|
|
 |
 |
 |
 |
|
|
Visual and anatomic outcomes of vitreoretinal surgery: results at the Boston VA and a review of the literature
Digital Journal of Ophthalmology 2009
Volume 15, Number 1
March 17, 2009
|
Printer Friendly
Download PDF |


 Nicole C. Hanley-Williams, MD
Nicole C. Hanley-Williams, MD | Boston University School of Medicine, Boston, MA USA Manju L. Subramanian, MD | Boston University School of Medicine, Boston, MA and Veterans Administration Medical Center, Boston, MA, USA Edward B. Feinberg, MD, MPH | Boston University School of Medicine, Boston, MA and Veterans Administration Medical Center, Boston, MA, USA
|
|
|
| Abstract | Introduction: The veteran population presents unique challenges in the management of vitreoretinal disorders. We compiled the surgical outcomes for the most common visually significant vitreoretinal diagnoses. Those results were then compared to visual and anatomic outcomes established in the literature.
Materials and Methods: Medical records over a three-year time period, from January 2005 through December 2007, were reviewed for 208 persons who underwent vitreoretinal surgery for vitreous hemorrhage, retained lens fragment, rhegmatogenous and tractional retinal detachment, macular hole, and macular pucker at the Jamaica Plain Campus of the Veterans Affairs Boston Healthcare System in Boston, MA. A comprehensive search of the literature was conducted on Medline. Data from several large case series and meta-analyses were compared to results obtained at the VA Boston.
Results: A total of 208 veterans underwent vitreoretinal surgery from January 2005 to December 2007. After excluding those with rare diagnoses and lack of adequate follow-up data, the outcomes of 181 vitreoretinal procedures were included in this study.
Discussion: Overall, veterans at a regional referral center in Boston demonstrate postoperative visual and anatomic outcomes comparable to outcomes reported in the ophthalmic literature. | | | Introduction | The Veterans Affairs Boston Healthcare System is the regional referral center for medical and surgical management of vitreo-retinal diseases for all veterans in the New England area. Patients are drawn from areas as far as northern Maine, Vermont, New Hampshire, and Rhode Island. Serving a largely senior veteran population, many of whom travel long distances for their care, veterans can present special social and diagnostic challenges in managing core eye diseases. Many veterans, being from remote areas, may go several years without a screening eye examination.(1) Difficulty in accessing care may result in more complicated medical and surgical eye diseases such as cataracts, diabetic retinopathy, hypertensive retinopathy, and age-related macular degeneration. In a diabetic veteran population, the prevalence of vitreo-retinal disorders and preventable blindness can be as high as 9.5% and 2.7%, respectively.(2) Alternatively, prevalence of vision-threatening retinopathy in the general US adult diabetic population is 8.2%.(3) These advanced ophthalmic disease entities, combined with advanced systemic co-morbidities, can potentially affect surgical outcomes.
