|
|
 |
 |
 |
 |
|
|
The effect of lubricating eye drops on optical coherence tomography imaging of the retina
Digital Journal of Ophthalmology 2009
Volume 15, Number 2
May 30, 2009
|
Printer Friendly
Download PDF |
|
|
|
|
| Abstract | Introduction: The goal of this study was to examine the potential value of corneal lubrication in improving the quality of optical coherence tomography (OCT) imaging of the retina.
Materials and Methods: This study is a consecutive series of 13 eyes of 11 patients in whom repeated attempts at OCT imaging failed to yield a good quality study despite the absence of significant media opacity or inadequate pupil dilation. Immediately following several poor quality scans, each eye received lubricating eye drops. The quality of images before and after the administration of drops was assessed.
Results: A statistically significant improvement in OCT image quality was observed following the administration of eye drops in each case. The change in mean signal strength (SS) was from 4.35 to 6.26 (p= 0.0002). The proportion of scans with erroneous edge detection decreased from 41 to 13 percent.
Discussion: Lubricating drops appear to improve the quality and feasibility of OCT imaging in selected cases.
Key Words: Corneal dryness, lubricating eye drops, optical coherence tomography, OCT. | | | Introduction | | Optical coherence tomography (OCT) imaging has revolutionized the practice of ophthalmology especially in the fields of glaucoma and retina. However, poor image quality can lead to unreliable quantitative data, misdiagnosis, difficulty with treatment decisions, and inability to follow the course of disease due to limitations in reproducibility. OCT image quality has been shown to be adversely affected by corneal drying.(1) Lubricating eye drops would be a simple and inexpensive way to enhance image quality and reproducibility in selected patients. | | | Materials and Methods | Approval for this study was obtained from the Institutional Review Board at the University of Virginia. This study is a consecutive series of 13 eyes of 11 patients in whom repeated attempts at OCT imaging failed to yield a good quality study despite the absence of significant media opacity or inadequate pupil dilation. All scans were performed by a trained technician on the same OCT machine (OCT Stratus, Third Generation, Model 3000, software 4.0, Carl Zeiss Ophthalmic Systems, Dublin, CA, USA). For the purpose of this study, an OCT study was considered of good quality if at least four of six (for fast macular imaging) or two of three (for nerve fiber layer imaging) scans had correct edge detection and a signal strength of greater than 6.0. Correct edge detection refers to the correct identification of the inner and outer retinal or retinal nerve fiber layer boundaries by the OCT software thus allowing accurate thickness measurements. Signal strength is the proprietary OCT software parameter for image quality based on signal-to-noise ratio and the uniformity of the signal across a scan.(2) Immediately following 1 to 4 poor quality scans, each eye received a single lubricating eye drop (Systane lubricant eye drops, Alcon) just before reattempting image acquisition using the same OCT parameters.
The quality of images before and after the administration of eye drops was assessed. Data recorded included retinal nerve fiber layer (RNFL) thickness, macular thickness measurements, signal strength (SS), and the number of scans with failed edge detection. Statistical analysis was performed using paired and unpaired t-tests. | | | Results | Patient demographics, ocular diagnoses and imaging details are listed in the Table. Of the 11 patients, 6 were male, 5 were female, and the mean age was 61 years. One patient carried a diagnosis of dry eye syndrome, one patient had blepharitis and was noted to have punctate epithelial erosions the day of the scan, and another patient had map-dot-fingerprint corneal dystrophy. The other patients had no documented tear film or corneal abnormalities that would place them at risk for surface irregularity.
A statistically significant improvement in OCT image quality was observed following the administration of eye drops in each case. In all but one eye, this was possible on the first attempt following application of the lubricating drops. The change in mean signal strength (SS) was from 4.35 to 6.26 dB (p= 0.0002) (Figure 1). The proportion of studies with an average SS greater than 6 increased from 1.1 percent before to 67 percent after eye drop application. Statistical significance was maintained even when the scan with the best SS prior to eye drop application was chosen for comparison. Six of 13 eyes had scans with correct edge detection before drops despite poor signal strength. After drops, 12 of 13 eyes had scans with proper edge detection. The proportion of scans with erroneous edge detection decreased from 41 to 13 percent (Figure 2A and 2B). In the 7 eyes with edge detection error before drops, the average retinal nerve fiber layer thickness in focal sectors (1/12 pie on the OCT report) affected by the error was 12.4 micrometers. Following eye drop application and restoration of correct edge detection, the average thickness in these areas increased to 48.25 micrometers (p=0.00004). | |
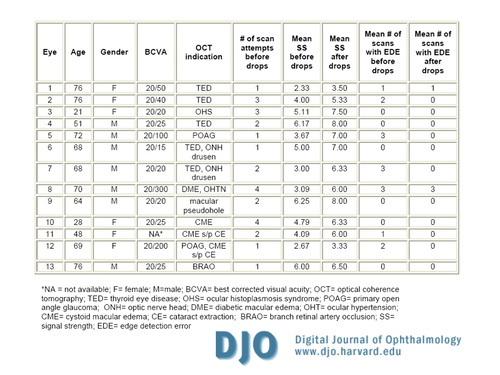
Table
Patient demographics and results.
