|
|
 |
 |
 |
 |
|
|
Anterior “beaded” emulsification as a late complication of heavy silicone oil in retina surgery
Digital Journal of Ophthalmology
2021
Volume 27, Number 1
March 20, 2021
DOI: 10.5693/djo.02.2021.01.002
|
Printer Friendly
Download PDF |
|
|


 Ahmed N. Zewar, MBBS, FRCS
Ahmed N. Zewar, MBBS, FRCS | Department of Ophthalmology, St. Mary’s Hospital, Isle of Wight, United Kingdom Jonathan Lochhead, FRCOphth | Department of Ophthalmology, St. Mary’s Hospital, Isle of Wight, United Kingdom
|
|
|
| Abstract | | We report 2 cases of emulsified silicone oil with a “beaded” appearance adherent to the posterior capsule as a long-term complication of heavy silicone oil tamponade in retina surgery. One case demonstrated mobile beaded opacity that has not been described in the literature previously. This heavy silicone oil complication might cause symptoms similar to posterior capsular opacity. Nd:YAG posterior capsulotomy can be considered as a treatment. | | | Introduction | Heavy silicone oils (HSOs) are indicated for use in the treatment of complex inferior retinal detachments and inferior giant retinal tears. In these cases, use of HSO can reduce the patient’s need for positioning postoperatively. A mixture of 5,000 mPas silicone oil (specific gravity of 0.97 g/cm3) and of 3.5 mPas perfluorohexyloctane F6H8 (specific gravity, 1.33 g/cm3), HSO is slightly heavier (1.06 g/cm3) than water, with a midrange viscosity (1,480 mPas).(1)
Relatively rapid emulsification is a feature of HSO that generally limits tamponade duration. Surgical removal of HSO can be challenging because of its viscosity and a more posterior aspiration that is required. “Sticky” silicone oil during removal has been described in the literature where heavy liquid and silicone oil have been used.(2) We report 2 cases where there was an appearance of “beaded” emulsification resulting from HSO entrapment between the posterior capsule and the intraocular lens (IOL) several years after its removal.
| | | Case Report | Case 1
A 64-year-old myopic man was referred to the eye unit of St Mary’s Hospital with macula-on inferior retinal detachment in the left eye, with a best-corrected visual acuity of 6/6. He underwent an uneventful 25-G pars plana vitrectomy (PPV), cryopexy and HSO (Densiron 68; Fluoron, Ulm, Germany) endotamponade. Anatomical success was achieved. Four months later, a combined phacoemulsification with insertion of a single-piece acrylic IOL (AcrySof SN60WF; Alcon Laboratories, Fort Worth, TX) and PPV with HSO removal was performed without complication. Over the following visits, he maintained a flat retina, with a visual acuity of 6/6, but he developed secondary ocular hypertension, and some emulsified HSO droplets were found in the anterior segment with inferior pseudohypopyon, for which he underwent an anterior chamber wash out.
Four years after the HSO removal, the patient presented with blurred vision and glare in the left eye; on slit-lamp examination, there was a glistening beaded appearance of compressed silicone oil droplets between the posterior capsule and the IOL (Figure 1). This location was confirmed after a successful Nd:YAG laser posterior capsulotomy under a magnified view (Figure 2).
Case 2
A 55-year-old diabetic man presented with right vitreous hemorrhage in addition to a localized inferior tractional retinal detachment (TRD). He underwent a right combined phacoemulsification with insertion of a single-piece acrylic IOL (AcrySof SA60AT) and 25-G PPV with delamination, membrane dissection, endolaser, and HSO (Densiron 68) injection. Six months later, he developed further preretinal fibrosis and TRD in addition to increased ocular pressure due to pupillary block. Another 25-G PPV was performed in which the HSO was removed, with inferior iridectomy, delamination, inferior retinectomy under heavy liquid, and endolaser followed by silicone oil 5500 cS injection. Postoperatively the inferior TRD remained stable under silicone oil fill with a final visual acuity of 6/18.
