|
|
 |
 |
 |
 |
|
|
A 71-year-old man with bilateral vision loss
Digital Journal of Ophthalmology 2017
Volume 23, Number 3
September 3, 2017
DOI: 10.5693/djo.03.2017.03.002
|
Printer Friendly
Download PDF |
|
|



Katy C. Liu, MD, PhD | Department of Ophthalmology, Duke University, Durham, North Carolina Jullia A. Rosdahl, MD, PhD | Department of Ophthalmology, Duke University, Durham, North Carolina Mays El-Dairi, MD | Department of Ophthalmology, Duke University, Durham, North Carolina
|
|
|
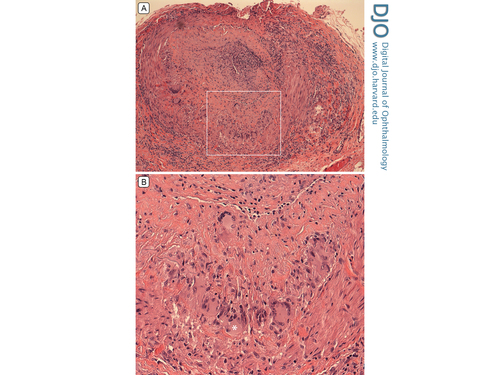
| Diagnosis and Discussion | Pathology of the temporal artery biopsy confirmed intense granulomatous arteritis (Figure 5). In this case, GCA presented as anterior segment ischemia that progressed to ophthalmic artery occlusion. In anterior segment ischemia, the anterior ciliary and long posterior ciliary arteries can be affected, leading to hypoxia, cell death, and inflammation.(1) Anterior chamber reaction can be the first sign of anterior segment ischemia, which likely led to the initial diagnosis of anterior uveitis in this case. Anterior segment ischemia can also manifest with hypotony and corneal edema due to ciliary body nonperfusion and corneal endothelial decompensation, respectively.
Although our patient was previously diagnosed with anterior uveitis, his clinical presentation, examination findings, and ancillary testing pointed to a vascular etiology of acute bilateral vision loss consistent with giant cell arteritis. In a patient >50 years of age, our history elicited several red flags, including severe new-onset headaches, jaw claudication, scalp tenderness, and recent unexplained weight loss.(2) In addition, his ESR and CRP were significantly elevated. Dilated examination of the left eye showed central retinal artery occlusion as well as involvement of posterior ciliary arteries with corneal opacification and hypotony due to anterior segment ischemia; together, the clinical picture favored occlusion of the ophthalmic artery.
It is important to consider the differential diagnosis for acute vision loss to no light perception, because there are few causes for such acute, profound vision loss. One must consider giant cell arteritis, other causes of ophthalmic artery occlusion, optic neuritis (neuromyelitis optica or multiple sclerosis), traumatic optic neuropathy, and nonorganic vision loss. In GCA, up to 21% of cases present with no light perception vision.(3) Although GCA oftentimes presents with evidence of optic disc or retinal ischemia on clinical examination, GCA can less commonly present with anterior segment ischemia,(4) posterior ischemic optic neuropathy, cranial nerve palsies, or Horner’s syndrome.
The visual prognosis of this patient presenting with no light perception in both eyes is poor, and he was lost to follow-up after hospital discharge. In a patient with unilateral or less severe vision loss due to GCA, appropriate and timely treatment may prevent a devastating visual outcome.
| |
|
Figure 5
A, Histopathology (hematoxylin-eosin stain) of temporal artery biopsy showing “intense granulomatous arteritis,” with a nearly occluded artery lumen and inflammation in all vessel layers (original magnification ×10). B, Higher magnification of the segment delineated by the whited box shows multinucleated cells, one of which is indicated by the asterisk (original magnification ×25).
 |
|
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in