Bartonella neuroretinitis: an optical coherence tomography series
Dec 28, 2018
Volume 24, Number 4
Desiree Albert, MD | Department of Ophthalmology, Henry Ford Health System, Detroit, Michigan
Daniel Brill, MD | Department of Ophthalmology, Henry Ford Health System, Detroit, Michigan
Amit Sangave, MD | Department of Ophthalmology, Henry Ford Health System, Detroit, Michigan
Uday Desai, MD | Department of Ophthalmology, Henry Ford Health System, Detroit, Michigan
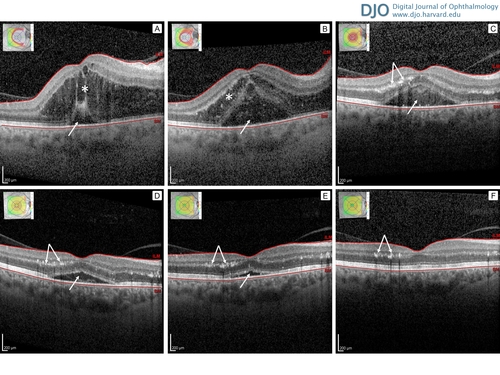
A 57-year-old white woman presented at Henry Ford Hospital with a 3-day history of worsening vision loss in her right eye. On examination, she had visual acuity of 20/400 and optic disc and macular edema. She revealed on questioning that her eye had been exposed directly to cat saliva. She was diagnosed and treated for neuroretinitis secondary to Bartonella henselae and had a good outcome, with 20/25 visual acuity. Her clinical course was documented with serial optical coherence tomographic (OCT) images, which clearly show the disease process of neuroretinitis. Three days after symptom onset (A), there was a large amount of fluid accumulation in the outer retina (star) and a small amount of subretinal fluid (arrow). One week after symptom onset (B), there was fluid movement from the outer retina (star) to the subretinal space (arrow). Two weeks after symptom onset (C), intraretinal fluid resolved, with decreasing subretinal fluid (arrow), and deposition of exudates in the outer plexiform layer (double arrow); clinically, this corresponded with the appearance of a classic “macular star” pattern of hard exudates on fundus examination. Four weeks after symptom onset (D), there was continued improvement in subretinal fluid (arrow) and persistent exudates in the outer plexiform layer (double arrow). Six weeks after symptom onset (E), there was near total resolution in subretinal fluid (arrow) and persistent exudates in the outer plexiform layer (double arrow). Ten weeks after symptom onset, there was total resolution in subretinal fluid, and persistent exudates in the outer plexiform layer (double arrow). BM, Bruch’s membrane; ILM, internal limiting membrane.
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in