|
|
 |
 |
 |
 |
|
|
The Boston Keratoprosthesis: A New Threadless Design
Digital Journal of Ophthalmology 2007
Volume 13, Number 3
September 5, 2007
|
Printer Friendly
|
|
|
|
|
| Abstract | Objective
To describe a new modification of the Boston Keratoprosthesis (KPro) which makes the assembly simpler and less traumatic.
Methods
The screw threads on the stem of the KPro and on the back plate have been removed and new dimensions have been introduced to the design.
Results
Twenty patients had the threadless KPro implanted and were followed from one to twelve months. No complications attributable to the new design occurred.
Conclusion
This threadless design should have the following advantages over the previous screwed-together device:
1. Assembly is easier for the surgeon.
2. The back plate is not causing shredding damage to the posterior graft membranes as can happen with the screw-on assembly.
3. It should be possible to manufacture this threadless device by molding rather than by machining, which should radically decrease production cost.
Keywords
Boston Keratoprosthesis; Threadless Device | | | Introduction | In cases of severe corneal opacity, a standard penetrating keratoplasty (PK) may not succeed and in such event a keratoprosthesis (KPro) (“artificial cornea”) may have to be resorted to. For history and various types of KPros, see the recent review by Khan et al.(1) The Boston Type I KPro is designed like a collar button with a front plate, a stem, and a back plate. It is manufactured from medical-grade polymethylmethacrylate (PMMA). During surgery it is usually incorporated into a corneal transplant, which is then sutured into the patient’s cornea in standard manner.(2)
The device comes in three parts: the front plate with the stem, the back plate, and a locking ring. For 18 years, the stem and the back plate have been machined with threads so that the plate can be firmly screwed onto the stem. Since 2003, a locking ring that can be snapped into a groove on the stem behind the back plate, has been added to prevent possible unscrewing of the plate in vivo.(2)
More recently concerns have been raised about this threading technique. In the process of assembly, the posterior surface layers of the corneal graft might become shredded in a detrimental way by the rotation of the back plate. In addition, the screwing technique can be difficult for the inexperienced surgeon. Finally, the presence of screw threads makes inexpensive manufacturing of the device by molding impossible. For these reasons a threadless design has been developed and tested clinically. This device is described here.
| | | Materials and Methods | The Threadless KPro
The front part, shown in figure 1, consists of a front plate with a diameter of 5.0 mm or 6.0 mm. The front surface is machined and polished to give the desired dioptric power (see below). The stem has several segments. The segment closest to the front plate has a diameter of 3.35 mm. and a height of 0.62 mm. It is made to accommodate the corneal graft (fig 2). The next segment is matched for the back plate central hole and the diameter is 3.0 mm. Its height is 0.84 mm. It has no screw threads but the fit between stem and plate is fairly snug. Just behind the back plate area is a groove for the locking ring to snap into. The groove has a diameter of 2.74 mm at the bottom and a height of 0.33 mm. The locking ring is made of medical grade titanium and it has a radial cut to facilitate snapping it into place. The ring outer diameter is 3.6 mm, inner diameter 2.8 mm and its thickness is 0.23 mm. Finally, there is a short, slightly beveled lead stem of slightly varying height to facilitate pushing the locking ring onto the stem. The total antero-posterior height of the assembled device is about 3.0 mm, depending on the steepness of the curvature of the anterior surface.
The back plate is substantially larger than the front plate, thus 8.5 mm in diameter. The central hole is 3.0 mm. The plate thickness next to the hole is 0.8 mm and at the periphery 0.6 mm. There are 16 holes of 1.17 mm diameter. The holes are necessary to allow aqueous access to the overlying cornea for nutrition.(3) The combined surface area of the holes is about 18 square millimeters. Another smaller back plate is also available and is useful in small children. It has a diameter of 7.0 mm, with 8 holes of 1.3 mm diameter each. The medical grade PMMA is purchased from Spartech Townsend, Pleasant Hill, Iowa. The machining of blanks for the two components of the KPro is performed similar to the previously described method4, now using a computerized lathe (Hardinge CHNC).
The front part is further processed as follows: The flat back surface of the stem is polished using ALOX 721 polishing compound. The anterior surface is next machined to the required radius. Subsequently, the part is placed into a polishing machine, using a lap and the ALOX compound. The back plate is fully made in the Hardinge lathe, and only requires deburring, inspection, and crack testing.
