|
|
 |
 |
 |
 |
|
|
High myopia as a risk factor for post-LASIK ectasia: a case report
Digital Journal of Ophthalmology 2009
Volume 15, Number 1
February 23, 2009
|
Printer Friendly
Download PDF |



Mona Harissi-Dagher, MD | Massachusetts Eye and Ear Infirmary, Boston, MA, USA and Department of Ophthalmology, Universite de Montreal, Quebec, Canada Sonja A.F. Frimmel | Friedrich-Alexander-University Erlangen-Nuremberg, Germany Samir Melki, MD, PhD | Massachusetts Eye and Ear Infirmary, Boston, MA and Boston Eye Group, Boston, MA, USA
|
|
|
| Abstract | Purpose: To describe the case of a patient developing corneal ectasia following LASIK for the correction of myopic astigmatism.
Materials and Methods: A 39-year-old man underwent bilateral uneventful LASIK for myopic astigmatism of -10.25 -1.75 x040 OD and -8.00 -2.50 x005 OS. Preoperative corneal pachymetry was 542 micrometers OD and 543 micrometers OS. Preoperative corneal topography showed bilateral oblique bow-tie patterns. Central keratometry measurements were 45.12 D @ 124 / 43.87 D @ 34 OD and 44.87 D @ 78 / 43.12 D @ 168 OS. Keratoconus or forme fruste keratoconus were not present preoperatively.
Results: The residual stromal bed was 314 micrometers OD and 295 micrometers OS. Increasing astigmatism was documented progressively after LASIK. Central keratometry and topography were performed with evidence of ectasia OD at 17 months post-operatively and early evidence of ectasia OS at last follow-up of 58 months.
Conclusion: High myopia appears to be a predisposing factor in this patient. High myopia may need to be considered as an ectasia risk factor independent of amount of ablation or residual stromal bed thickness and in the absence of forme fruste keratoconus. The possibility remains that ectasia was due to an unidentified risk factor or an intrinsic corneal problem with this patient's right eye.
Keywords: LASIK, Ectasia, Forme Fruste Keratoconus, Myopia | | | Introduction | | Laser in situ keratomileusis (LASIK) is currently the most common refractive surgical procedure for the treatment of myopia. Its safety, effectiveness, and success have been widely reported.(1) With an increasing number of LASIK surgeries performed and with longer follow-ups, more complications are being observed. The incidence of serious complications is relatively low, but visual consequences can be dramatic considering the elective nature of this procedure.(1) Ectasia resulting from an unknown alteration in the biomechanical strength can lead to loss of best-corrected visual acuity and the need for a corneal transplant in severe cases. Seiler et al. described the first three cases of corneal ectasia after LASIK in 1998;(2) more cases have been reported since then. Herein, we describe a case of post-LASIK ectasia with high myopia as the identifiable risk factor. | | | Materials and Methods | Case report
A 39-year-old man of middle-eastern descent underwent refractive surgery for the correction of myopic astigmatism. Past ocular history was unremarkable. There was no history of contact lens wear. His uncorrected visual acuity (UCVA) was count fingers in both eyes. Best spectacle-corrected visual acuity (BSCVA) was 20/40 in both eyes with a refraction of –10.25 –1.75 x040 in the right eye (OD) and –8.00 –2.50 x005 in the left eye (OS). After instillation of Tropicamide 1% and Cyclopentolate 0.5%, the visual acuity (VA) was 20/30 OD and 20/25 OS with a refraction of –10.25 –1.50 x040 OD and –7.75 –3.25 x005 OS. Three measurements of corneal pachymetry were taken with Sonogage Pachymeter (Corneo-Gage Plus Cleveland, OH, USA), and the lowest measurement was recorded. Preoperative corneal pachymetry was 542 micrometers OD and 543 micrometers OS. Preoperative Humphrey Atlas Corneal Topography Systems (version A11.2, Carl Zeiss Inc.) showed bilateral oblique bow-tie patterns (Figure 1). No other topographers were available and hence posterior float and anterior float were not obtained. Central keratometry measurements were 45.12 D @ 124 / 43.87 D @ 34 OD and 44.87 D @ 78 / 43.12 D @ 168 OS. | |

Figure 1
Pre-operative corneal topography OD and OS showing bilateral oblique bow-tie patterns. A standard 0.5 D interval scale is used.
