Amelanotic choroidal melanoma
Feb 17, 2017
Volume 23, Number 1
Alec L. Amram, MD | Department of Ophthalmology & Visual Sciences, University of Texas Medical Branch
Jaafar El-Annan, MD | Department of Ophthalmology & Visual Sciences, University of Texas Medical Branch, Galveston, Texas
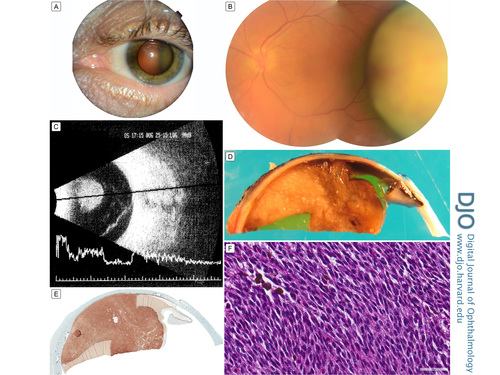
A 53-year-old man presented at the University of Texas Medical Branch – Texas Department of Criminal Justice Ophthalmology Clinic with 1-year history of steady, painless, progressive vision blurring in his left eye. He denied pain or photopsias. The best-corrected visual acuity was 20/30 in the right eye (secondary to the presence of a mild cataract) and counting fingers at 3 feet in the left eye. External (A) and slit-lamp (B) examination revealed a large, dome-shaped, grossly amelanotic mass with superficial vascularization protruding into the temporal vitreous cavity. B-scan ultrasonography (C) revealed a 9.6 × 7.9 mm mushroom-shaped mass with low-to-medium internal reflectivity, suggestive of choroidal melanoma. He was referred to the Oncology Service for metastatic work-up. It was determined that this mass likely represented a primary malignancy. Although he qualified for brachytherapy, this was not an option for him, and he was referred for enucleation. Gross pathology (D) demonstrated a lack of visible melanin pigment but strongly positive MelanA staining throughout (E), confirming melanocytic tumor origin. Hematoxylin-eosin staining (F) demonstrated fascicles of plump spindle cells with large oval nuclei and prominent nucleoli. These cells originated in the choroid and extended through Bruch's membrane in a mushroom configuration confirming the diagnosis of spindle-B amelanotic choroidal melanoma.
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in