|
|
 |
 |
 |
 |
|
|
Intracapsular hemorrhage in the setting of pseudoexfoliation syndrome
Digital Journal of Ophthalmology
2020
Volume 26, Number 2
June 20, 2020
DOI: 10.5693/djo.02.2020.02.003
|
Printer Friendly
|
|
|


 Jean H. Park, MD
Jean H. Park, MD | Department of Ophthalmology, Geisinger Medical Center, Danville, Pennsylvania William Ensor, DO | Department of Ophthalmology, Geisinger Medical Center, Danville, Pennsylvania Joanna Olson, MD | Department of Ophthalmology, Geisinger Medical Center, Danville, Pennsylvania Benjamin Hale, MD | Department of Ophthalmology, Geisinger Medical Center, Danville, Pennsylvania
|
|
|
| Abstract | | We report the case of an 84-year-old man who presented with decreased vision in his left eye. Ocular history included bilateral pseudoexfoliative glaucoma and vitelliform macular dystrophy. He had undergone intraocular lens placement in both eyes 6 years before presenting at our institution. Over follow-up of 4 years, he experienced recurrent spontaneous hyphema and continued residual intracapsular hemorrhage. He was eventually diagnosed with uveitis-glaucoma-hyphema syndrome in the setting of pseudoexfoliation. | | | Introduction | | Uveitis-glaucoma-hyphema (UGH) syndrome was first reported by Ellingson in 1978 as a complication of iris chafing by an anterior chamber intraocular lens (IOL).(1) This rare syndrome is classically associated with poorly positioned IOLs in the anterior chamber or sulcus. More recently, in-the-bag posterior chamber IOLs have been recognized as a cause of UGH syndrome. Recent case reports also highlight pseudoexfoliation syndrome, pseudophacodonesis, and haptic displacement through compromised capsular defects as mechanisms for UGH syndrome.(2-4) | | | Case Report | An 84-year-old man was referred to Geisinger Medical Center for evaluation of decreased vision in the left eye of 3 days’ duration. He denied any change in his usual medical history. His current medications included warfarin for paroxysmal atrial fibrillation, with a therapeutic international normalized ratio (INR) of 2.5, managed by an anticoagulation clinic. Past ocular history included pseudoexfoliative glaucoma and vitelliform macular dystrophy in both eyes. His past ocular surgical history included trabeculectomy in the left eye and uneventful cataract extraction with implantation of a one-piece intraocular lens (IOL) in the bag in both eyes at an outside clinic approximately 6 years prior. He denied a history of trauma to either eye.
On examination, corrected visual acuity was 20/30 in the right eye and hand motions in the left eye, decreased from his baseline visual acuity of 20/200. Intraocular pressure (IOP) was 16 mm Hg in the right eye and 8 mm Hg in the left eye. Examination of the right eye showed a well-positioned posterior chamber IOL in the bag with pseudoexfoliative material at the pupillary border, cup-to-disc ratio of 0.6, and a subfoveal vitelliform lesion. Examination of the left eye revealed a healthy bleb located in the superonasal conjunctiva, without evidence of a leak or blebitis. The anterior chamber showed 4+ red blood cells (RBCs), with a 2 mm layered hyphema obscuring a view of the posterior pole. B-scan ultrasonography revealed vitreous syneresis with intact retina. The patient was started on topical prednisolone 4 times daily and atropine twice daily.
He returned after 1 week with resolution of the hyphema but residual RBCs in the anterior chamber. His examination was most notable for settled hemorrhage between the IOL and posterior capsule (Figure 1). There was no evidence of iris transillumination defects or neovascularization. Pseudoexfoliative material on the anterior capsule, iridodonesis, and pseudophacodonesis were all noted. The posterior pole could be visualized. The cup-to-disc ratio was 0.9, and there was a subfoveal vitelliform lesion, with no evidence of posterior segment neovascularization. On gonioscopy, the angle was open, with heavily pigmented trabecular meshwork but without neovascularization of the angle. At this time, the exact etiology of his hyphema was unknown.
