|
|
 |
 |
 |
 |
|
|
Photodynamic therapy for peripapillary pachychoroid syndrome—a case report
Digital Journal of Ophthalmology
2022
Volume 28, Number 1
January 27, 2022
|
Printer Friendly
Download PDF |
|
|



George J. Manayath, MS | Department of Retina and Vitreous Services, Aravind Eye Hospital, Coimbatore, India Shishir Verghese, MS | Department of Retina and Vitreous Services, Aravind Eye Hospital, Coimbatore, India Ratnesh Ranjan, MS | Department of Retina and Vitreous Services, Aravind Eye Hospital, Coimbatore, India Venkatapathy Narendran, DNB | Department of Retina and Vitreous Services, Aravind Eye Hospital, Coimbatore, India
|
|
|
| Abstract | | A 76-year-old man presented with reduced visual acuity in both eyes, more severe in the right eye. His previous medical history included anti–vascular endothelial growth factor treatment, with multiple intravitreal injections in both eyes, and repeated focal laser in the left eye. His best-corrected visual acuity was 20/200 in the right eye and 20/40 in the left eye. Based on fundus examination and multimodal imaging, the patient was diagnosed with pachychoroid disease with peripapillary pachychoroid syndrome in the right eye and nasal macular scarring with late cystoid degeneration in the left eye. He underwent low-fluence photodynamic therapy in both eyes. At 6 months’ follow-up, best-corrected visual acuity improved to 20/120 in the right eye and was maintained at 20/40 in the left eye, with good anatomical outcome. | | | Introduction | Peripapillary pachychoroid syndrome (PPS) is a recently described entity in pachychoroid disease spectrum (PDS) characterized by thickening of the choroid close to the optic nerve and intraretinal cystoid spaces and subretinal fluid (SRF) in the nasal macula, with occasional disc edema. (1) PPS shares many features with central serous chorioretinopathy (CSC), including male predilection, thickened choroid, SRF, pigment epitheliopathy, serous pigment epithelial detachments, and gravitational tracks. Its most important distinguishing feature is preferential localization of these changes in the nasal macular region, with a reduction in choroidal thickness sharply toward the temporal side.
Low-fluence verteporfin photodynamic therapy (PDT) has been recommended as the standard of care for chronic CSC management;(2,3) however, effective treatment modalities for PPS are not well described. We report a case of PPS refractory to anti–vascular endothelial growth factor (VEGF) therapy that responded well, both anatomically and functionally, to low-fluence PDT.
| | | Case Report | A 76-year-old man was referred to Aravind Eye Hospital, Coimbatore, with progressive visual decline in the right eye for the previous 2 years and in the left eye for the previous 10 years, despite ongoing treatment. His medical history included anti-VEGF therapy, with multiple intravitreal injections in both eyes and repeated focal laser treatments in the left eye. He had no systemic illnesses. On examination, his best-corrected visual acuity was 20/200 in the right eye and 20/40 in the left eye. Anterior segment examination of both eyes revealed pseudophakia. The axial length in the right eye was 21.63 mm and the left eye was 21.81 mm. Fundus examination of the right eye showed shallow SRF, with areas of retinal pigment epithelial (RPE) degeneration at the fovea and peripapillary region and gravitational tracks in the inferior peripapillary area. The macula of the left eye showed multiple chorioretinal scars suggestive of previous laser marks, RPE mottling surrounding the fovea and peripapillary region, and the presence of an inferior gravitational track. Fundus autofluorescence in the right eye revealed an inferior peripapillary hypoautofluorescent area corresponding to the inferior RPE tract and patchy hyperautofluorescence in the peripapillary region and temporal macula (Figure 1). The left eye showed large hypoautofluorescent spots corresponding to chorioretinal scars, with hyperautofluorescence in the peripapillary area as well as surrounding the hypoautofluorescent areas (Figure 2). In the right eye, spectral domain optical coherence tomography (SD-OCT) revealed shallow SRF, intraretinal cystoid spaces extending from the peripapillary to foveal center, intraretinal hard exudates, and a convex undulating RPE surface on the nasal macula, with juxtapapillary hypertransmission defect. The ellipsoid zone was also disrupted at the nasal macula (Figure 1). In the left eye, SD-OCT revealed intraretinal cystoid spaces, nasal macular scarring at the level of the RPE, ellipsoid zone disruption at the nasal macula, and a thick choroid with the presence of pachyvessels, seen nasal to the fovea and suggestive of late cystoid macular degeneration (Figure 2).
