|
|
 |
 |
 |
 |
|
|
Diagnosis and treatment of penetrating orbital cranial foreign body injuries
Digital Journal of Ophthalmology 2013
Volume 18, Number 4
December 31, 2012
DOI: 10.5693/djo.04.2012.06.001
|
Printer Friendly
Download PDF
|
|
|
Penetrating transorbitocranial injuries can occur in a variety of circumstances, and heightened suspicion is required to identify the foreign body, particularly in the setting of a trivial external wound. In “5-year-old girl with left upper eyelid swelling,” Shoeb and colleagues draw attention to an infrequent but important and potentially life-threatening injury.(1) A multidisciplinary team approach is mandated to provide expedient yet cautious and safe treatment. In the reported case, an ocular motility deficit and palpable foreign object led to appropriate neuroimaging with computed tomography (CT) and identification of the object. This is, however, infrequently the case; in the review of 23 wooden intraorbital foreign body injuries cited in the current report, the foreign object was identified by the radiologist on initial imaging in only 61% of cases.(2) Five cases were read as “possible foreign body” and 3 were read definitively as “no foreign body.” Thus the clinician caring for the patient should maintain a high index of suspicion and is best positioned to review the imaging obtained and to consider secondary studies, such as magnetic resonance (MR) and vascular imaging. This will facilitate prompt identification and treatment of a retained foreign body, preventing delay in diagnosis and subsequent sequelae, such as infection, hemorrhage, or death.
The bony orbit has a cone-like shape that literally funnels objects to the orbital apex, where the superior orbital fissure or optic canal may grant a penetrating object direct access to the intracranial cavity, particularly the area of the cavernous sinus and internal carotid artery. There should always be heightened awareness of the potential of life-threatening intracranial vascular injury. Examples from our personal experience follow. First, a young child presented with a trivial eyelid laceration; neuroimaging was interpreted as “air” in the orbit, and the treating physician in the emergency ward repaired the laceration. The following day, the child was referred to our Oculoplastic Surgical service with orbital cellulitis, somnolence, visual acuity of no light perception, and total ophthalmoplegia of the affected eye. Review of the previous neuroimaging revealed a linear foreign object extending from the orbital apex, through the superior orbital fissure, and to the region of the cavernous sinus (Figure 1). Because there was concern for possible vascular injury, a cerebrovascular neurosurgeon was consulted and CT angiography performed. A temporary endovascular balloon catheter was then placed into the left cavernous internal carotid artery (ICA) as a precautionary measure to control bleeding in the event of intraoperative hemorrhage (Figure 2). The foreign object (2.5 cm piece of wood) was removed via a transcranial orbitotomy. The child survived, but the eye remained without vision or movement.
With recent improvement in noninvasive vascular imaging with CT angiography and multiplanar bony reconstructions, significant vascular injury can also be excluded with a high degree of sensitivity. As a companion example, a 21-year-old man who was running down a hallway with a pen in his hand ran into a wall, impaling his right orbit. CT revealed an intact right globe, transgression of the right lamina papyracea and penetration of the left sphenoid sinus, with the pen tip along the expected course of the left cavernous ICA (Figure 3A). Multiplanar reconstructions and adjustment of the window width and level of the CT angiogram (Figure 3B) revealed that the “clicker” of the pen was not engaged meaning that the metallic tip lay within the plastic housing of the pen tip, and that the pen tip lay within the sphenoid sinus without penetration of the bony wall (white arrow). No carotid injury was evident. The pen was uneventfully removed via an anterior approach by the treating ophthalmologist. Only a mucosal abrasion on the wall of the intact sphenoid sinus was evident on endoscopic evaluation.
In the present case, the authors reported successful removal of a large foreign body that deeply penetrated from the anterior orbit well into the area of the brainstem. The case was managed by neurosurgery, which is essential when the intracranial compartment is breached. Definitive treatment plans are based on surgeon experience and preference, and the present case is an excellent vehicle to reiterate the importance of a multidisciplinary team approach combined with comprehensive neuroimaging in cases of suspected penetrating transorbital injuries.
There is a theoretical risk of brisk hemorrhage and death if a penetrating foreign body that surreptitiously tamponades a lacerated intracranial vessel is extracted from an anterior approach without proper preoperative preparation to stop or avoid hemorrhage. Notably, a review of the literature does not readily yield examples of such cases, possibly because surgeons are unlikely to publicly report such fatal errors. Lay people who quickly insert and then, on their own, remove sharp objects that have penetrated the orbit and intracranial vessels are not immune to reporting, as two such cases reported by Carothers in 1978 demonstrate.(3) The first case was a 25-year-old male who was stabbed below the right eye with an umbrella in a New York City bar. The wound was an “innocuous-appearing puncture in the lower lid, [and] was barely discernible.” Thirty minutes after injury, the patient developed focal seizure activity that progressed to hemiparesis. Neuroimaging showed an avulsed bone-spicule near the internal carotid artery. The patient regained motor function and was discharged from the hospital after ten days of inpatient care. He was lost to follow-up, until ten weeks later when, “during sexual intercourse,” the patient experienced headache, nausea, and vomiting. Angiography demonstrated a large, traumatic, internal carotid aneurysm. He died of a re-rupture of the aneurysm the night prior to surgery. The second case was of an off-duty police officer who, in a quarrel with a taxicab driver, was struck in the upper left eyelid by the tip of an umbrella. The injury was thought to be minimal, and the officer’s friends drove him home, where he collapsed and died of a cerebral hemorrhage.
