|
|
 |
 |
 |
 |
|
|
Segmental removal of infected frontalis sling
Digital Journal of Ophthalmology
2021
Volume 27, Number 4
November 14, 2021
|
Printer Friendly
Download PDF |
|
|


 Snehaa V. Maripudi, MD
Snehaa V. Maripudi, MD | Department of Ophthalmology and Visual Sciences, University of Maryland School of Medicine, Baltimore, Maryland Francis Lawson Grumbine, MD | Department of Ophthalmology and Visual Sciences, University of Maryland School of Medicine, Baltimore, Maryland; Department of Ophthalmology, Greater Baltimore Medical Center, Baltimore, Maryland Shannath Merbs, MD, PhD | Department of Ophthalmology and Visual Sciences, University of Maryland School of Medicine, Baltimore, Maryland Janet Leath Alexander, MD | Department of Ophthalmology and Visual Sciences, University of Maryland School of Medicine, Baltimore, Maryland
|
|
|
| Abstract | | Congenital ptosis is one of the most common oculoplastic diseases of infancy. Where there is poor levator function, a frontalis sling is the procedure of choice. Here, we describe 2 cases of frontalis sling extrusion that were managed by segmental sling removal, with favorable results. In case 1, an infant developed silicone extrusion 2 months after bilateral frontalis sling implantation. The exposed segment was excised, and the area healed quickly without recurrence of infection and lid height remained optimal. Case 2 developed recurrent brow abscesses during the 3 years following bilateral frontalis sling. Surgical revision involved excision of the involved sling segment for definitive control of the chronic recurrent infection. Adjustment at the time of segmental excision resulted in improved eyelid position. These cases demonstrate that postoperative infection with implant exposure can be managed by partial sling removal, which may be the preferred procedure in children in order to minimize the number of procedures and exposure to general anesthesia. | | | Introduction | | Congenital blepharoptosis may require timely surgical correction to mitigate the risk of amblyopia. We report 2 cases of congenital blepharoptosis with chronic infections related to silicone extrusion following treatment with frontalis sling placement. Both cases were surgically revised, with relatively little tissue manipulation, and both cases resulted in optimal eyelid height. | | | Case Report | Case 1
A 3-month-old girl with mosaic chromosome 3p deletion syndrome and multiple cardiac anomalies was referred to University of Maryland Ophthalmology because she had not opened her eyes since birth. Her condition was initially attributed to medical illness and sedation but later became concerning to her primary physician. On examination, it was determined that she had congenital ptosis, with poor levator function. One week after presentation, bilateral frontalis sling surgery with silicone was performed using the single rhomboid technique.(1) Her early postoperative course was uncomplicated. By postoperative week 2, she was demonstrating reliable fix-and-follow visual acuity in each eye.
By postoperative month 2, she developed a 3 mm abscess over the left eyebrow. The abscess was surgically drained after 2 days of clindamycin via gastrostomy tube. The defect was closed in layered fashion with mattress sutures to ensure complete coverage of the sling. The surgical specimen demonstrated no bacterial growth. One month later, the wound appeared to be healing well with appropriate scar formation (Figure 1A). However, 2 weeks later, the wound reopened, and the sling was visible through the drainage site. Four days prior to her scheduled revision, she presented because her parents were concerned that the patient’s condition had worsened and required earlier intervention. On examination, the sling had folded anteriorly, and approximately 2 mm was protruding from the site of the previous surgical wound (Figure 1B).
The prolapsed portion of the sling was removed in clinic, with the child awake and swaddled. Given that the implant was easily accessible with minimal manipulation, no local anesthetic was used; no internal tissue was manipulated during the procedure. The exposed sling was grasped with forceps, pulled out, and cut at the level of the skin. Ten millimeters of silicone sling was removed, and the entire remaining portion of the sling was left in the skin. The removed portion did not include any silicone sleeve, which had remained in place and unexposed. The wound was cleaned with betadine before and after. The intent was to reduce the presence of potentially infectious material and fully remove and replace the sling later in the same week, under the assumption that her ptosis would recur.
