision of free devices. In the Stelmack et al, study devices were provided to subjects at no cost. In the Jackson et al, study rehabilitation did not include free provision of devices for all subjects. Devices were provided by local or state agencies for some patients or could be purchased by patients if they chose. Neither study separated the effect of training on reading from the effect of using devices. Pijnacker et al reviewed methods to train reading performance and found various training methods beneficial (no strong support for one method) but noted that a limitation of all studies was that it was not possible to disentangle the benefit of training from the benefit of devices.(18) A systematic review of eccentric viewing also noted that a failure to separate effects of eccentric viewing training from effects of using low-vision devices was one reason that reviewed studies failed to meet criteria for well-designed trials.(19)
In this study we offered the VM to subjects in the intervention group at their first contact with the clinic so that effects of training would be separated temporally from receiving the device. We offered all subjects standard VR so that any improvement in reading that might be attributed to education about rehabilitation strategies, information about remaining visual function, or simply contact with caring professionals would be balanced between the two groups. Tasks used as objective reading tasks in this study approximate “real world” goals such as reading continuous print, phone numbers, or amounts on bank checks. A crossover design, although an excellent study design to evaluate single-device use, was not selected for this pilot study because the transient use of a device may not approximate the real-world situation where one has access to device(s) indefinitely to use as much as one chooses.
Subjects were free to purchase devices that were demonstrated to them at any time in the rehabilitation process, as is typical for standard VR. Some patients are early adopters and quickly make choices of devices that can address their goals once options are outlined for them. Others require training or additional time until they choose to purchase and use devices.
As was hypothesized, access to a VM improved reading. It allowed improvement on reading of continuous print and fine print. Several findings, however, are of note. First, the objective improvement in reading speed is not paralleled in patient-reported subjective improvement in reading performance. Also, the patient-reported quality of life is not different in those who received the expensive video magnifier, than in those subjects who simply had the first step in the comprehensive vision rehabilitation process, the initial consultation. Improvement in well-being 1 month after the consultation was found when all subjects were considered. Those who had received the VM did not have greater gain in mood or perceived reading performance on the IVI reading subscale or AI reading questions. It is possible that receiving an expensive device at no cost reduces motivation and perceived success. Perhaps the 53-wpm improvement in reading speed on average in the subjects who received the video magnifier is not sufficient for subjects to perceive true success in day-to-day activities. It may be that the reading tasks, despite measured success, were still perceived as sufficiently difficult to not be reported as “successful.”
Considering all subjects, there was improvement in ability to read a check amount and a phone number over time. The VM group improved their ability to find and read a number in a phone book more than the VR group at 1 month (P = 0.02) but not a check amount (P = 0.17). This difference may reflect the relative success of subjects with reading checks at enrollment, that a video magnifier is not required for such a spot reading task, or that the number of enrolled subjects is not great enough to discover whether true differences exist. The phone number reading task was more difficult at enrollment than the check reading task, which may have allowed a ceiling effect for the check reading task.
Patients presenting for rehabilitation in this study had extreme difficulty reading. Reading rates are known to decrease with age and with eye disease. Legge et al reported that reading rates drop to one-fifth to one-third the rates of normally sighted adults in the setting of age-related ocular disease. Patients with low vision and central visual field loss read on average <50 wpm when using magnifiers.(20) Individuals without vision loss would be anticipated to read up to 300 wpm.(21) The increase in reading speed with the video magnifier was significant but did not approach normal reading speeds. This may have contributed to the finding that subjective reports of reading performance did not increase in those subjects with access to the VM.
Previous literature has outlined some benefit of video camera magnifiers. A Cochrane Review concluded that electronic devices tended to be preferred to optical ones.(5) More recently, a retrospective review by Nguyen et al of 530 vision rehabilitation patients reported improved reading speeds in patients who were prescribed low vision aids; 42% of the group received video camera magnifiers.(22) It is not stated whether there was a difference between those receiving video camera magnifiers or other aids. A recent trial in the Netherlands showed that use of a VM decreased reported difficulties with reading and fine work, but patient training on the use of the VM provided no more benefit than supplier provided instructions.(23) A current cross-over design study is comparing the use of a portable VM to using optical magnifiers (p-EVES).(24)
In this study there was a significant improvement in reported well-being when all subjects were considered and results adjusted for vision and demographic characteristics. The IVI well-being subscale includes questions about how much the subject perceives their vision to impact their ability to cope and emotions such as frustration. It is reasonable that the initial consultation, as the initial step in comprehensive vision rehabilitation, where options and future plans to assist the individual are outlined, would positively impact one’s perception of ability to cope. In 2007 Lamoureux et al reported significant improvement in IVI well-being subscale after rehabilitation as well as improvement on both total score and reading subscales.(25) It is of interest that no improvement on the mobility subscale was reported previously using this instrument post multidisciplinary low-vision rehabilitation.(25,26) Although not significant, our results did show improvement on the mobility score. This change on the mobility score may seem counterintuitive, because the intervention group received a reading device; however, two comments by study subjects may be informative. One subject reported that he was not using the bus when he enrolled in the study because he could not read the bus schedules, but once he had the device and could easily read the schedule he returned to going out on the bus. Another subject reported that he was more active planting a garden once he had the VM and could read seed packages. Reading is an integral part of many activities of daily living, and it is feasible that enhanced reading could augment activity and mobility.