Some of the commonly managed diagnoses requiring surgical intervention at the Veterans Administration Hospital in Boston include non-clearing vitreous hemorrhage from diabetes, retained lens fragments, tractional and rhegmatogenous retinal detachment, macular hole, and epiretinal membranes. In this series we examined the visual outcomes of veterans undergoing vitreo-retinal surgery for these disorders. We then performed a comprehensive search in Medline, looking at detailed outcome data from numerous case series, review articles, and meta-analyses for each diagnosis. As expected, there is variability in the literature regarding visual and anatomic outcomes from vitreo-retinal surgery. This can be due to a number of factors, which include but are not limited to, the stage of disease at the time of diagnosis, the status of the macula, co-existing ocular or systemic disease, preoperative vision, and the presence and frequency of postoperative complications. There are copious and detailed data in the literature describing the results of vitreo-retinal surgery for at least four of the six of the aforementioned diagnoses, many of which are included in this article. However, we acknowledge that a comprehensive review and meta-analyses of all of the data for every common vitreo-retinal diagnosis is simply not possible to present in a single manuscript. For the purposes of this article, we have favored data from selected meta-analyses and review articles offering anatomic and visual outcomes of surgery for the more common vitreo-retinal disorders as a frame of reference. Articles were excluded if they were non-english and the corresponding abstract failed to provide the needed information. The data obtained from the literature were then compared to the visual and anatomic outcomes of veterans undergoing vitreo-retinal surgery at the Boston VA. Hence, this review will serve two purposes: 1) to offer a general overview of the literature describing surgical outcomes for common vitreo-retinal disorders, and 2) to help provide a standard of comparison for the outcomes of veterans in the New England area receiving surgical vitreo-retinal care in the Veterans Administration system. | | | Materials and Methods | Data Collection
The electronic medical records were reviewed for all patients undergoing vitreo-retinal surgery at the Veterans Affairs Boston Healthcare System between January 2005 and December 2007. As this was, in part, a review article based on data gathered in a retrospective chart review, Institutional Review Board approval was obtained but informed consent was waived. Data were recorded in an ongoing fashion in order to track visual and anatomic outcomes for surgeons. For each case, the Snellen visual acuity was recorded pre-operatively and post-operatively at day one, month one, month three and month six after surgery. Complications occurring during this period were also recorded. In addition, each patient's significant co-morbidities and ocular history were also recorded. Each case was followed to the absolute post operative period. The absolute post-operative period is defined as the time period to obtain the final visual acuity, and this time period differed for each patient. The best corrected visual acuity or the best visual acuity with correction was recorded at each post-operative month.
Data Analysis
The most common preoperative diagnoses for our veterans were diabetic vitreous hemorrhage, retained lens fragment, rhegmatogenous and tractional retinal detachment, macular hole, and epiretinal membranes. The diagnoses of epiretinal membrane and vitreo-macular traction were combined to form one group. For each case, the preoperative visual acuity was compared with the best visual acuity during the absolute postoperative period to obtain the number of lines of improvement in vision. Both the pre-operative and post-operative visual acuities were converted to logMAR equivalents based on the method described by J. Holladay.(4) For each diagnostic group, the mean, median, and standard deviation were calculated for the number of lines of improvement, pre-operative logMAR equivalent, post-operative logMAR equivalent, and post-operative month during which the best visual acuity was recorded. The mean logMAR equivalent for each diagnostic group was subsequently converted back into Snellen visual acuity. Cases in which the pre-operative or post-operative visual acuity was recorded as light perception (LP) or no light perception (NLP) were excluded from the visual outcome data because LP and NLP cannot be converted to logMAR equivalents. However, these cases were subsequently included in the stratification of visual outcomes shown in Table 3, and they were also included in Table 4 (complications) to aide in giving a more accurate assessment of outcomes. Other exclusionary criteria were: lack of recorded manifest refraction during the absolute post-operative period, lack of recorded visual acuity with correction in the absolute post-operative period, and having insufficient follow up in the post-operative period due to either death or missed appointments. | | | Results | A total of 208 veterans underwent vitreo-retinal surgery from January 2005 to December 2007 at the Veterans Affairs Boston Healthcare System. Sixteen (7.7 percent) subjects were excluded because they had relatively rare disorders. An additional 31 patients (15 percent) were excluded because of being lost to follow up or having an incalculable preoperative or postoperative visual acuity (9 and 6 percent, respectively). As a result, 172 operations of 161 eyes were included when calculating visual outcomes in terms of fractionated snellen acuities and lines of improvement. While reporting stratified, non-fractionated snellen visual outcomes and major complications, the 9 procedures with incalculable pre-operative or post-operative vision (LP or NLP) were subsequently included (see Table 4), for a sum of 181 vitreo-retinal procedures.