Four days later, the lid height was excellent, and the wound nearly fully healed. The family elected not to proceed with surgery. The patient was followed at least once every 6 months to ensure eyelid height remained at its optimal level. At the most recent follow-up examination, at 23 months of age, the patient’s brow was completely healed, eyelid height was symmetric, and vision was normal for age (Figure 1C).
Case 2
A 3-month-old healthy boy presented with bilateral congenital ptosis with poor levator function. At 2 years of age, he underwent bilateral frontalis sling surgery with silicone, using a single rhomboid technique.(1) At postoperative month 1, he was found to have a left forehead abscess (Figure 2A), which was drained and cultured, growing Staphlococcus warneri. The patient was treated with oral amoxicillin, and the infection resolved and remained stable for more than 1 year. At postoperative month 18, another abscess developed (Figure 2B) and was treated with the same oral antibiotic and surgical incision and drainage with culture (resulting in no growth). The wound remained fully healed for 1 year (Figure 2C). When the patient was 4.5 years of age, a third abscess developed, over 2 years after the initial surgery.
The third occurrence was treated by segmental sling removal. For this case, the cut ends of the removed segment were joined using a polypropylene suture conduit. Polypropylene was chosen because it is nondissolvable and has a good anti-infective profile. Intraoperatively, after drainage of the skin abscess, debridement of the wound margin, and thorough irrigation with normal saline, the sling was hooked using a small von Graefe muscle hook and pulled anteriorly. The center of the exposed portion was marked with a sterile marking pen. Two 6-0 polypropylene sutures were then tied around the sling, one on either side of the marked location, at 5 mm distance from the central marked location. The 10 mm segment between the sutures was cut out and sent for culture (no growth identified). The cut sling ends were brought together by tying the two sutures, for a total of 10 mm of excised silicone segment. The wound was cleaned with betadine before and after the procedure.
The preoperative goal was 3 mm of eyelid elevation, and it was felt that removal of 10 mm of the sling’s circumference would offer this result, based on the assumption that the sling is a roughly circular conduit. In this way, the potentially infected portion of the implant was removed, and the overall diameter of the sling was reduced to address eyelid asymmetry that was clinically evident but nonamblyogenic (Figure 2D). Eyelid symmetry had improved at post operative month 1 (Figure 2E). At 7 years of age, 5 years after his initial sling placement, the patient maintained excellent eyelid symmetry. | |
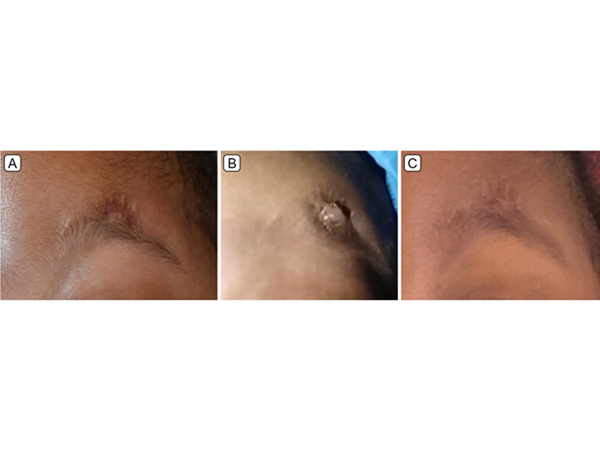
Figure 1.
A, One month after initial surgery. B, Sling extrusion 2 months postoperatively. C, One year after segmental removal.
|
|

Figure 2.