Enhanced-depth imaging OCT in both eyes revealed increased choroidal thickness, with preferentially thickened choroids at the nasal macula. The right eye showed a nasal macular choroidal thickness of 638 µm, subfoveal choroidal thickness of 490 µm, and temporal choroidal thickness of 241 µm; the left eye, 473 µm, 385 µm, and 270 µm thickness, respectively, in the nasal, subfoveal, and temporal macular choroids.
Fundus fluorescein angiogram (FFA) in both eyes revealed areas of stippled hyperfluorescence in the temporal peripapillary region and degenerative tracks along the inferior RPE. The late-phase FFA showed mild disc leakage, with inferior peripapillary and inferotemporal leakage. Indocyanine green angiography (ICGA) showed areas of choroidal hyperpermeability nasal and temporal to the disc, with late-phase washout (Figures 1-2). Left eye ICGA showed additional areas of hypofluorescence corresponding to the laser-induced chorioretinal scars, which were staining on FFA (Figure 2).
Based on the multimodal imaging, a diagnosis of bilateral, chronic pachychoroid disease with right eye peripapillary pachychoroid syndrome and left eye nasal macular scarring with late cystoid degeneration was made. The patient underwent low-fluence photodynamic therapy (PDT) with multiple spots to treat the areas of choroidal hyperfluorescence, sparing the optic nerve head, using 25 J/cm2 energy, 300 mW/cm2 irradiance, 3500 µm spot size, and duration of 83 seconds duration in both eyes. One month after PDT, SD-OCT revealed complete resolution of SRF and intraretinal cystoid spaces in the right eye as well as disappearance of cystoid spaces in the left eye, with a reduction in choroidal thickness in both eyes, which was maintained at 6 months’ follow-up. Nasal macular ellipsoid zone disruption persisted in both eyes. His best-corrected visual acuity improved to 20/120 in the right eye and remained 20/40 in the left eye (Figures 3-4). | |
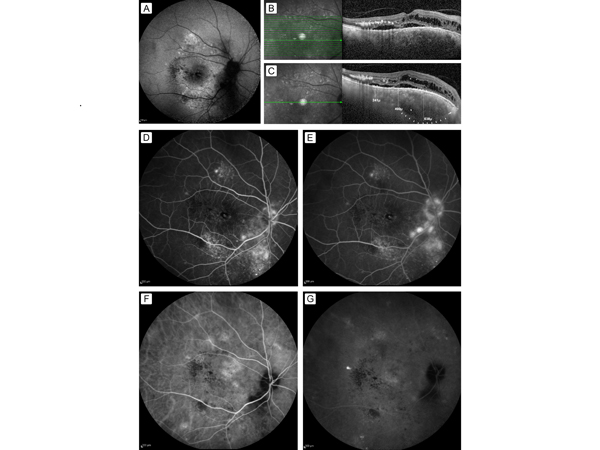
Figure 1.
Multimodal imaging of the right eye. A, Fundus autofluorescence showing inferior peripapillary hypoautofluorescent area corresponding to the inferior retinal pigment epithelium (RPE) tract and patchy hyperautofluorescence in the peripapillary region and temporal macula. B, Spectral domain ocular coherence tomography (SD-OCT) showing shallow serous macular detachment with intraretinal schitic spaces extending from the peripapillary to foveal area, with intraretinal hard exudates and a convex undulating RPE surface on the nasal macula along with ellipsoid zone disruption. C, Enhanced-depth imaging OCT showing a preferential nasal choroidal thickness of 638 µm, subfoveal choroidal thickness of 490 µm, and temporal choroidal thickness of 241 µm, with a juxtapapillary hypertransmission defect (arrow). D, Fundus fluorescein angiogram showing areas of stippled hyperfluorescence in the temporal peripapillary region and the inferior RPE degenerative track in the mid-phase. E, Late-phase image showing a mild disc leakage, with increasing hyper fluorescence in the inferior peripapillary and inferotemporal area. F-G, Indocyanine green angiogram showing choroidal hyperpermeability nasal and temporal to the disc (F) with late-phase washout (G).
|
|
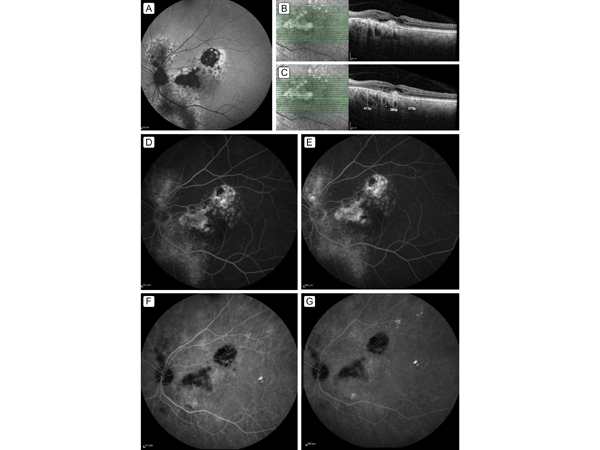
Figure 2.