Table 1 describes the demographic characteristics of the patients, including mean and median age for each group of patients. As this study was conducted at a Veterans Administration Hospital, over 95 percent of all patients are male. Tables 2, 3, and 4 summarize the results and major complications for each study group. The visual outcomes are outlined in detail within each of the tables. Table 2 describes mean pre-operative and post-operative vision, as well as the mean and median lines improved for each diagnosis. Table 3 stratifies the final visual outcomes, and includes those patients with incalculable vision (LP and NLP). Table 4 describes the major post-operative complication rates. Table 5 conveys results of sample case series from original articles and meta-analyses describing the outcomes of vitreo-retinal surgery for each diagnosis. | |
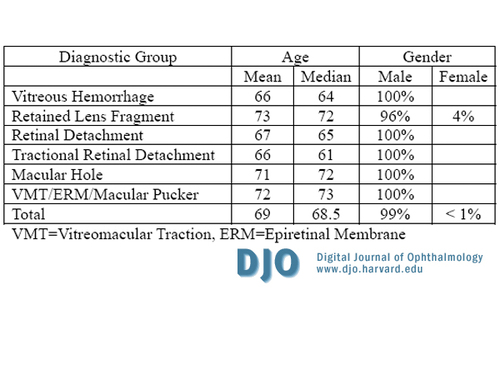
Table 1
Patient demographics for veterans undergoing vitreo-retinal surgery between January 2005 and December 2007 at the Veterans Affairs Boston Healthcare System.
|
|
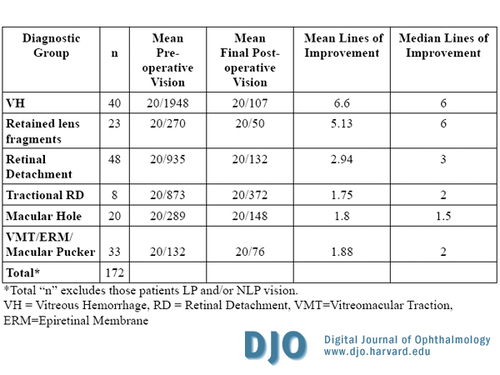
Table 2
Visual outcomes for each diagnostic group of veterans who underwent vitreo-retinal surgery at the Veterans Affairs Boston Healthcare System.
|
|
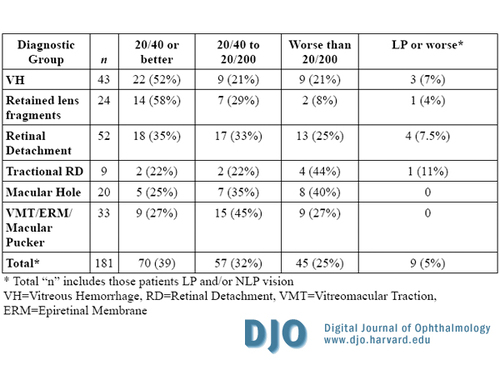
Table 3
Visual outcomes stratified by visual acuity for each diagnostic group of veterans.
|
|
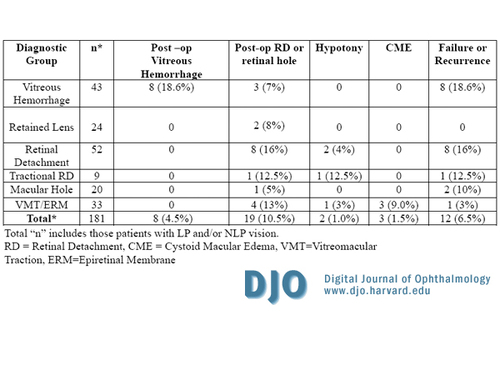
Table 4
Major complication rates from vitreo-retinal surgery at the Veterans Affairs Boston Healthcare System.
|
|

Table 5
Visual Outcomes from sample articles from a review of the literature.
|
|

Table 6
Visual outcomes for the retinal detachment diagnostic group of veterans receiving vitreo-retinal surgery at the Veterans Affairs Boston Healthcare System.