Evaluation of Optics
The KPros are manufactured to match the refractive need of the individual patient and, therefore, a substantial inventory is required to rapidly supply a device of the desired dimensions. Thus, for the eye that is pseudophakic and, therefore, approximately emmetropic, and where the IOL is left in place at surgery, a single standard power is chosen for the manufacture (see below). For aphakic eyes of different axial lengths, however, devices with varying degrees of power are made to allow a match to the patient’s needs as closely as possible. Thus, the axial length of the individual aphakic patient is always requested from the surgeon to allow the choice of a KPro that theoretically matches the dioptric requirement of the eye to be operated.
The optical power of every KPro is determined in the machine shop at the end of manufacturing by using a microscope base mounted on an optical bench.(4) The KPro is held in a diaphragm in front of the microscope and an illuminated Air Force bar chart is placed 10 feet away. The observer looks through the microscope at both KPro surfaces for quality evaluation. For measurement of focal length, the back surface of the KPro is first brought into focus. The microscope is then slid backwards until the details on the chart become clear. If the specified target on the chart can be seen sharply without distortions, the device is optically approved. Next, the distance between the two positions of the microscope, read on a millimeter scale, represents the back focal length (BFL) in air. These values normally run from 11 mm to 18 mm.
The conversion of the BFL in air to a recommended axial length value of the aphakic eye was originally calculated theoretically. However, the table had to be adjusted empirically based on past outcomes in terms of refraction and need for plus or minus correction. The present conversion table represents the best clinical fit. An inventory of the Boston KPro that can accommodate requests for patient eyes with axial lengths between 15 mm and 30 mm is sufficient. The power of the anterior curve of a KPro made for an eye with 23 mm axial length is approximately 60 diopters. For the emmetropic pseudophakic eye, a BFL in air of about 20 mm is recommended, and it varies little. The anterior surface power for the pseudophakic KPro is about 43-44 diopters.
Assembly
In the operating room, the technique of assembling the threadless KPro into a corneal graft varies from that of the previous, threaded type only in the placement of the back plate. Whereas the plate was, in the past, rotated 2.5 revolutions onto the stem and locked with a small spanner wrench, the present arrangement allows the plate simply to be placed gently on the stem, followed by pushing the locking ring into the groove. In short, the steps for assembly presently are as follows:
1. A corneal graft (usually 8.5 mm in diameter) is prepared, and a central 3.0 mm hole is trephined with a dermatological punch (AcuPunch, Acuderm Inc., Ft. Lauderdale, FL). Alternatively, the patient’s own cornea can be used.
2. For stability, the front part of the KPro is placed upside down on a patch of adhesive, which accompanies the device.
3. The graft with the central hole is slid over the KPro stem. An accompanying small pin, hollowed in one end, can be used to gently push the graft down to the front plate.
4. Viscoelastics are applied to the posterior surface of the graft.
5. The back plate is placed on the stem without any rotating movement.
6. The locking ring is pressed onto the lead stem with a finger. The hollowed pin is used to press the ring firmly down into the groove, usually with an audible snap. The assembly is inspected for correct position of the ring (Fig 2, 3).
7. The graft-prosthesis combination is removed from the adhesive and stored in the eye bank solution while the patient’s eye is prepared.
8. A trephine with 0.5 mm smaller diameter than the prepared graft (usually 8.0 mm) is used for the patient’s cornea. Any required cataract extraction, vitrectomy, iris manipulation, etc, are performed before the graft-prosthesis combination is transferred to the corneal opening and sutured in place. Present preference is to use twelve 9-0 nylon sutures, knots buried.
9. Finally, a soft contact lens, usually a Kontur lens (Kontur Kontact Lens Co., Hercules, CA), 16.0 mm diameter and 9.8 mm curve, plano, is placed on the eye as the last step of the operation.