Six years later, an asymptomatic glistening emulsification was seen superficial to the posterior capsule of the right eye resulting from small and compressed HSO droplets. These microspheres of silicone oil arose between the IOL and the posterior capsule arranged in a beaded pattern similar to the previous case (Figure 3A). Three months later, the HSO bubbles were observed at different locations within the capsular bag while keeping the same characteristic beaded appearance (Figure 3B). | |
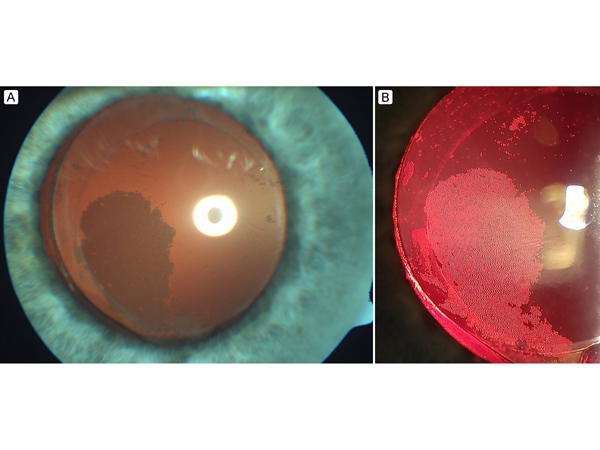
Figure 1.
A, Photograph of the HSO-related posterior capsular opacity. B, Slit-lamp trans-illumination image showing the beaded structure of the emulsified HSO on the anterior surface of posterior capsule.
|
|
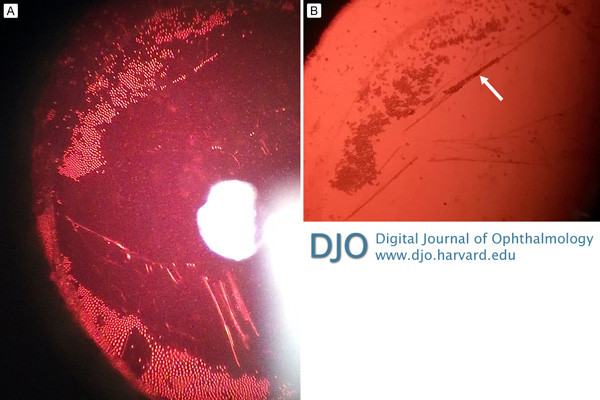
Figure 2.
A, Redistribution of HSO droplets between the IOL and the remains of the posterior capsule after YAG-posterior capsulotomy. B, Magnified view, showing sticky HSO beads (arrow) to the anterior surface of the torn edge of the posterior capsule.
|
|

Figure 3.
Slit-Lamp biomicroscopic images. A, At first follow-up examination, showing compressed beaded heavy silicone oil on the lateral side of the posterior capsule. B, Three months later, showing beaded heavy silicone oil bubbles having separated and moved to superior and inferior locations.
|
|
| Discussion | Densiron 68 has been used widely by vitreoretinal surgeons in managing complex retinal detachments involving the inferior retina, particularly with associated proliferative vitreoretinopathy. It can provide a good endotamponade for both the inferior and the posterior pole with normal head positioning.(3) Nevertheless, its reactions with different ocular structures and resultant complications make it unsuitable as a long-term endotamponade. These reactions include early emulsification, dispersion, cataract, ocular hypertension, prolonged inflammatory reactions, and membrane formation.(4)
One of the rarer complications described is the phenomenon of “stickiness,” which is largely due to two main factors, namely, reduced surface tension of the surrounding aqueous material and contamination of silicone oil with intraoperative heavy liquid.(5)
In the cases reported here, we document unusual beaded opacity on the anterior surface of the posterior capsule occurring 4-6 years after removal of Densiron 68. To our knowledge, this is the first case series to describe such an appearance in pseudophakic eyes as a late complication of HSO, occurring many years after removal. Both cases had HSO in situ for 4-6 months; 1 case then subsequently had a procedure requiring heavy liquid followed by long-term silicone oil 5500 cS. Densiron 68 contains both components linked to sticky silicone oil observations. Sticky HSO droplets entering the capsular bag through the zonules with subsequent emulsification could explain our cases.