|
|
| Discussion | Vitreous Hemorrhage
The most common underlying diagnosis for vitreous hemorrhage is proliferative diabetic retinopathy.(5) All patients who underwent surgery for vitreous hemorrhage in this case series had underlying diabetic retinopathy. There is a paucity of data in the literature describing the outcomes of vitrectomy for diabetic vitreous hemorrhage. Only one case series was found which looked solely at vitreous hemorrhage outcomes in a similar fashion to our case series, and it showed a wide range of results, from better than 20/50 to worse than 20/400.(6) The variability in visual outcomes is likely due to the presence of co-existing diabetic eye disease, such as neovascularization leading to a retinal detachment. Table 5 includes a breakdown of visual outcomes from the case series (Cooper et al.) of patients who underwent vitrectomy for non-clearing vitreous hemorrhage. These results show outcomes that are similar to our series of patients.(6)
Retained Lens Fragments
Most patients with retained lens fragments do well following vitrectomy, with the majority of patients having a final visual acuity of 20/40 or better.(7-11) Analysis of retrospectively reviewed, large non-comparative case series show that significant predictors of good final visual acuity include good preoperative vision, presence of an intraocular lens, and an uncomplicated intraoperative and post-operative course.(12) Our case series is consistent with that reported in the literature, with 58 percent achieving a final vision of 20/40 or better.
Retinal Detachments
In general, visual outcome analyses for retinal detachment repair are often difficult to track and compare. This is because several factors impact the overall visual outcome of surgery for a retinal detachment. The most important preoperative predictor is the status of the macula. Other factors include lens status, presence of symptoms, signs of chronicity, and presence of proliferative vitreo-retinopathy. To further complicate the scenario, the type of procedure selected by the surgeon (i.e. primary vitrectomy, pneumatic retinopexy, scleral buckle, or combination procedure), and the rationale that is used in determining the ideal approach, affects the overall outcome. All of the aforementioned factors, in addition to other unknown factors, may prevent a thorough exploration and control for heterogeneity between the studies. As a result, we were unable to convey (in Table 5) visual outcomes for retinal detachment repair from the literature in the same manner as the other diagnoses.
Instead, we offer data from the literature looking at outcomes for retinal detachment repair in a dual fashion - visual and anatomic outcomes. The literature has shown that the visual outcomes for retinal detachment repair range between 20/50 and 20/200.(13-16) In pseudophakic patients, reports have cited that repair with primary vitrectomy has yielded a single operation anatomic success rates between 50-95 percent.(17-24) Patients undergoing pneumatic retinopexy have anatomic success rate between 68-73 percent after a single procedure.(25-27) Patients undergoing scleral buckling for retinal detachment have a success rate of 80-86 percent after a single procedure.(28-31) Approximately 52 patients in this case series underwent surgical repair for rhegmatogenous retinal detachment at the VA Boston. All of the patients underwent either primary vitrectomy, scleral buckle, or combination of scleral buckle and vitrectomy. Eighty-four percent of patients achieved anatomic success after a single operation, leaving a 16 percent re-detachment rate. About 35 percent of patients achieved a final vision of 20/40 or better. Table 6 shows a breakdown of the preoperative and postoperative vision based on status of the macula and the type of procedure. Overall, these data suggest that anatomic and visual outcomes from repair of retinal detachments at the Boston VA seem to fall within the standards reported in the literature.
Tractional Retinal Detachment
The surgical treatment of tractional retinal detachment is an individual matter that is influenced by the preoperative findings on examination, patient characteristics, use of a wide variety of available tools and techniques for surgery, and the experience and ability of the retinal surgeon. The nature of tractional retinal detachments, in the setting of advanced diabetic retinopathy, unsurprisingly will often lead to poor visual outcomes. Our series looked at 9 patients who underwent vitrectomy for tractional retinal detachment. Visual outcomes were modest, but due to a small number of cases, it is difficult to compare these outcomes to those reported in the literature.