Multimodal imaging of the left eye. A, Fundus autofluorescence showing large hypoautofluorescent spots corresponding to laser-induced chorioretinal scars, with peripapillary hyperautofluorescence and surrounding patchy hyperautofluorescence. B, SD-OCT showing intraretinal cystoid spaces, nasal macular scarring at the level of the RPE, and ellipsoid zone disruption at the nasal macula. C, Thick choroid along with the presence of pachyvessels was seen nasal to the macula with choroidal thickness of 473 µm; subfoveal and temporal macular choroidal thickness were 385 µm and 270 µm, respectively. D-E, Fundus fluorescein angiogram showing areas of peripapillary and inferior track hyperfluorescence (D), with late leakage and staining of the multiple laser induced chorioretinal scars (E). F-G, Indocyanine green angiogram showing areas of choroidal hyperpermeability along with hypofluorescence corresponding to areas of scarring (F) and late-phase washout (G).
|
|
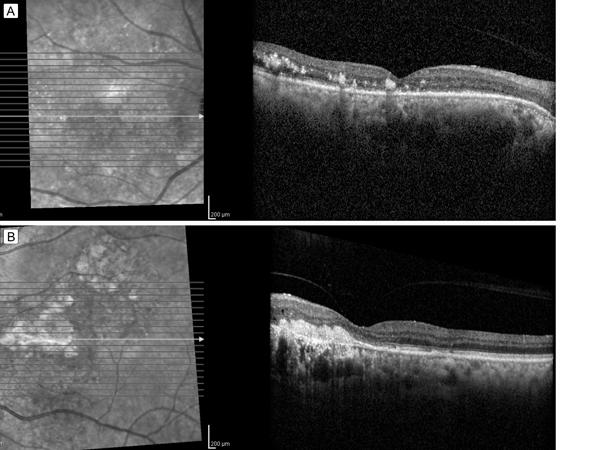
Figure 3.
SD-OCT 1 month after treatment showing complete resolution of subretinal fluid and intraretinal cystoid spaces in the right eye (A) and disappearance of cystoid spaces in the left eye (B).
|
|
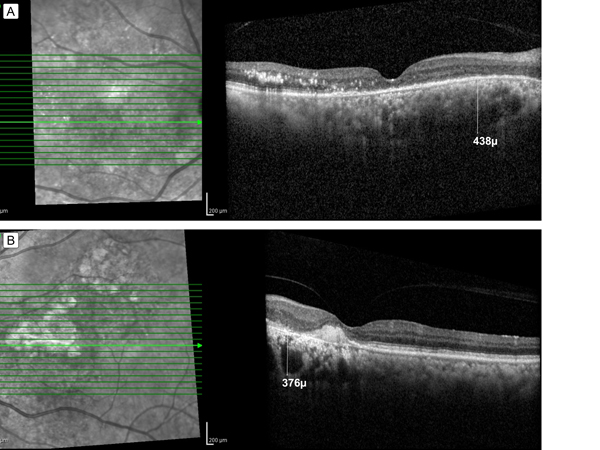
Figure 4.
SD-OCT 6 months after treatment showing mild foveal thinning with photoreceptor layer absence and hard exudates in the right eye (A) and foveal thinning with photoreceptor absence and juxtafoveal hyperreflective lesion consistent with scar in the left eye (B). Note the reduction in choroidal thickness in both eyes (438 µm in the right eye and 376 µm in the left eye) and the persistent nasal ellipsoid zone disruption.