Sim et al reported a case of intraoperative firm adhesion of an HSO (Oxane HD) to the posterior capsule of a phakic patient in addition to the posterior pole, giving it an hourglass appearance.(6) Yesilirmack et al described a similar appearance of adhered Densiron 68 to the anterior surface of the posterior lens capsule in a pseudophakic patient only 5 months after its removal.(7)
In our cases, the mechanism of this glistening beaded appearance is not known. Contributing factors might include the hydrophobic nature and “tacky” surface of Acrysof IOLs, which could lead to adherence with the posterior capsule.(8) This consequently compresses the trapped silicone oil droplets, which may increase the shear forces within the droplets but decrease the interfacial tension between silicone oil and the IOL. These factors increase silicone oil tendency to disperse into ever smaller spheres.(9) Both of our patients have the same type of IOL inserted in their eyes.
The period between HSO insertion and formation of the beaded capsular opacity is related to the fact that emulsification is time dependent. This is speculated to depend on a combination of the density difference between intraocular fluids and silicone oil, saccadic eye movement, and the gradual decline of the oil’s interfacial surface tension due to the adsorption of surface-active components from the intraocular fluids.(9) Both of our cases presented very late. Contact between remaining lens epithelial cells and oil droplets may stimulate a foreign body reaction, with release of extracellular matrix components.(10) This possibly changes surface tension and emulsification properties, contributing to the formation of partitions between silicone oil droplets in a beaded pattern.
In the second case, we believe that the beaded appearance was due to the HSO rather than to silicone oil 5500 cS or heavy liquid. The similar appearance to the first case and noticing no identical complication after using silicone oil with or without heavy liquid, either in our practice or on reviewing the literature, led us to this conclusion. The observed change in distribution of the HSO microspheres suggests that there is some potential mobility of emulsified oil if a cavity or space persists in front of the posterior capsule. This suggests that stickiness may not be an important factor in the formation of this late complication. Alternatively, it may indicate that any potential stickiness can still be overcome by natural saccadic eye motions.
Both patients had undergone phacoemulsification with IOL insertion at the same time when Densiron 68 was also removed from (case 1) or injected inside (case 2) the eye. These combined surgeries with the more liability to disrupt the lens zonular apparatus may explain the pathway through which silicone oil droplets got access to the capsular bag.
These 2 cases highlight the characteristic ability of emulsified HSO to stick to different ocular structures and even to separate and mobilize depending on certain biologic and dynamic factors. In both cases, the complication appeared many years after HSO removal.
Literature Search
Vitreoretinal books and PubMed were searched in March and April 2020, for English language results, using the following terms: sticky heavy silicone oil, heavy silicone oil emulsification, adhesion of heavy silicone oil, and silicone oil–induced posterior capsular opacity. | | | References | 1. Joussen AM, Gardner TW, Kirchhof B, Ryan SJ. Retinal Vascular Disease. Berlin: Springer; 2007:264.
2. Williamson TH. Vitreoretinal Surgery. 2nd ed. Heidelberg: Springer; 2013:83.
3. Rizzo S, Caporossi T, Finocchio L, Tartaro R, Barca F. Heavy oils in vitreoretinal surgery: Heavy tamponades have utility in managing complex retinal detachment. Retinal Physician 2018;15:45, 46, 48, 52.
4. Mete M, Parolini B, Maggio E, Pertile G. 1000 cSt silicone oil vs heavy silicone oil as intraocular tamponade in retinal detachment associated to myopic macular hole. Graefes Arch Clin Exp Ophthalmol 2011; 249:821-6.
5. Dresp JH, Menz DH. The phenomenon of sticky silicone oil. Graefes Arch Clin Exp Ophthalmol 2007; 245:863-8.
6. Sim KT, Hero M. Adhesion of heavy oil to posterior lens capsule. Retina 2006; 26:964-5.
7. Yesilirmak N, Pinarci EY, Akkoyun I, Yilmaz G. Adhesion of heavy silicone oil to the anterior surfaces of the posterior lens capsule. Eur J Ophthalmol 2013;23:436-8.
8. Oshika T, Nagata T, Ishii Y. Adhesion of lens capsule to intraocular lenses of polymethylmethacrylate, silicone, and acrylic foldable materials: an experimental study. Br J Ophthalmol 1998;82:549-53.
9. Barca F, Caporossi T, Rizzo S. Silicone oil: different physical proprieties and clinical applications. Biomed Res Int 2014;2014:502143.
10. Miyamoto T, Saika S, Yamanaka A, et al. Deposition of silicone oil droplets in the residual anterior lens capsule after vitrectomy and lensectomy in rabbits. Br J Ophthalmol 2004; 88:703-7.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in