Limitations of this study include the small sample size, that an adaptive design was not used to balance the scotoma patterns in each group, that subjects receiving only standard care knew they would receive a VM after the completion of rehabilitation training, that we did not explicitly encourage all subjects to choose the device of their choosing for each reading task, that the same spot reading tasks were repeated, and that there was no control group that did not receive any rehabilitation. Withholding care raises ethical issues as even waitlist controls have been shown to have deterioration in self-reported visual performance. Hence, using standard care as a comparison group is practical and fairer. Patients in the VM group may have had more comorbidities affecting reading practice or device use.
This exploratory study raises further issues to be investigated in future confirmatory research. Future studies will consider the time frame after one month (T3-T5). Future studies can measure the time that patients use their devices at home for reading and other tasks to determine whether improvement in reading performance is related to practice with the device or even reading practice. It can also consider whether training with the device changes patient-reported reading performance. Macular perimetry testing and categorization of scotoma patterns remains largely unstandardized in clinical settings and future consensus on testing and quantification of central visual field will be beneficial. | | | Acknowledgements | Grants/Funding: Devices provided by Optelec USA.
Clinical trial number: NCT01670643. | | | References | 1. Owsley C, McGwin G Jr, Lee PP, Wasserman N, Searcey K. Characteristics of low-vision rehabilitation services in the United States. Arch Ophthalmol 2009;127:681-9.
2. Kaldenberg J, Flax M. Evaluation and Intervention For Deficits In Reading and Writing. In M. Warren (Ed) Self Paced Clinical Course: Low Vision: Occupational Therapy Evaluation and Intervention with The Older Adult. Bethesda: AOTA Press; 2008.
3. Friedman DS, O’Colmain B, Muñoz B, et al; Eye Diseases Prevalence Research Group. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol 2004;122:564-72.
4. Binns AM, Bunce C, Dickinson C, et al. How effective is low vision service provision? A systematic review. Surv Ophthal 2012;57:34-65.
5. Virgili G, Acosta R, Grover LL, et al. Reading aids for adults with low vision. Cochrane Database Syst Rev 2013;10:CD003303.
6. Trauzettel-Klosinski S, Dietz K. Standardized assessment of reading performance: the New International Reading Speed Texts IReST. Invest Ophthalmol Vis Sci 2012;53:5452-61.
7. Lamoureux EL, Pallant JF, Pesudovs K, Hassell JB, Keeffe JE. The Impact of Vision Impairment Questionnaire: an evaluation of its measurement properties using Rasch analysis. Invest Ophthalmol Vis Sci 2006;47:4732-41.
8. Weih LM, Hassell JB, Keeffe J. Assessment of the impact of vision impairment. Invest Ophthalmol Vis Sci 2002;43:927-35.
9. Massof RW, Ahmadian L, Grover LL, et al. The Activity Inventory: an adaptive visual function questionnaire. Optom Vis Sci 2007;84:763-74.
10. Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav Res Ther 1997;35:79-89.
11. Andrich D. A rating formulation for ordered response categories. Psychometrika 1978;43:561-73.
12. Linacre JM. A User’s Guide to Winsteps: Rasch-Model Computer Program. Chicago: Mesa Press; 2002.
13. Mallinson T. Why measurement matters for measuring patient vision outcomes. Optom Vis Sci 2007;84:675-82.
14. Lamoureux E, Pesudovs K. Vision-specific quality-of-life research: a need to improve the quality. Am J Ophthalmol 2011;151:195-7.
15. American Academy of Ophthalmology Vision Rehabilitation Committee. Preferred Practice Pattern® Guidelines. Vision Rehabilitation for Adults. San Franciso, CA: American Academy of Ophthalmology; 2012. Available at: www.aao.org/ppp.
16. Stelmack JA, Tang XC, Reda DJ, Rinne S, Mancil RM, Massof RW; LOVIT Study Group. Outcomes of the Veterans Affairs Low Vision Intervention Trial (LOVIT). Arch Ophthalmol 2008;126:608-17.
17. Jackson ML, Wallis J, Schoessow K, Drohan B, Williams K. Visual function in the “oldest-old” 1 year after comprehensive vision rehabilitation. J Am Geriatr Soc 2012;60:183-5.