A, Left forehead abscess 1 month postoperatively. B, Recurrence of abscess. C, One year after abscess drainage. D, Eyelid asymmetry after initial procedure. E, Postoperative month 1 after segmental removal to address infection and correct asymmetry.
|
|
| Discussion | In these cases, segmental sling removal effectively managed localized infection of silicone frontalis sling with extrusion. In both cases, the eventual outcomes were favorable, and the patients’ exposure to general anesthesia was minimized. Silicone is conducive to subsequent modification and minimally invasive revision in children. Other sling materials, such as Goretex or Supramid may be similarly adjustable.
General surgical principle dictates that implanted material be removed in the setting of infection.(2) In frontalis sling surgery, complete silicone sling removal must be considered for complications such as infection and extrusion.(3) Typically, the sling is replaced at a subsequent surgery. Our cases suggest that partial removal of potentially infected material, rather than total implant removal, may also be sufficient to control a localized infection. Potential issues of leaving infected foreign material in a patient include recurrent infection and inflammation. Complete removal of infected sling material also has disadvantages, however, including additional tissue manipulation, possible need for multiple sling replacements with sterile implant, and additional exposure to general anesthesia.
Case 1 illustrated a previously reported but nonetheless surprising feature of the silicone frontalis sling that was essential to the success of the segmental removal technique: permanence of the lifting effect.(4,5) The perpetual elevation effect noted in this case allowed for a quick in-clinic revision, sparing the young patient from additional general anesthesia and tissue manipulation. Similar results were noted by Wojno and Green, who described multiple cases of complete silicone sling removal without recurrence of ptosis for at least 3 years, seemingly because of the persistence of bands of scar tissue continuing to perform a suspensory function.(4,5) This case further supports the frontalis suspensory effect of scar tissue in a younger patient and demonstrates that the same effect can be obtained without complete sling removal. Late failure is a potential long-term risk of sling segment removal, and this risk is similarly present with an intact sling.(6)
The sling revision in case 2 demonstrated the same segmental removal of the implant as case 1, allowing for complete resolution of a chronic brow abscess associated with sling extrusion. Case 2 also featured an adjustment technique to improve eyelid height when removing an exposed segment of silicone frontalis sling. For this procedure, the goal of 3 mm of eyelid elevation was determined preoperatively. We calculated that removal of a 10 mm segment of sling would achieve this result (assuming a roughly circular shape to the conduit, so that a 10 mm reduction in circumference would reduce the diameter/height by about 3 mm) (C=?d). Although this calculation oversimplifies the three-dimensional nature of sling placement, it offers a simple heuristic starting point that can be further adjusted intraoperatively based on the surgeon’s judgement.
These cases suggest that partial sling removal has a role in cases of localized sling extrusion. Because small amounts of asymmetry may occur in up to 5% of bilateral and unilateral frontalis sling patients after correction of congenital ptosis,(5) this procedure offers added benefit of concurrent adjustment, if needed, to elevate the eyelid height and improve symmetry. Although these results may not be universally generalizable, under controlled circumstances for patients requiring frontalis sling revision, this simple revision technique may serve well.
Funding support: UMB ICTR/Clinical Science and Translational Science KL2 Award 1KL2TR003099-01 (JLA). | | | References | 1. Katowitz JA. Pediatric Oculoplastic Surgery.New York: Springer; 2013.
2. Mulholland MW. Greenfield’s Surgery: Scientific Principles and Practice. 6th ed. Philadelphia:Lippincott Williams and Wilkins; 2017.
3. Bansal RK, Sharma S. Results and complications of silicone frontalis sling surgery for ptosis. J Pediatr Ophthalmol Strabismus 2015;52:93-7.
4. Wojno TH, Green JP. Sling removal. Ophthalmic Plast Reconstr Surg 2000;16:79-80.
5. Green JP, Wojno T. Removal of an infected silicone rod frontalis sling without recurrence of ptosis. Ophthal Plast Reconstr Surg 1997;13:285-6.
6. Pacella E, Mipatrini D, Pacella F, et al. Suspensory materials for surgery of blepharoptosis: a systematic review of observational studies. PLoS One 2016;11:e0160827.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in