The effect of threaded back plate on the posterior layers of the graft
Based on past clinical observation, there has been the suspicion that by screwing a threaded back plate onto the stem, there could be a shredding effect on the endothelium and Descemet’s membrane with adverse consequences within the back plate holes. A non-threaded plate, simply placed on the stem without rotation, might avoid such damage. A small experiment has confirmed this suspicion. Two eye bank corneas have had a standard, threaded Boston KPro implanted and examined afterwards. Rotation of the back plate was done in the usual way, avoiding excessive force. The corneas were afterwards grossly inspected, stained with fluorescein and subjected to standard embedding, cutting and H & E staining. It immediately became obvious that the back plate rotation had caused extensive damage to the posterior graft layers (Fig 4 ). Descemet’s membrane with the endothelium was shredded into scrolls, with the stroma exposed. The damage was extensive. | |
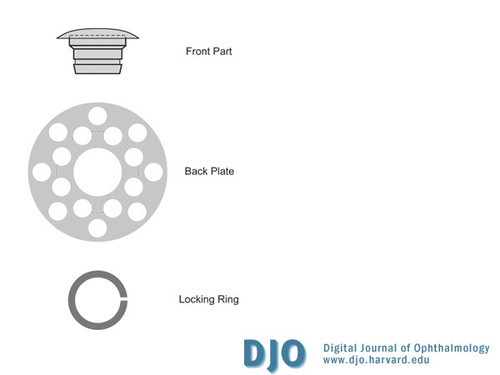
Figure 1
New design of the Boston Keratoprosthesis. Screw threads have been eliminated and dimensions have been changed.
|
|
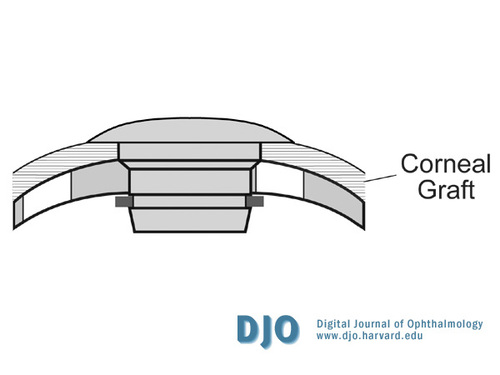
Figure 2
Diagram of the assembled device. The KPro has been incorporated into a corneal graft.
|
|
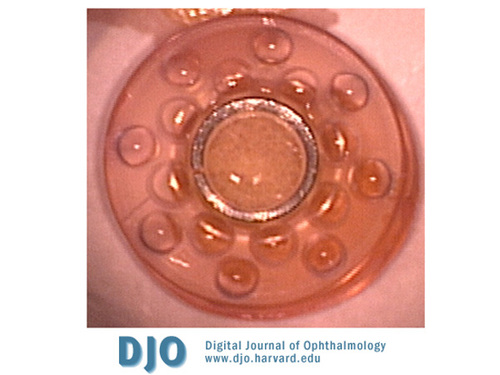
Figure 3
The assembled graft-prosthesis combination seen from the posterior side. The locking ring of titanium prevents the back plate from loosening.
|
|
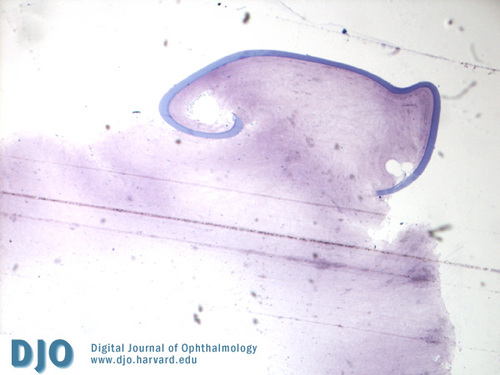
Figure 4
Result of assembly with the previous, threaded device. Descemet’s membrane and endothelium of the graft have been shredded by the screwed-on back plate.
|
|
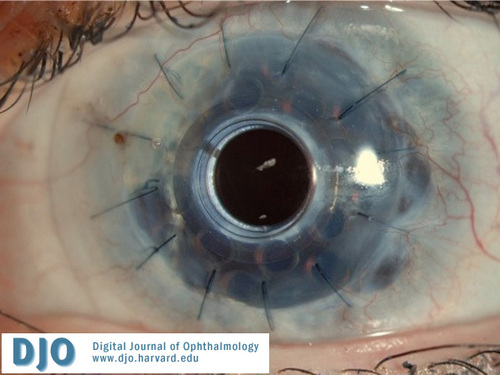
Figure 5
An eye with the threadless device used in a patient who had suffered a chemical burn at 9 months follow-up. Note lack of opacity in the holes.
|
|
| Results | Preliminary Clinical Experience
It is not the intention here to give a detailed description of the patients who have received the new threadless device. The purpose of cautiously introducing this modification under close surveillance has been to try to detect any adverse consequence attributable to the lack of threads.