|
|
| Results | On June 21, 2002, uneventful LASIK was performed OS first followed by OD seven days later on June 28, 2002. There were no intraoperative complications. Excimer laser ablation was performed with a VISX Star S3 IR Excimer Laser System (VISX Technology, California) after a superiorly hinged flap was made with a Hansatome microkeratome (Bausch & Lomb, Rochester, NY) using a 9.5-mm suction ring. A 160 micron Hansatome head was used being that it provided the thinnest available cut at the time of surgery. Intraoperative pachymetry was performed after lifting the flap, taking 3 central measurements, and recording the lowest. The residual stromal bed was calculated by obtaining the lowest central pachymetry and deriving the ablation depth from the laser. In this patient, the targeted flap thickness of 160 micrometers resulted in a measured flap thickness of 124 micrometers OD and 153 micrometers OS, thinner than the corresponding settings on the microkeratome. Hence, the calculated residual stromal bed was 314 micrometers OD and 295 micrometers OS after an ablation of 103 micrometers OD and 95 micrometers OS. Laser ablation OD was performed with an M Ellipse (6.0 mm x 5.4 mm diameter, 80 micrometers depth) and an M Sphere (5.5 mm diameter, 23 micrometers depth). For OS, laser ablation was performed with an M Elllipse (6.5 mm x 5.3 mm diameter, 95 micrometers depth).
The patient achieved his best level of UCVA in the early post-operative period. UCVA was 20/40 OD eight days after LASIK and 20/50 OS two weeks after LASIK. BSCVA was 20/20 OD with –1.00-1.00x020 and 20/30 OS with -1.25-1.00x125 two weeks after the initial procedure OS.
Five months after LASIK, the UCVA decreased to 20/70 in both eyes. At that time the patient complained of blurred vision at distance and difficulty driving at night. No evidence of ectatic topography was found. The patient was followed and monitored for visual stability while entertaining the possibility of performing an enhancement.
The first evidence of ectasia was noted OD in September 2003, 17 months after the initial procedure. At that time, BSCVA was 20/40 OD with a manifest refraction of -6.50-4.00x060 and 20/30 OS with a manifest refraction of -1.50 –1.25 x122. His axial videokeratography map OD revealed an asymmetric bow-tie pattern with inferior steepening. The latter was also seen on the tangential map (Figure 2). In the second to third year after LASIK, the refractive error stabilized with BSCVA of 20/150 OD and 20/30 OS with –3.50 –3.25 x070 and –0.75 -3.75 x120, respectively, indicating progressing ectasia OU. At the end of the third year, corneal topography showed central to inferior steepening OD typical of ectasia and normal topography OS. At last follow-up of 58 months, BSCVA was 20/200 OD and 20/25 OS with -3.00 -4.50 x075 and -5.25 –3.75 x135, respectively. Central keratometry measured 52.37 D@ 132 / 50.50 D@42 OD and 44.25 D @38 / 39.50 D @128 OS (Table 1). Pachymetry was 463 micrometers OD and 471 micrometers OS. | |
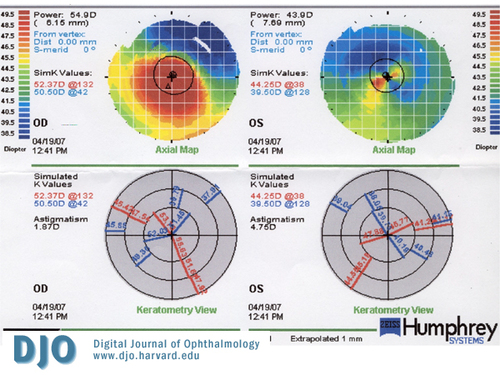
Figure 2
Corneal topography demonstrating severe inferior steepening OD and asymmetric bow tie OS with inferior steepening 58 months post-operatively. A standard 0.5 D interval scale is used.
|
|

Table 1
Keratometric Readings Pre-op and Post-LASIK OU.
|
|
| Discussion | Corneal ectasia is a known complication of LASIK that can lead to devastating visual consequences. It is defined as an acquired, non-inflammatory, biomechanical outward bulging of the cornea. It results in progressive thinning and central to inferior steepening of the cornea. This usually happens in the context of a myopic shift in refraction, increasing regular astigmatism, irregular astigmatism, and eventually loss of BCVA.