Macular Holes
Surgical repair for full thickness macular holes (Stages 2, 3 and 4) has been well studied. Stage 1 macular holes are typically treated with observation, although reports of surgical intervention for stage 1b have yielded good anatomic and visual results.(32) Patients with macular holes who elect surgical intervention typically complain of distortion and difficulty reading. While anatomic success and relief of distortion is often achieved following surgery, the degree of improvement in visual acuity on the Snellen chart is often less proportionate and incongruous with anatomic results. This variability in visual outcomes can be due to preoperative staging, length of symptoms, lens status of the patient, use of adjuvants such as indocyanine green to assist in intraoperative peeling, and type of procedure selected by the surgeon. Following prompt surgical intervention for treatment of a stage 3 or 4 macular hole, vision can improve to better than 20/40 in 22-49 percent of patients.(33-35) Other meta-analyses have shown improvement to 20/40 or better in 27-72 percent (Table 5).(36) Anatomic success, seen as closure or flattening of the edges, is achieved in 80 percent of cases.(31-34) Length of post-operative recovery is variable. Optical coherence tomography demonstrates that the significant improvement in macular configuration can take up to six months.(37) Patients at the Boston VA (n=20) who underwent repair of their macular hole showed an anatomic closure rate of 90 percent. Twenty-five percent of these patients achieved a final visual acuity of 20/40 or better (Table 3).
Epiretinal Membranes/Vitreomacular Traction Syndrome
It has been reported that epiretinal membranes frequently occur in conjunction with vitreo-macular traction.(38) However, the exact nature of this relationship is yet to be determined. As such, we combined the diagnoses of vitreomacular traction and macular pucker. Patients who develop epiretinal membranes will often complain of visual distortion similar in degree to those with macular holes. Surgical repair often does not require intraoperative infusion of gas nor postoperative prone positioning, as it does with macular holes. As with other vitreo-retinal disorders, final postoperative vision in patients undergoing vitrectomy for macular pucker is dependent on a number of factors, such as preoperative vision, duration of symptoms, presence of macular edema, and intraoperative and postoperative courses. Anatomic success is often conveyed as the presence or absence of the membrane, any associated macular edema, or development of recurrence. This is determined by clinical examination and confirmed by optical coherence tomography (OCT). In the case of epiretinal membranes, visual outcomes can be as good as 20/40.(39-41) One report looked at visual outcomes for 125 patients who underwent surgery for macular pucker and showed that 39 percent had a final vision of 20/40 or better (Table 5).(42)
Thirty-three patients underwent surgery at the Boston VA for removal of symptomatic epiretinal membrane. Of those, 9 patients (27 percent) had a final vision of 20/40 or better, 15 (45 percent) had a final vision between 20/40 and 20/200, and the remainder had vision worse than 20/200.
The Veterans Affairs Boston Healthcare System is the only VA facility in New England that provides surgical vitreo-retinal care. As such, it draws veterans from a large geographic area to provide care for advanced surgical vitreo-retinal disorders that significantly affect vision. Veterans who live in remote areas of New England will often have difficulty keeping appointments and maintaining ongoing care of chronic disorders. This can lead to potentially challenging diagnostic and therapeutic scenarios. It should be noted that geographical diversity of population, multitude of vitreo-retinal surgeons, the type of procedure selected by the operating surgeon, the perceived complexity of the diagnosis, variations in intra-operative course, co-morbidities, and other unknown factors impact the eventual outcome and prognosis for vision. However, these issues pertaining to diversity is consistent with actual clinical practice. Moreover, it gives insight to improving the care of patients.
There are limitations present in this case series. The first include the retrospective nature of the study and the inherent bias associated with it. In addition, the exclusion of patients whose preoperative or final postoperative visual acuity was LP or NLP (due to difficulty in converting the fractionated visual acuities to LogMar equivalents for analysis of mean visual acuities), should be recognized as potentially skewing the data favorably. Moreover, the outcomes reported from the literature serve as a historical cohort and frame of reference for comparison, and the authors acknowledge that this is not as meaningful as performing a meta-analysis for all 6 diagnoses studied in this article. Finally, the patient population at the VA is different in terms of demographic characteristics (mostly male patients), making extrapolation of data to females more difficult.
Surgical intervention for each vitreo-retinal diagnosis at the Boston VA appears to demonstrate postoperative improvement in both mean and median visions (Table 2). Overall, this review offers some reassurance that surgical outcomes for veterans undergoing vitreo-retinal surgery for common diagnoses were generally consistent with visual and anatomic outcomes and standards of care established in the literature. | | | References | 1. Newcomb RD. Prevalence of undiagnosed eye/vision disorders in a VA Hospital. Journal of the American Optometric Association 1976;47:1145-1150.