|
|
| Discussion | The primary pathology in PDS is thickened choroid, which may be focal or diffuse and foveal or extrafoveal, along with congested and hyperpermeable choroidal vasculatures, with compressed choriocapillaris causing an overlying RPE dysfunction that leads to leakage of fluid into the subretinal space.(4) PPS is a novel PDS disorder, where the morphological pachychoroid features are found in the peripapillary area and nasal macula rather than at the fovea.(1) CSC and PPS share features, as noted above.(1) Similar to CSC, ICGA findings in PPS include pachyvessels and choroidal hyperpermeability; however, choroidal changes in PPS are preferentially localized to the nasal macula, as seen in our patient. Various treatment options tried for chronic CSC include subthreshold micropulse laser, PDT, and mineralocorticoid antagonists, such as spironolactone and eplenerone.(3,5,6) Anti-VEGF treatment has also been used in cases of chronic CSC, but without promising effects.(7) Currently, low-fluence PDT has been recommended as the treatment of choice for chronic CSC. However, treatment modalities for PPS as a relatively newly described entity, have been little described.(1,8)
Phasukkijwatana et al,(1) in the first and largest series of PPS cases, reported the response in PPS patients to various treatments, including anti-VEGF injection, PDT, and topical and systemic carbonic anhydrase inhibitors. Three eyes treated with anti-VEGF injections did not respond. Alonso-Martin et al also treated a case of PPS with multiple injections of different anti-VEGF agents, including bevacizumab, aflibercept, and ranibizumab. They reported waxing and waning of SRF but no final reduction in central macular thickness.(8) Similarly, our patient also was treated with multiple anti-VEGF injections, although elsewhere, as chronic CSC, there was no functional or anatomical improvement.
Of the 3 eyes treated with PDT reported by Phasukkijwatana et al, 1 had resolution of the macular fluid; however, the authors did not provide details regarding fluence or other PDT treatment parameters, and the functional outcome in that eye was not reported.
With the benefit of a clearer picture of the PPS variant of PDS, we diagnosed our patient with chronic pachychoroid disease in both eyes, with PPS in the right eye and nasal macular scarring and cystoid degeneration in the left eye, based on multimodal imaging. In view of the chronic nature of the disease as well as previous failed treatments with anti-VEGF injections, we decided to perform low-fluence PDT bilaterally. Multispot PDT was performed, aimed at the areas of diffuse choroidal hyperpermeability and sparing the optic nerve head. The treatment resulted in good anatomical improvement and stabilization of vision in both eyes at 6 months’ follow-up.
In CSC, PDT induces the remodeling of choroidal vasculature, with the reduction of choroidal hyperpermeability and the underlying choroidal thickness;(9) reduced choroidal hyperpermeability leads to resolution of SRF. In chronic CSC, low-fluence and low-dose PDT have shown promising therapeutic effect on the choroidal circulation while also providing a safety margin.(10)
Our report highlights the successful outcome following low-fluence PDT for PPS refractory to other treatment modalities. Large, prospective studies are needed to confirm the efficacy of low-fluence PDT in PPS.
| | | References | 1. Phasukkijwatana N, Freund KB, Dolz-Marco R, et al. Peripapillary pachychoroid syndrome. Retina 2018;38:1652-67.
2. Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol 2013;58:103-26.
3. Ma J, Meng N, Xu X, Zhou F, Qu Y. System review and meta-analysis on photodynamic therapy in central serous chorioretinopathy. Acta Ophthalmol (Copenh) 2014;92:e594-601.
4. Cheung CMG, Lee WK, Koizumi H, Dansingani K, Lai TYY, Freund KB. Pachychoroid disease. Eye (Lond) 2019;33:14-33.
5. Chen S-N, Hwang J-F, Tseng L-F, Lin C-J. Subthreshold diode micropulse photocoagulation for the treatment of chronic central serous chorioretinopathy with juxtafoveal leakage. Ophthalmology 2008;115:2229-34.
6. Bousquet E, Beydoun T, Zhao M, Hassan L, Offret O, Behar-Cohen F. Mineralocorticoid receptor antagonism in the treatment of chronic central serous chorioretinopathy: a pilot study. Retina 2013;33:2096-102.
7. Unlü C, Erdogan G, Aydogan T, et al. Intravitreal bevacizumab for treatment of central serous chorioretinopathy. J Ophthalmic Vis Res 2016;11:61.
8. Alonso-Martín B, de-Lucas-Viejo B, Gimeno-Carrero M, Ferro-Osuna M, Sambricio J. Diagnosis by multimodal imaging in peripapillary pachychoroid syndrome: a case report. Arch Soc Esp Oftalmol Engl Ed 2020;95:248-53.
9. Izumi T, Koizumi H, Maruko I, et al. Structural analyses of choroid after half-dose verteporfin photodynamic therapy for central serous chorioretinopathy. Br J Ophthalmol 2017;101:433-7.
10. Lai TYY, Wong RLM, Chan W-M. Long-term outcome of half-dose verteporfin photodynamic therapy for the treatment of central serous chorioretinopathy (an American Ophthalmological Society Thesis). Trans Am Ophthalmol Soc 2015;113:T8. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in