Clues to a potential intracranial vascular injury include trajectory of the object near or past the course of known vessels or the cavernous sinus, intracranial hematoma, or fractures of the greater wing of the sphenoid.(4) In these cases, CT angiography or MR angiography should be obtained, along with catheter-based cerebral angiography if more detailed information is needed. Apart from assessing for local vascular injury, the circle of Willis collaterals can be assessed to gauge the risk of neurological morbidity or mortality should the affected artery require surgical ligation or endovascular occlusion. It is reasonable to remove penetrating transorbitocranial foreign bodies anteriorly if there is no evidence of vascular compromise and if the neurosurgeon advocates for anterior orbital rather than transcranial surgery. In cases in which vascular injury is suspected, a craniotomy may be preferable along with additional measures for hemostatic control, such as prepping and draping the neck for potential rapid access to the proximal carotid arteries(5) or the use of temporary balloon occlusion of the internal carotid artery.(6) Repeat imaging (post-procedure) can be useful to demonstrate the absence or stability of any intracranial hematoma;(7) repeat delayed vascular imaging is also important in cases where there is high suspicion of vascular injury, as traumatic pseudoaneurysms can occur weeks to months later.(8)
In conclusion, although periorbital trauma may appear trivial externally, ophthalmic findings of decreased vision, decreased motility, or of any neurological derangement should raise suspicion for more serious injury. In such cases, particularly in children (who may resist revealing the details of the injury), the possibility of a retained foreign body must also be considered. Initial neuroimaging in the form of CT should be carefully reviewed, and concern for a retained foreign body should also be communicated directly to the radiologist, preferably a neuroradiologist. The treating clinician should directly review all imaging studies and not simply rely on written reports. Wooden foreign bodies typically appear as aerated structures and widening of window width and level on CT scans can be helpful in revealing a linear course and overall geometric structure that is highly suspicious for a clinically occult wooden foreign body. If there is any concern for intracranial injury, neurosurgery should be consulted. Special studies, such as CT angiography or formal digital subtraction cerebral angiography, may be warranted to further assess vascular integrity. The foreign body should be extracted as safely as possible, either via anterior orbitotomy or craniotomy taking into account adjunctive measures that may be required to prevent or emergently control potentially life threatening hemorrhage.
References
1. Shoeb Ahmad S, Ghani SA, Peng KS, Sellamuthu P. 5-year-old girl with left upper eyelid swelling. Digital J Ophthalmol 2012;18. December 31, 2012.
2. Shelsta HN, Bilyk JR, Rubin PAD, Penne RB, Carrasco JR. Wooden Intraorbital foreign body injuries: clinical characteristics and outcomes of 23 patients. Ophthal Plast Reconstr Surg 2010;26:238-44.
3. Carothers A. Orbitofacial wounds and cerebral artery injuries caused by umbrella tips. JAMA 1978;239:1151-2.
4. Schreckinger M, Orringer D, Thompson BG, La Marca F, Sagher O. Transorbital penetrating injury: case series, review of the literature, and proposed management algorithm. J. Neurosurg 2011;114:53-61.
5. Dunn IF, Kim DH, Rubin PA, Blinder R, Gates J, Golby AJ. Orbitocranial wooden foreign body: a pre-, intra-, and postoperative chronicle: case report. Neurosurgery 2009;65:E383-4; discussion E384.
6. Cunningham EJ, Albani B, Masaryk TJ, Rasmussen PA. Temporary balloon occlusion of the cavernous carotid artery for removal of an orbital and intracranial foreign body: case report. Neurosurgery 2004;55:1225.
7. Fezza J, Wesley R. The importance of CT scans in planning the removal of orbital-frontal lobe foreign bodies. Ophthal Plast Reconstr Surg 1999;15:366-8.
8. Hern JD, Coley SC, Hollis LJ, Jayaraj SM. Delayed massive epistaxis due to traumatic intracavernous carotid artery pseudoaneurysm. J Laryngol Otol 1998;112:396-8.
|
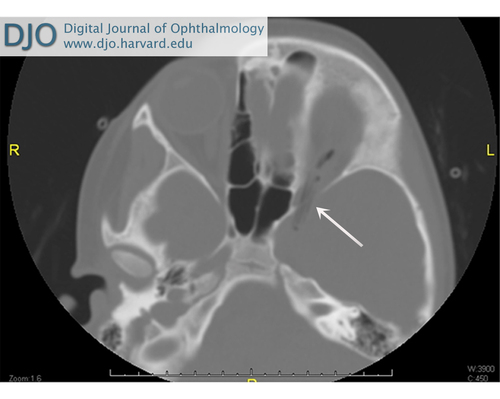
Figure 1
Axial computed tomography (CT) of the orbits (bone windows) of a child presenting with eyelid laceration. Wide bone windows (4000H width/40H level) are useful to distinguish wood from air and fat and to define a linear course or geometric structure suspicious for foreign objects. The wooden object in this case traverses the left superior orbital fissure to the region of the cavernous sinus.
|
|

Figure 2
Lateral digital subtraction angiography image. A balloon-catheter has been temporarily inflated within the left cavernous ICA. Endovascular techniques are useful to control intra-operative hemorrhage in cases of vascular injury.
|
|

Figure 3
Pen penetrating the right medial orbital wall in a 21-year-old man. Axial CT of the orbits (A) and lateral CT angiogram (B) with wide bone windows show the metallic writing tip of the pen within the plastic housing (white arrow). There is no penetration of the posterior wall of the sphenoid sinus, and no carotid injury was identified. The pen was removed uneventfully via an anterior approach.
|
|



|
| Author Information |
Daniel R. Lefebvre, MD | Ophthalmic Plastic Surgery, Massachusetts Eye and Ear Infirmary, and Harvard Medical School, Boston, Massachusetts Ronil V. Chandra, MBBS, FRANZCR | Neurointerventional Radiology, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts
|
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in