Proper preoperative evaluation and patient selection are essential to decrease the risk of ectasia. Certain preoperative risk factors for ectasia have been determined. These include high myopia,(2-9) high astigmatism, reduced preoperative corneal thickness, and low residual stromal bed. These have been reported in the majority of ectasia cases, but none of these characteristics alone definitively predicts the development of ectasia. In fact, ectasia can develop in eyes with low myopia and no currently identifiable risk factors.(10)
Documented diagnoses predisposing to corneal ectasia after excimer laser ablation are keratoconus, keratoconus suspect, or pellucid marginal degeneration. None of these conditions was present at the time of LASIK either by exam or by corneal topography. Our patient was 39 years old at the time of the surgery with a history of a stable refraction making the diagnosis of labile keratoconus extremely unlikely. LASIK retreatment may increase the risk of ectasia as it ablates more corneal tissue and thins the cornea further.
Ectasia developed in our patient without the presence of any of the three main predisposing factors: keratoconus or forme fruste keratoconus, LASIK retreatment or a thin residual bed. Although the patient has oblique and slightly asymmetric astigmatism, it does not meet the criteria for a keratoconus-suspect. The patient’s vision was not correctable to 20/20, but instead his BCVA was 20/40 OU. In retrospect, this may be an indication of forme fruste keratoconus; nevertheless, it is not unusual for high myopes not to correct to 20/20 vision as demonstrated by laser interference fringes.(11) The lack of anterior and posterior float does not allow us to rule out forme fruste keratoconus either, but imaging of the posterior surface was not a widespread modality at the time the patient was evaluated for LASIK. In summary, myopia seems to be the only identifiable factor, and this has already been reported as a risk factor for post-LASIK ectasia. This is not a new clinical finding, but rather a possible confirmatory case of the existing literature on the subject. It is not clear from previous reports (4) whether high myopia predisposes to ectasia because of the larger amount of tissue ablation or from other inherent factors.
In fact, risk factors related to preoperative and postoperative corneal thickness were not present in this case. Preoperative central corneal thickness was 542 micrometers OD and 543 micrometers OS, higher than the advocated 500 micrometers limit for LASIK.(10) Machat suggested a posterior stromal thickness of no less than 50 percent of the corneal thickness.(12) In our patient, posterior stromal thickness with respect to total corneal thickness was measured at 57.9 percent OD and 54.3 percent OS.
A residual stromal bed thickness of 250 micrometers has been advocated as a relatively safe limit for the prevention of corneal ectasia.(2,3) It appears that the forward shift of the cornea may be more marked with less than 250 micrometers. This is not a strong relationship however, and one should conclude from the literature that the 250 micrometers limit is not necessarily safe.
Unknowingly cutting thicker flaps may result in thinner residual stromal bed thickness than intended leading to ectasia erroneously attributed to other risk factors. Also, the thickness of the corneal flap may vary with the same microkeratome in the same surgeon’s hands.(13,14) The achieved flap in one reported case of ectasia was excessively thick leading to ectasia immediately after surgery despite avoidance of laser ablation.(15) In many other ectasia case reports, the corneal flap was much thicker than planned.(16) Other case reports lack intraoperative pachymetry measurements leaving a question around this important variable.(4) We advocate routinely measuring the intraoperative bed thickness to ensure adequate room for the laser ablation. In our patient, the targeted flap thickness of 160 micrometers resulted in a measured flap thickness of 124 micrometers OD and 153 micrometers OS, thinner than the corresponding settings on the microkeratome.
The residual stromal bed thickness is also directly related to the amount of corneal tissue removed. To minimize tissue removal, surgery on this patient was performed with a combined ablation zone diameter of 5.5/6 mm OD and 6.5 mm OS. Based on the Munnerlyn’s formula,(17) as the width of ablation increases, the thickness of the residual stromal bed decreases proportionately; thus, the risk of developing ectasia increases with wider ablations. In OD, 2 diopters were treated at a zone of 5.5 mm diameter thereby further minimizing tissue removal. This brought the amount of tissue removal OD (103 micrometers) quite close to OS (95 micrometers). The reduced laser ablation, in combination with a thinner corneal flap, resulted in a thicker residual stromal bed thickness in the ectatic OD (314 micrometers) compared to OS (295 micrometers).