2. Orcutt J, Arpenik A, Koepsell TD, Maynard C. Eye disease in Veterans with diabetes. Diabetes Care 2004;27:B50-B53.
3. The Eye Disease Research Prevalence Research Group. The prevalence of diabetic retinopathy among adults in the United States. Arch of Ophthalmol 2004; 122:552-563.
4. Holladay, JT. Proper Method for Calculating Average Visual Acuity. Journal of Refractive Surgery 1997;13:388-391.
5. Goff MJ, McDonald HR, Johnson RN, Ai E, Jumper JM, Fu AD. Causes and treatment of vitreous hemorrhage. Compr Ophthalmol Update 2006;7(3):97-111.
6. Cooper B, Shah GK, Grand GM, Bakal J, Sharma S. Visual Outcomes and Complications after Multiple Vitrectomies for Diabetic Vitreous Hemorrhage. Retina 2004;24:19-22.
7. Ho SF, Zaman A. Clinical Features and Outcomes of Pars Plana Vitrectomy in Patients with Retained Lens Fragments after Phacoemulsification. J Cataract Refract Surg 2007;33:2106-2110.
8. Merani R, Hunyor AP, Playfair TJ, et al. Pars Plana Vitrectomy for the Management of Retained Lens Material after Cataract Surgery. Am J Ophthalmol 2007;144:364-370.
9. Hansson LJ, Larsson J. Vitrectomy for Retained Lens Fragments in the Vitreous after Phacoemulsification. J Cataract Refract Surg 2002;28:1007-1011.
10. Chen CL, Wang TY, Cheng JH, et al. Immediate pars plana vitrectomy improves outcome in retained intravitreal lens fragments after phacoemulsification. Ophthamlologica 2008;222(4):277-83.
11. Murat UO, Kapran Z, Akkan F, et al. Vitreoretinal surgery for retained lens fragments after phacoemulsification. Eur J Ophthalmol 2003;13(1):69-73.
12. Scott IU, Flynn HW Jr, Smiddy WE, et al. Clinical features and outcomes of pars plana vitrectomy in patients with retained lens fragments. Ophthalmology 2003;110(8):1567-72.
13. Noemi L, Wong D. Major Review: Pseudophakic Retinal Detachment. Survey of Ophthalmology 2003;48:467-487.
14. Tseng W, Cortez RT, Ramirez G, et al. Prevalence and Risk Factors for Proliferative Vitreoretinopathy in Eyes with Rhegmatogenous Retinal Detachment but no Previous Vitreoretinal Surgery. Am J Ophthal 2004;137:1105-1115.
15. Arya AV, Emerson JW, Englebert M, et al. Surgical Mangagement of Pseudophakic Retinal Detachments: a meta-analysis. Ophthalmology 2006;113 (10): 1724-33.
16. Heimann H, Bartz-Schmidt KU, Bornfeld N, et al. Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study Group. Ophthalmology 2007;114(12): 2142-54.
17. Greven CM, Sanders RJ, Brown GC, et al. Pseudophakic retinal detachments: anatomic and visual results. Ophthalmology 1992;99:257–262.
18. Haddad WM, Monin C, Morel C, et al. Retinal detachment after phacoemulsification: a study of 114 cases. Am J Ophthalmol 2002;133:630–638.
19. McHugh D, Wong D, Chignell A, et al. Pseudophakic retinal detachment. Graefes Arch Clin Exp Ophthalmol 1991;229:521–525.
20. Ranta P, Kivelä T. Functional and anatomic outcome of retinal detachment surgery in pseudophakic eyes. Ophthalmology 2002;109:1432–1440.
21. Frau E, Sam H, Korobelnik JF, et al. Retinal detachment after cataract surgery: retrospective study of 57 cases. Eur J Ophthalmol 1993;3:177–180.
