Traumatic aniridia
Dec 31, 2019
Volume 25, Number 4
Kevin Ma, MD | Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, Boston, Massachusetts
Jo-Ann Haney-Tilton, MD | Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, Boston, Massachusetts
Tedi Begaj, MD | Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, Boston, Massachusetts
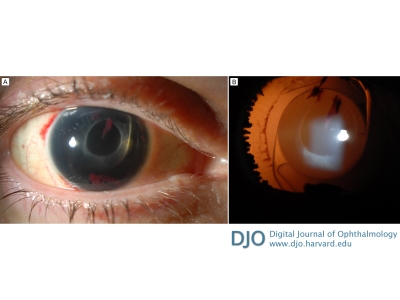
A 49-year-old woman with a remote history of cataract surgery in both eyes presented emergently at the Massachusetts Eye and Ear after blunt injury to her right eye from a mechanical fall. Computed tomography imaging revealed no evidence of orbital fracture nor globe injury. On examination, visual acuity in the right eye was hand motions, and intraocular pressure was normal; a total hyphema prevented visualization of the fundus. The left eye was normal. Examination 2 days later revealed complete 360° avulsion of the iris and a well-centered acrylic intraocular lens within an intact lens capsule (A). The iris had collapsed and was resting in the inferior anterior chamber. On transillumination, ciliary processes and lens zonules were clearly visible (B). Separation of the iris from the ciliary body due to trauma is known as traumatic iridodialysis. Rarely, the entire iris can separate and lead to aniridia. On follow-up, the patient’s visual acuity in the right eye improved to 20/40. She elected not to pursue surgical intervention.
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in