Infectious keratitis following laser in situ keratomileusis LASIK
Nov 28, 2016
Volume 22, Number 4
Yuna Rapoport, MD, MPH | Vanderbilt Eye Institute, Vanderbilt University School of Medicine, Nashville, Tennesssee; Massachusetts Eye and Ear Infirmary, Boston, Massachusetts Massachusetts General Hospital, Boston, Massachusetts
Sahar Kohanim, MD, MPH | Vanderbilt Eye Institute, Vanderbilt University School of Medicine, Nashville, Tennessee
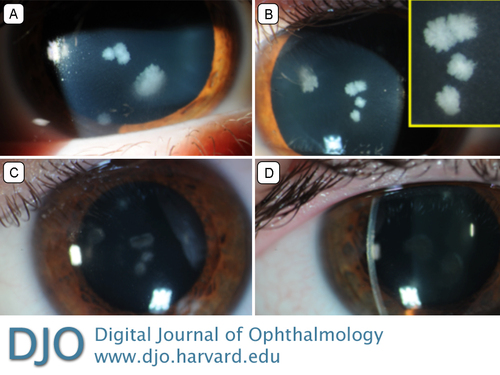
A 22-year-old healthy man who had undergone uncomplicated LASIK 3 weeks prior to presentation at an outside institution presented to the Vanderbilt Eye Institute with 3 days of bilateral blurry vision, photophobia, and pain. The patient was using topical steroids. He denied a history of trauma or contact with organic matter. On examination, best-corrected visual acuity was 20/40 in the right eye and 20/70 in the left. There were multifocal feathery infiltrates within the cornea under the partial-thickness LASIK flaps bilaterally (A-B). The corneal flaps were lifted to culture and irrigate the interface, and moxifloxacin and trimethoprim/polymyxin b were initiated. Cultures grew Mycobacterium chelonae on Löwenstein-Jensen medium, and the antibiotics were switched to amikacin and clarithromycin. Prednisolone acetate was subsequently added. At 8 weeks’ follow-up, the keratitis had fully resolved (C-D), with best-corrected acuity of 20/25 in the right and 20/30 in the left eye. Atypical mycobacteria are a major cause of post-LASIK infections and aggressive treatment directed against these organisms must be considered in all cases of post-LASIK infection. If the infection cannot be controlled with flap irrigation and medical therapy, flap amputation or corneal transplantation should be considered.
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in