The new threadless KPro design, labeled the “SO” series, has been used in 20 patients who have been followed for 1-12 months. 17 of the patients had previous graft failures in non-autoimmune disease, 1 patient had a chemical burn and 2 had a presumed autoimmune condition (Stevens - Johnson syndrome), the latter normally having a very guarded prognosis. No complication has occurred that could be attributable to the design. No infection has happened. A retroprosthesis membrane requiring opening with YAG laser formed in only 3 eyes (one with SJS, one after pseudomonas keratitis and one after severe herpes simplex keratitis). In general, the posterior surface of the graft areas within the back plate holes which previously often looked grey from scarring, now appear more clear and non-scarred (Fig 5).
| | | Discussion | Assembly of the Boston KPro with the threaded system has never been technically difficult. On occasion, however, surgeons have complained that they have mis-threaded the back plate and it has gotten stuck – without adverse clinical consequences, however. Also, recent examinations with high-definition OCT has revealed that not all threaded back plates have been rotated to completion.(Garcia JP Jr, de la Cruz J, Rosen RB, Buxton DF. Imaging implanted keratoprostheses with anterior segment OCT and UBM. 2007 ARVO poster #3868.) The consequence has been a space that is too wide for the corneal graft which has not swelled sufficiently to completely occupy the space. This has resulted in the front plate not lying flat on the graft surface but extruding forwards. Such configuration can result in exposure and tissue melt if the contact lens should become lost. Such assembly difficulties should be avoided with the new threadless design. As long as the locking ring has snapped into the groove, as has been done in 100% of the cases since its introduction 4 years ago, the position of the graft tissue should be as planned. The frequent damage to the endothelium and Descemet’s membrane with the threaded device has the potential of causing substantial long-term problems to the outcome. It is quite possible that the absence of limiting barriers in the holes of the back plate can allow steady access of allogeneic proteins and various injurious cytokines into the eye. This could explain examples of long-lasting intraocular inflammation, sudden sterile vitritis, cystoid macular edema, etc. It is also conceivable that keratocytes, converting to myofibroblasts, can escape backwards and be a cause of troublesome retroprosthesis membranes. Whether the new system of simply placing the back plate on the cornea, without rotating movement is gentler in the long run, cannot yet be stated with certainty but initial impressions are certainly very encouraging. It is possible, indeed likely, that there has been less intraocular inflammation postoperatively than with the previous design.
The third advantage of conversion to a threadless design should be the possibility of manufacturing the device by molding rather than by more expensive machining and polishing. Constructing a steel mold for a PMMA KPro with threads is considered extremely difficult and, therefore, expensive. A threadless device can be easily molded, opening the door to cheap KPro production that in turn could mean much greater use in developing countries. These countries have the highest incidence of corneal infectious ulcers and trauma, and they could benefit from lower the cost of manufacturing. Still, the lack of ophthalmologists, expense of patient travel, cost of antibiotics and contact lenses, and lack of education are formidable barriers to universal access, but a low cost of the KPro would certainly be of helpful. | | | References | 1. Khan BF, Harissi-Dagher M, Dohlman CH. Keratoprosthesis. In Albert & Jakobiec: Principles and Practice of Ophthalmology, 4th ed. (Eds Albert DM, Miller JW, Azar DT) Philadelphia, Saunders, in press.
2. Dohlman CH, Harissi-Dagher M, Khan BF, et al. Expert Review of Ophthalmology 2006;1(1):41-48.
3. Harissi-Dagher M, Khan BF, Schaumberg DA, Dohlman CH. Importance of nutrition to corneal grafts when used as a carrier of the Boston Keratoprosthesis. Cornea 2007 Jun;26(5):564-8.
4. Doane MG, Dohlman CH, Bearse G. Fabrication of a keratoprosthesis. Cornea 1996 Mar;15(2):179-84.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in