18. Pijnacker J, Verstraten P, van Damme W, Vandermeulen J, Steenbergen B. Rehabilitation of reading in older individuals with macular degeneration: a review of effective training programs. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn 2011;18:708-32.
19. Gaffney AJ, Margrain TH, Bunce CV, Binns AM. How effective is eccentric viewing training? A systematic literature review. Ophthal & Physio Opt 2014;34:427.437.
20. Legge GE, Pelli DG, Rubin GS, Schleske MM. Psychophysics of reading—I. Normal vision. Vision Res 1985;25:239-52.
21. Akutsu H, Legge GE, Ross JA, Schuebel KJ. Psychophysics of reading—X. Effects of age-related changes in vision. J Gerontol 1991;46:325-31.
22. Nguyen NX, Weismann M, Trauzettel-Klosinski S. Improvement of reading speed after providing of low vision aids in patients with age-related macular degeneration. Acta Ophthalmol 2009;87:849-53.
23. Burggraaff MC, van Nispen RM, Hoeben FP, Knol DL, van Rens GH. Randomized controlled trial on the effects of training in the use of closed-circuit television on reading performance. Invest Ophthalmol Vis Sci 2012;53:2142-50.
24. Taylor J, Bambrick R, Dutton M, et al. The p-EVES study design and methodology: a randomised controlled trial to compare portable electronic vision enhancement systems (p-EVES) to optical magnifiers for near vision activities in visual impairment. Ophthalmic Physiol Opt 2014;34:558-72.
25. Lamoureux EL, Pallant JF, Pesudovs K, Rees G, Hassell JB, Keeffe JE. The effectiveness of low-vision rehabilitation on participation in daily living and quality of life. Invest Ophthalmol Vis Sci. 2007;48:1476-82.
26. Wang BZ, Pesudovs K, Keane MC, Daly A, Chen CS. Evaluating the effectiveness of multidisciplinary low-vision rehabilitation. Optom Vis Sci 2012;89:1399-408.
| |
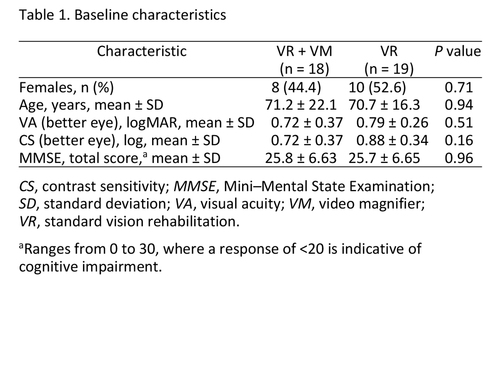
Table 1
|
|

Table 2
|
|
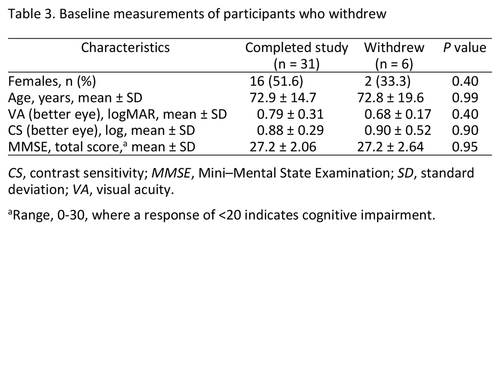
Table 3
|
|
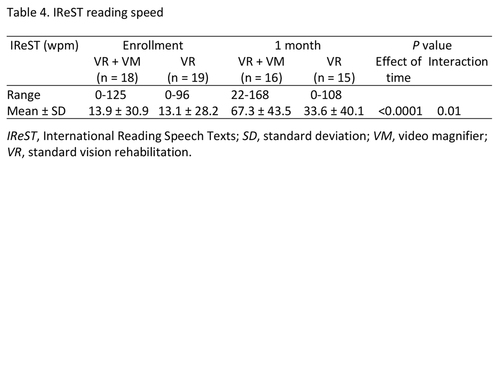
Table 4
|
|
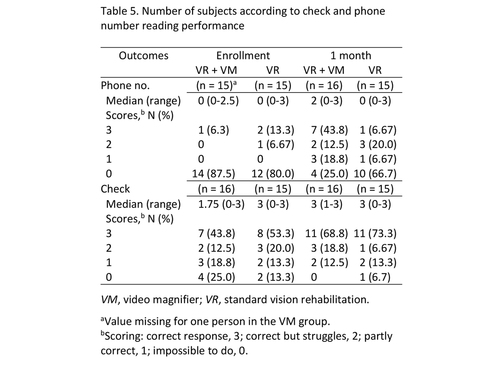
Table 5
|
|

Table 6
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in