|
|
 |
 |
 |
 |
|
|
Boston Keratoprosthesis in epithelial downgrowth
Digital Journal of Ophthalmology 2009
Volume 15, Number 1
January 1, 2009
DOI: 10.5693/djo.01.2009.001
|
Printer Friendly
|



Tarinee Sa-ngiampornpanit, MD | Ramathibodi Hospital, Bangkok, Thailand Sureka Thiagalingam, MBChB, MPH | Massachusetts Eye and Ear Infirmary, Boston, MA USA Claes H. Dohlman, MD, PhD | Massachusetts Eye and Ear Infirmary, Boston, MA USA
|
|
|
| Abstract | Introduction: To report a case of histologically proven epithelial downgrowth after multiple failed penetrating keratoplasties and glaucoma filtering surgeries that was successfully treated with Boston keratoprosthesis implantation.
Materials and Methods: A 61-year-old monocular patient had severe congenital ocular syphilis with secondary glaucoma. He had undergone many intraocular surgeries with a history of epithelial downgrowth, and he presented with a failed graft after 7 penetrating keratoplasties. Implantation of a corneal graft with an aphakic type of Boston keratoprosthesis was performed, combined with anterior vitrectomy. The main outcome measures were visual acuity, ocular inflammation and media clarity.
Results: Media clarity was restored and revealed severe retinal scarring and a pale optic nerve. Best corrected visual acuity of 20/400 was maintained without any further surgical intervention during 6 years follow up. No retroprosthesis membrane or epithelial growth behind the keratoprosthesis was observed.
Discussion: This is, to our knowledge, the first case of long-term successful treatment of epithelial downgrowth with a Boston keratoprosthesis. This approach might be considered a suitable treatment of epithelial downgrowth. | | | Introduction | Epithelial downgrowth is an uncommon but sight-threatening complication of intraocular surgery or penetrating eye injury.(1, 2) The incidence of this condition after aphakic penetrating keratoplasty (PK) has been estimated at 0.25%.(3) Clinically, it is recognized as a migratory line on the posterior surface of the cornea or as a membrane on the iris surface. It is often associated with elevated intraocular pressure (IOP) and corneal edema, resulting in poor vision.(3, 4)
Treatment of epithelial downgrowth has met with only rare success despite attempts with a variety of methods such as stripping the membrane, swabbing with alcohol, cryotherapy and wide surgical excision.(1, 5) Corneal transplantation has had a high failure rate.(6) Secondary glaucoma, corneal edema and recurrence after treatments have been the rule.
We herein describe a case of epithelial downgrowth treated with the Boston keratoprosthesis as a new alternative treatment for epithelial downgrowth to keep the media clear on a long-term basis. | | | Materials and Methods | Case Report:
A 61-year-old man was referred to the Cornea Service of the Massachusetts Eye and Ear Infirmary in August 2000 with a history of congenital syphilis, congenital deafness and congenital glaucoma. He had undergone multiple filtering surgeries and cyclo-cryotherapies for control of the IOP in both eyes. Finally his right eye was enucleated. The left eye had poor vision from corneal edema and graft failure since 1992. The eye had undergone a total of 5 PKs which often failed after 6-12 months postoperatively. Corneal epithelial downgrowth was first documented in the pathology report of the second transplant specimen in 1995. Best corrected visual acuity (BCVA) during the past 10 years had been 20/400 in his left eye (20/50 with telescopic lens). He also had a right cochlear implant for his congenital deafness.
On examination, the BCVA of his left eye was counting fingers at 5 feet (20/200 with telescopic lens) and the IOP was controlled. Because of this stable situation, we declined surgery and decided to continue observation. During this period he underwent 2 more PKs elsewhere, which again failed 6-12 months postoperatively.