|
|
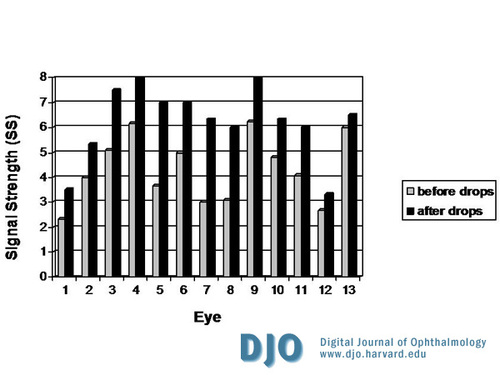
Figure 1
Change in mean optical coherence tomography signal strength (SS) before and after lubricating eye drops. The SS significantly increased in every case following the application of drops.
|
|

Figure 2
Edge detection before (A) and after (B) lubricating eye drops in the same eye undergoing optical coherence tomography for retinal nerve fiber layer (RNFL) imaging. Note image degradation with reduction in reflectivity of the RNFL with associated failure of edge detection and collapse of the border detection lines (A). Following application of a single drop of artificial tears during the same imaging session, improvement in signal strength and image quality (B) with associated proper edge detection was noted at the first attempt at re-imaging.
|
|
| Discussion | Image quality is essential for the accurate interpretation of OCT test results. Several studies have analyzed error and reproducibility of OCT measurements,(3-6) but few have investigated the role of the tear film. Because OCT is a light-based imaging system, image quality may be degraded secondary to the scattering of light by the rough surface of a dry cornea. Stein et al. used eyelid taping to demonstrate the effect of corneal drying on OCT image quality.(1) They found a significant deterioration of image quality following induced corneal exposure with lid taping; furthermore, image quality slowly recovered after patients were allowed to blink.
The patients in our study demonstrated persistently decreased image quality even in the absence of significant media opacity or poor pupillary dilatation. Lubricating eye drops improved scan quality immediately after the drops were applied. This is most likely due to the restoration of a smooth optical corneal surface following drop application. Following application of eye drops, the proportion of scans with erroneous edge detection placement decreased from 41 to 13 percent (Figure 2A and 2B). We believe this to be related to the associated improvement in SS. When the SS is poor (Figure 2A), the OCT cross sectional image may be degraded so that the retinal or retinal nerve fiber layer boundaries may not be distinct enough for proper edge detection, leading to collapse of the border detection lines (Figure 2) with subsequent decreased thickness measurements and poor reproducibility of imaging studies.(1) Restoration of proper edge detection can explain the statistically significant increase in focal thickness measurements observed following drop application in some of our patients.
The major limitations of our study include the lack of a control group and the small sample size. Our study also had a high proportion of patients with thyroid eye disease, most of whom received nerve fiber layer scans for suspected optic neuropathy. Such eyes are predisposed to dry eyes, and in future studies, we plan to analyze data regarding objective measures of dry eyes in these patients such as Schirmer’s testing and tear break-up time. Another limitation in our study is that we did not systematically measure pupil size at the time of imaging; however, all eyes were clinically judged to be well-dilated. Moreover, the significant improvement in image quality following drop application makes pupil size an unlikely confounder.
This small series suggests that lubricating drops appear to improve the quality and feasibility of OCT imaging in selected cases. Eyes with poor quality OCT imaging of the fundus with no apparent cause may benefit from the administration of lubricating drops just before image acquisition even in the absence of dry eye syndrome. We currently keep a bottle of artificial tears available on the OCT machine table for potential use in such cases. | | | References | 1. Stein DM, Wollstein G, Ishikawa H, et al. Effect of corneal drying on optical coherence tomography. Ophthalmology 2006; 113:985-91.
2. Stein DM, Ishikawa H, Hariprasad R, et al. A new quality assessment parameter for optical coherence tomography. Br J Ophthalmol 2006; 90:186-90.
3. Olmedo M, Cadarso-Suarez C, Gomez-Ulla F, et al. Reproducibility of optic nerve head measurements obtained by optical coherence tomography. Eur J Ophthalmol 2005; 15:486-92.
4. Polito A, Del Borrello M, Isola M, et al. Repeatability and reproducibility of fast macular thickness mapping with stratus optical coherence tomography. Arch Ophthalmol 2005; 123:1330-7.
5. Ray R, Stinnett SS, Jaffe GJ. Evaluation of image artifact produced by optical coherence tomography of retinal pathology. Am J Ophthalmol 2005; 139;18-29.
6. Sadda SR, Wu Z, Walsh AC, et al. Errors in retinal thickness measurements obtained by optical coherence tomography. Ophthalmology 2006; 113:285-93. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in