|
|
 |
 |
 |
 |
|
|
Spontaneous Crystalline Lens Dislocation in Vogt-Koyanagi-Harada Disease
Digital Journal of Ophthalmology 2007
Volume 13, Number 4
November 15, 2007
|
Printer Friendly
|


 Gareth Lewis
Gareth Lewis | Southampton Eye Unit Parwez Hossain | Southampton Eye Unit
|
|
|
| Abstract | Objective
To describe an uncommon case of spontaneous anterior crystalline lens dislocation in a man with Vogt-Koyanagi-Harada disease (VKH).
Methods
Observational case report.
Results
A 48 year old man with Vogt-Koyanagi-Harada disease presented to our eye department with a spontaneous anterior crystalline lens dislocation. He had lenticulo-corneal touch with corneal edema and was treated with an urgent lensectomy and anterior vitrectomy to reduce secondary corneal endothelium damage.
Conclusion
To the authors knowledge this is the first reported case of anterior crystalline lens dislocation in a patient with Vogt-Koyanagi-Harada disease.
Keywords
Lens, Dislocation, Uveitis, Vogt-Koyanagi-Harada | | | Introduction | VKH disease is a granulomatous inflammatory disorder affecting the eyes, auditory system, meninges and skin.(1) Early ocular manifestations include diffuse choroiditis, and exudative detachment of the retina. Late manifestations are not specific, with the possible exception of focal pale choroidal pigmentation (the “sunset glow fundus”) and Sugiura sign (perilimbal vitiligo). Other late ocular signs include nummular chorio-retinal depigmented scars, retinal pigment epithelium clumping and recurrent or chronic anterior uveitis.(1)
We report a unique case of a patient with VKH disease developing a spontaneous anterior lens dislocation illustrating how lensectomy can avoid subsequent potential complications. To our knowledge this is the first reported case of spontaneous lens dislocation in a patient with VKH disease. | | | Materials and Methods | | Report of a case. | | | Results | In April 2006, a 48 year old Caucasian man from the United Kingdom presented to Southampton Eye Unit with a 1 week history of left ocular discomfort. On examination, corneal decompensation was noted in the left eye with overlying epithelial loss secondary to an anteriorly dislocated crystalline lens (Figure 1). The crystalline lens was located in the anterior chamber and there was corneo-lenticular touch. There was no history of trauma and the intraocular pressure was not elevated.
The visual acuity in the left eye was unchanged at no perception of light after an episode of lymphocytic meningitis, exudative retinal detachment and central retinal artery occlusion 7 years previously for which he was treated at a different ophthalmic center.
A diagnosis of VKH disease was made on the basis of his history of meningism and exudative detachment followed several years later by left sensorineural deafness and recurrent left anterior uveitis with retinal vasculitis. In addition he had recently developed left poliosis and vitiligo.
At the time of initial presentation the patient’s neurological findings included recurrent headaches followed, in 1996, by an episode of lymphocytic meningitis. Other disease entities such as sacroidosis, tuberculosis, and Lyme disease were excluded with blood tests at the time. In addition an optic nerve biopsy was performed and excluded lymphoma and sarcoidosis. Histology confirmed that the central retinal artery lumen was occluded by an atheromatous plaque. He had discontinued steroid immuno-suppressive therapy 6 years previously as his left eye was considered to be blind and was painless.
He was admitted and treated with intensive topical antibiotics and steroids followed by urgent lensectomy and anterior vitrectomy. Viscoelastic material (Provisc) was injected between the cornea and the lens using the soft-shell technique to separate the lens from the cornea. The lens was then extracted through a large, superior clear corneal incision. No zonules were attached to the lens. An anterior vitrectomy was performed and the pupil was constricted with intracameral miochol. Figure 2 shows the patient at 8 weeks post-operatively.
| |
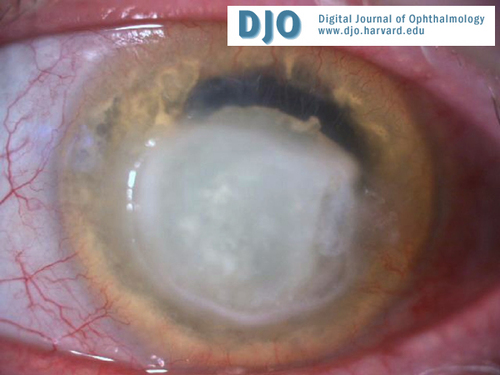
Figure 1
Left corneal decompensation and overlying epithelial loss secondary to an anteriorly dislocated crystalline lens + poliosis.