The patient returned in March of 2002. At this examination, his left eye BCVA was counting fingers at 4 feet. His left cornea was edematous and cloudy consistent with graft failure (Figure 1). IOP was approximately 5 mmHg (finger palpation) on 0.2% dorzolamide hydrochloride-0.5% timolol maleate ophthalmic solution twice daily. This time we agreed to perform keratoprosthesis implantation following detailed discussion regarding the risks and benefits. A Boston keratoprosthesis (KPro Type I) in a fresh donor corneal graft was implanted using standard technique.(7) The diameter of the donor corneal button was 8.5 mm, and the eye was trephined to 8.0 mm; anterior vitrectomy was also performed. At the end of the operation, 400 micrograms of dexamethasone was injected into the anterior chamber. A soft contact lens of 16.0 mm diameter and 9.8 mm base curve (Kontur Kontact Lens Co., Inc., Richmond, CA) was applied. No intraocular membrane formation was identified during the surgery. Histopathology of the corneal button demonstrated thin epithelial layers on the endothelial side consistent with epithelial downgrowth (Figure 2). | |
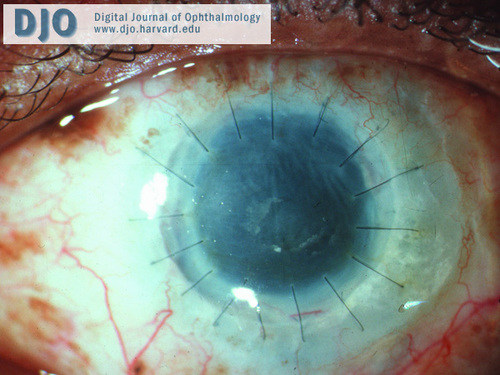
Figure 1
Preoperative appearance of left eye showing a cloudy, edematous left cornea with peripheral vascularization.
|
|
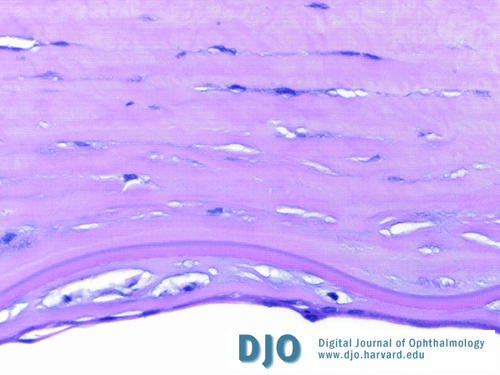
Figure 2
Pathologic specimen of the left corneal button demonstrates thin epithelial layers on the endothelial surface. (Hematoxylin-eosin, 40x). (Courtesy of TJ Dryja, M.D., Massachusetts Eye and Ear Infirmary, Boston, MA)
|
|
| Results | Postoperatively, the IOP was low (on no glaucoma medication) and the eye developed peripheral choroidal detachments, which gradually improved over 2 weeks. He also showed low-grade anterior chamber cells and flare, which required several subtenon injections of triamcinolone 40 mg during the first few months. The postoperative regimen included 1% prednisolone acetate, 0.3% ofloxacin, and vancomycin (14 mg/ml) drops, originally 4 times daily but gradually reduced to once per day. His vision improved to 20/400 after one month and has remained at that level since (Figure 3).
At the most recent visit, 6 years after the operation, his BCVA was maintained at the level of 20/400, with low IOP without any glaucoma medication and a stable cup-disc ratio of 0.85. The keratoprosthesis has remained in place without sign of inflammation or tissue melt (Figure 4). No retroprosthesis membrane or epithelial growth has been observed, but the optic nerve was markedly pale and there was severe retinal scarring, which had been noticed since the media clarity was restored. No further surgery was considered. | |

Figure 3
One month after the Boston keratoprosthesis implantation with contact lens in place. There was only mild conjunctival injection and a few cells and flare in anterior chamber. The visual acuity was 20/400.
|
|

Figure 4
At most recent follow up visit, 6 years after the surgery, the left eye was quiet and without signs of intraocular epithelium or retroprosthesis membrane formation. The visual acuity remained 20/400.
|
|
| Discussion | Epithelial downgrowth is a rare but usually devastating complication of multiple ocular surgeries.(1, 2) It can occur after intracapsular or extracapsular lens extraction complicated by improper wound healing. With advanced surgical techniques, it is presumably less frequent.(3, 8) It can also be observed in cases of traumatic, full thickness corneal wounds. PK has also resulted in epithelial downgrowth, as in the present case, and with a history of multiple surgeries the risk of developing this condition is increased.(3,4,5,9,10) Regardless of etiology, the epithelial cells slowly spread over the posterior corneal surface, trabecular structures and iris. For unknown reasons, further posterior spread is very rare.