It is possible that a safe residual stromal bed thickness is patient-dependent relative to other biomechanical properties of the cornea. It has been postulated that the posterior corneal stroma has less biomechanical strength than the anterior layers.(18) Lee et al. reported on the biomechanics of the cornea noting that there were no statistically significant changes in the post-surgical forward shift of the posterior corneal surface if the residual corneal thickness is more than 350 micrometers or if the ablation ratio per total cornea is less than 10 percent.(12) In our case, the ablation ratio was not significantly different between the two eyes. The measured ablation was 103 micrometers OD and 95 micrometers OS representing 19.2 percent OD and 17.5 percent OS ablation ratio per total cornea. These two figures are higher than the advocated 10 percent but are essentially similar in both eyes. Yet, OD suffered earlier and more severe ectatic changes than OS. In this case report, myopia is the only identifiable risk factor, but the possibility remains that ectasia was due to an unidentified risk factor or an intrinsic corneal problem with this patient's right eye.
Conclusion
In summary, post-LASIK ectasia OD was noted unilaterally initially even though other known intraoperative predisposing factors would have predicted a slightly higher ectasia risk for OS. The only predisposing factor OD was the higher level of preoperative myopia. It is possible that higher levels of myopia may be associated with different corneal biomechanical properties that predispose to ectasia. These inherent factors as well as a safe level of myopia remain to be elucidated in future studies. | | | Acknowledgements | Financial support: none
Proprietary interest: none | | | References | 1. Sugar A, Rapuano CJ, Culbertson WW, Huang D, Varley GA, Agapitos PJ, de Luise VP, Koch DD. Laser in situ keratomileusis for myopia and astigmatism: Safety and efficacy: A report by the American academy of ophthalmology. Ophthalmology. 2002; 109:175-187.
2. Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg. 1998;14:312-317.
3. Joo C, Kim T. Corneal ectasia detected after laser in situ keratomileusis for correction less than –12 diopters of myopia. J Cataract Refract Surg. 2002;26:292-295.
4. Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110:267-275.
5. Tabbara KF, Kotb AA. Risk factors for corneal ectasia after LASIK. Ophthalmology. 2006;113(9):1618-22.
6. Condon PI, O'Keefe M, Binder PS. Long-term results of laser in situ keratomileusis for high myopia: risk for ectasia. J Cataract Refract Surg. 2007;33(4):583-90.
7. Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008;115(1):37-50. Epub 2007 Jul 12.
8. Binder PS. Analysis of ectasia after laser in situ keratomileusis: risk factors. J Cataract Refract Surg. 2007;33(9):1530-8.
9. Caster AI, Friess DW, Potvin RJ. Absence of keratectasia after LASIK in eyes with preoperative central corneal thickness of 450 to 500 microns. J Refract Surg. 2007;23(8):782-8.
10. Amoils SP, Deist MB, Gous P, Amoils PM. Iatrogenic keratectasia after laser in situ keratomileusis for less than –4.0 to 7.0 diopters of myopia. J Cataract Refract Surg. 2000;26:967-977.
11. Coletta NJ, Watson T. Effect of myopia on visual acuity measured with laser interference fringes. Vision Res. 2006;46(5):636-51
12. Machat JJ. Eximer laser refractive surgery; practice and principles. Thorofare, NJ, Slack Inc, 1996;300.
13. Lee DH, Seo S, Jeong KW, Shin AC, Vukich JA. Early spatial changes in the posterior corneal surface after laser in situ keratomileusis. J Cataract Refract Surg. 2003;29:778-784.
14. Flanagan GF, Binder PS. The precision of flap measurements for laser in situ keratomileusis in 4428 eyes. J Refractive Surg. 2003;19:113-123
15. Haw WW, Manche EE. Iatrogenic keratectasia after a deep primary keratotomy during laser in situ keratomileusis. Am J Ophthalmol. 2001;132:920-921.
16. Tervo TM. Iatrogenic keratectasia after laser in situ keratomileusis [letter]. J Cataract Refract Surg. 2001;27:490-491.
17. Gatinel D, Hoang-Xuan T, Azar DT. Determination of corneal asphericity after myopia surgery with the excimer laser: a mathematical model. Invest Ophthalmol Vis Sci. 2001;42(8):1736-42.
18. Andreassen TT, Simonsen AH, Oxlund H. Biomechanical properties of keratoconus and normal corneas. Exp Eye Res. 1980;31:435-441. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in