|
|

Figure 2
Eight weeks post operatively
|
|
| Discussion | To our knowledge this is the first reported case of spontaneous lens dislocation in a patient with VKH. Our patient had no history of ocular trauma or family history of lens dislocation. There have been several cases of spontaneous anterior lens dislocation in the literature (2, 3, 4) but this is the first case described associated with chronic intraocular inflammation. It is possible that previous severe chronic anterior uveitis may have caused zonular weakness predisposing our patient to this condition.
In the current literature the etiology of anterior crystalline lens dislocation includes spontaneous, traumatic, and heredity causes.(2) Traumatic dislocation accounts for slightly more than 50% of cases. Hereditary forms of lens dislocation can be associated with other systemic anomalies (eg, Marfan’s syndrome, homocystinuria, Weill-Marchesani syndrome).(2, 3, 4)
An anteriorly dislocated crystalline lens should always be removed.(5) Corneal edema, acute glaucoma and uveitis are frequently encountered complications. In our case corneal edema secondary to contact between the dislocated lens and the corneal endothelium was so severe, it had caused overlying epithelial loss, (Figure 1). Acute glaucoma can occur from a pupillary block mechanism, when the pupil margin is pressed down by the anteriorly dislocated lens.(3) This did not occur with our patient.
Vogt-Koyanagi syndrome is characterised by skin changes and anterior uveitis and the addition of Harada disease is given when there are neurological features and the possible occurrence of exudative retinal detachments.(6) VKH disease is a chronic granulomatous inflammatory disorder whose exact etiology remains unknown. The most commonly suggested immunologic basis involves autoimmune T cell activity against an unknown melanocytic antigen, a tyrosinase or tyrosinase-related protein.(7, 8)
New diagnostic criteria have been suggested based on the concept that VKH disease is a single entity with very different clinical manifestations depending on the stage at which the patient is examined.(1) In our patient, the initial neurological and ocular manifestations of meningism and exudative retinal detachment were followed years later by recurrent anterior uveitis, alopecia, poliosis and vitiligo. There was no clinical or laboratory evidence suggestive of other ocular disease entities such as sarcodosis, sympathetic ophthalmia, syphilitic uveitis, tuberculosis uveitis, Lyme disease, posterior scleritis, intraocular lymphoma, central serous choriodopathy or uveal effusion syndrome.
This unique case of a patient developing a spontaneous anterior lens dislocation alerts clinicians to this entity. To our knowledge this is the first reported case of spontaneous lens dislocation in a patient with VKH disease. | | | References | 1. Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, Arellanes-Garcia L, Pivetti-Pezzi P, Tessler HH, Usui M. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. Am J Ophthalmol. 2001 May;131(5):647-52.
2. Choi DY, Kim JG, Song BJ. Surgical management of crystalline lens dislocation into the anterior chamber with corneal touch and secondary glaucoma. J Cataract Refract Surg. 2004 Mar;30(3):718-21.
3. Peter NM, Nath R, Tranos PG, Teimory M. Bilateral lens subluxation associated with atopic eczema. Eur J Ophthalmol. 2005 May-Jun;15(3):409-11.
4. Lam A, Seck CM, Faye M, Brassier PK, Cisse MB, Diagne M. Spontaneous and bilateral anterior luxation of the lens in a 5-year-old child. J Fr Ophtalmol. 1996;19(4):279-82.
5. Jaffe NS, Jaffe MS, Jaffe GF. Cataract Surgery and Its Complications, 6th Ed. St Louis, MO: Mosby-Year Book, 1997; Chap. 8.
6. Kanski J. Clinical Ophthalmology, 5th Ed. Butterworth-Heinemann, 2003; Chap. 20.
7. Yamaki K, Gocho K, Hayakawa K, Kondo I, Sakuragi S. Tyrosinase family proteins are antigens specific to Vogt-Koyanagi-Harada disease. J Immunol. 2000 Dec 15;165(12):7323-9.
8. Gocho K, Kondo I, Yamaki K. Identification of autoreactive T cells in Vogt-Koyanagi-Harada disease. Invest Ophthalmol Vis Sci. 2001 Aug;42(9):2004-9.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in