Epithelial downgrowth can result in two serious complications: glaucoma and corneal edema. Both are very difficult to treat and have a high risk of recurrence after attempted treatment. The secondary glaucoma often requires placement of a glaucoma drainage device or diode cyclophotocoagulation, often with unsatisfactory results. Corneal edema resulting from epithelium interfering with the endothelial pump function is likewise very difficult to eradicate. Repeated PKs rarely lead to restoration of vision in the long term.(6, 10) The remaining peripheral epithelium usually re-invades the posterior graft surface, resulting in graft edema and failure, and likewise the trabecular structures can be further occluded.
Recently, radical surgery has had some success in isolated cases but especially in the localized disease such as segmental epithelial cyst, which overall has a better prognosis compared to the diffuse variant.(12-13) In contrast, a keratoprosthesis in a corneal carrier graft may be another, rather simple and effective alternative treatment for epithelial downgrowth. The Boston kerotoprostheis surgery is much less complicated and less destructive than some block dissection techniques.
In our case, there was no identifiable epithelial tissue or membrane on the posterior surface of the keratoprosthesis or on the vitreous surface, postoperatively. Two months after the surgery, there were no inflammatory cells visible in the anterior chamber, only some anterior chamber flare, undoubtedly the effect of multiple surgeries on the blood-aqueous barrier.
Our patient’s current visual acuity, although better than the preoperative vision, is still disappointing. The vast destruction of the retina as well as the pale optic nerve (not visible preoperatively) fully explain this level of vision. However, the media have remained very clear during the whole postoperative period and should have allowed a vision of 20/70-40 if the posterior segment had been normal. Three more cases with epithelial downgrowth have since been implanted with the Boston KPro with anatomically good results. These patients with shorter follow up will be described more fully in a future setting.
The clinical picture in this patient has shown remarkable stability with media clarity and absence of inflammation. This technique of essentially bypassing the cloudy cornea might be applicable in others cases of epithelial downgrowth as well, regardless of etiology. | | | Acknowledgements | Proprietary interest, financial disclosure:
None of the authors has financial interest in any of the products described in this manuscript. | | | References | 1. Maumenee AE, Paton D, Morse PH, et al. Review of 40 histologically proven cases of epithelial downgrowth following cataract extraction and suggested surgical management. Am J Ophthalmol 1970; 69:598–603.
2. Weiner MJ, Trentacoste J, Pon DM, et al. Epithelial downgrowth: A 30-year clinicopathological review. Br J Ophthalmol 1989; 73:6–11.
3. Sugar A, Meyer RF, and Hood CI. Epithelial downgrowth following penetrating keratoplasty in the aphake. Arch Ophthal 1977; 95:464–7.
4. Mazow ML and Stephens RW. An unusual complication after keratoplasty. Surv Ophthalmol 1966; 11:205-8.
5. Stark WJ, Michels RG, Maumenee AR, et al. Surgical management of epithelial downgrowth. Am J Ophthalmol 1978; 85:772–80.
6. Anseth A, Dohlman CH, and Albert DM. Epithelial downgrowth—fistula repair and keratoplasty. Refract Corneal Surg 1991; 7:23–7.
7. Dohlman CH and Nouri M. Keratoprosthesis surgery. In: Foster CS, Azar DT, Dohlman CH, eds. Smolin and Thoft’s The Cornea: Scientific Foundations and Clinical Practice. Philadelphia, PA: Lippincott Williams & Wilkins, 2004; 1085-1095.
8. Schaeffer AR, Nalbandian RM, Brigham DW, et al. Epithelial downgrowth following wound dehiscence after extracapsular cataract extraction and posterior chamber lens implantation: Surgical management. Cataract Refract Surg 1989; 15:437–441.
9. Feder RS and Krachmer JH. The diagnosis of epithelial downgrowth after keratoplasty. Am J Ophthalmol 1985; 99:697-703.
10. Leibowitz HM, Elliott JH, and Boruchoff SA. Epithelization of the anterior chamber following penetrating keratoplasty. Arch Ophthal 1967; 78:613-7.
11. Groh MJ and Naumann GO. Cystic epithelial growth after penetrating keratoplasty: Successful curative treatment by block excision. Br J Ophthalmol 2001; 85:240.
12. Daneshvar H, Brownstein S, Mintsioulis G, et al. Epithelial ingrowth following penetrating keratoplasty: A clinical, ultrasound biomicroscopic and histopathological correlation. Can J Ophthalmol 2000; 35:222-4.
13. Nagra PK and Raber IM. Epithelial ingrowth in a phakic corneal transplant patient after traumatic wound dehiscence. Cornea 2003; 22:184-6. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in