The patient returned 5 months after initial presentation with recurrent hemorrhage filling the entire capsular bag that did not completely resolve, with residual persistent staining at the most recent follow-up visit examination (Figure 2), about 4 years after initial presentation. Visual acuity in the left eye has remained light perception only.
Three years after initial presentation, the right eye developed a spontaneous hyphema. The IOL appeared stable and in good position, and no other abnormal examination findings were identified, including iris transillumination defects. His INR remained in therapeutic range of 2.8. Fluorescein angiography of the anterior segment of both eyes confirmed no iris neovascularization or arteriovenous malformation.
Given a history of pseudoexfoliative glaucoma, uveitis-glaucoma-hyphema (UGH) syndrome was felt to be the likely etiology for spontaneous hyphema in both eyes. Of note, access to ultrasound biomicroscopy was unavailable at our institution, and it was recommended to the patient that he obtain this testing at an outside facility, but the patient declined. | |
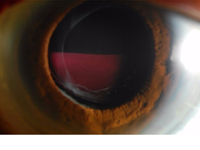
Figure 1
Clinical photograph of patient 1 week after initial presentation showing hemorrhage between the intraocular lens and posterior capsule.
|
|

Figure 2
Residual hemorrhage staining the capsular bag at the most recent follow-up examination, approximately 4 years after initial presentation.
|
|
| Discussion | We present a case of bilateral spontaneous hyphema likely secondary to UGH syndrome in the setting of pseudoexfoliative glaucoma. Single-piece IOLs placed in the bag are a rare cause of UGH syndrome. Zhang et al proposed a mechanism for in-the-bag UGH syndrome in a patient with pseudoexfoliation: zonular instability leading to subclinical pseudophacodonesis of the haptic-capsule complex resulting in chafing of the posterior iris.(2) In our case, we believe pseudophacodonesis of the IOL-capsule complex caused iris chafing leading to hyphema. We believe the prolonged clearing of intracapsular hemorrhage was exacerbated by the patient’s anticoagulation status. Yalinbas et al reported 2 cases of intracapsular hemorrhage in pseudoexfoliation patients after an uncomplicated gonioscopy-assisted transluminal trabeculotomy combined with phacoemulsification surgery, where hemorrhage was cleared by IOL extraction–anterior vitrectomy in one case with intraoperative IOL subluxation and by YAG-laser capsulotomy in the other.(5)
In our patient, YAG-capsulotomy was considered to clear the intracapsular hemorrhage; however, given our patient’s limited visual prognosis in the left eye because of advanced glaucoma, it was not recommended.
This case highlights the importance of single-piece IOL-related in-the-bag UGH syndrome as a rare but potentially serious complication after uneventful cataract surgery, especially in pseudoexfoliation patients.
Literature Search
PubMed was searched on April 15, 2019, without date restriction, for English-language articles, using the following terms: uveitis-glaucoma-hyphema syndrome, in-the-bag intraocular lens, pseudoexfoliation, and intracapsular hemorrhage. | | | References | 1. Ellingson FT. The uveitis-glaucoma-hyphema syndrome associated with the Mark VIII anterior chamber lens implant. J Am Intraocul Implant Soc 1978;4:50-3.
2. Zhang L, Hood CT, Vrabec JP, Cullen AL, Parrish EA, Moroi SE. Mechanisms for in-the-bag uveitis-glaucoma-hyphema syndrome. J Cataract Refract Surg 2014;40:490-2.
3. Badakere SV, Senthil S, Turaga K, Garg P. Uveitis-glaucoma-hyphaema syndrome with in-the-bag placement of intraocular lens. BMJ Case Rep 2016;2016:bcr2015213745.
4. Sousa DC, Leal I, Faria MY, Pinto LA. A rare manifestation of uveitis-glaucoma-hyphema syndrome. J Curr Glaucoma Pract 2016;10:76-8.
5. Yalinbas D, Aktas Z, Hepsen İ, Dilekmen N. An unusual complication of combined gonioscopy-assisted transluminal trabeculotomy and phacoemulsification: vision loss due to intracapsular hematoma. Int Ophthalmol 2018;38:2223-6. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in