22. Vatne HO, Syrdalen P. Retinal detachment after intraocular lens implantation. Acta Ophthalmol (Copenh) 1986;64:544–546.
23. Girard P, Karpouzas I. Pseudophakic retinal detachment: anatomic and visual results. Graefes Arch Clin Exp Ophthalmol 1995;233:324–330.
24. Senn P, Schmid MK, Job O, et al. Primäre Pars-plana-Vitrektomie zur Behandlung der Pseduophakieamotio—eine retrospective Studie über 129 Fälle. Klin Monatsbl Augenheilkd 2002;219:226–230.
25. Tornambe PE, Hilton GF, Brinton DA, et al. Pneumatic Retinopexy. A two-year follow-up study of the multicenter clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology 1991 Jul;98(7):1115-23.
26. Mulvihill A, Fulcher T, Datta V & Acheson R: Pneumatic retinopexy versus scleral buckling: a randomized controlled trial. Ir J med Sci 1996;165:274-277.
27. Tornambe PE. Pneumatic retinopexy: the evolution of case selection and surgical technique: A twelve year study of 302 eyes. Trans Am Ophthalmol Soc 1997;95:551-78.
28. La Heij EC, Derhaag PF, Hendrikse F. Results of scleral buckling operations in primary rhegmatogenous retinal detachment. Doc Ophthalmol 2000;100(1):17-25.
29. Oshima Y, Yamanishi S, Sawa M, et al. Two-year follow up study comparing primary vitrectomy with scleral buckling for macula-off rhegmatogenous retinal detachment. Jpn J Ophthalmol 2000 Sep-Oct;44(5):538-49.
30. Sharma T, Challa JK, Ravishankar KV, et al. Scleral buckling for retinal detachment. Predictors for anatomic failure. Retina 1994;14(4):338-43.
31. Saw SM, Gazzard G, Wagle AM, et al. An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment. Acta Ophthalmol Scand 2006;84(5):606-12. Review.
32. Subramanian ML, Truong SN, Rogers AH, et al. Vitrectomy for stage 1 macular holes identified by optical coherence tomography. Ophthalmic Surg Lasers Imaging 2006;37(1):42-6.
33. Bensom WE, Cruickshanks KC, Fong DS, et al. Surgical Management of Macular Holes: A Report by the American Academy of Ophthalmology. Ophthalmology 2001;108:1328-1335.
34. Ho AC, Guyer DR, Fine SL. Major Review: Macular Hole. Survey of Ophthalmology 1998;42:393-416.
35. Jaycock PD, Bunce C, Xing W, et al. Outcomes of Macular Hole Surgery: Implications for Surgical Management and Clinical Governance. Eye 2005;19:879-884.
36. Kang HK, Chang AA, Beaumont PE. The macular hole: report of an Australian surgical series and meta analysis of the literature. Clin Experiment Ophthalmol 2000;28(4):298-308.
37. Wong JG, Sachdev N, Beaumont PE, et al. Visual outcomes following vitrectomy and peeling of epiretinal membrane. Clin Experiment Ophthalmol 2005;33(4):373-8.
38. Koizumi H, Spaide RF, Fisher YL, et al. Three-Dimensional Evaluation of Vitreomacular Traction and Epiretinal Membrane Using Spectral-Domain Optical Coherance Tomography. Am J Ophthal 2008;145:509-517.
39. Tari SR, Vidne-Hay O, Greenstein VC, et al. Functional and Structural Measurements for the Assessment of Internal Limiting Membrane Peeling in Idiopathic Macular Pucker. Retina 2007;27:567-572.
40. Sheard RM, Charanjit S, Gregor Z. Acute Macular Pucker. Ophthalmology 2003;110:1178-1184.
41. Grewing R, Mester U. Results of Surgery for Epiretinal Membranes and their Recurrences. Br J Ophthalmol 1996;80:323-326.
42. Wong JG, Sachdev N, Beaumont PE, et al. Visual outcomes following vitrectomy and peeling of epiretinal membrane. Clin Experiment Ophthalmol 2005;33(4):373-8. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in