|
|
 |
 |
 |
 |
|
|
Yoga-induced uveitis glaucoma hyphema syndrome
Digital Journal of Ophthalmology
2020
Volume 26, Number 4
December 20, 2020
DOI: 10.5693/djo.02.2020.11.001
|
Printer Friendly
Download PDF |
|
|



Danny Mammo, MD | Department of Ophthalmology & Visual Neurosciences, University of Minnesota, Minneapolis Michael A. Page, MD | Department of Ophthalmology & Visual Neurosciences, University of Minnesota, Minneapolis Joshua H. Olson, MD | Department of Ophthalmology & Visual Neurosciences, University of Minnesota, Minneapolis
|
|
|
| Abstract | | A 74-year-old pseudophakic white woman with pseudoexfoliation syndrome presented with right eye pain and photophobia and was found to have pseudophacodenesis with recurrent episodes of anterior uveitis, microhyphema, and elevated intraocular pressure (IOP). All episodes occurred after yoga sessions with intensive facedown postures. Ultrasound biomicroscopy (UBM) performed in supine and prone positions demonstrated significant change in the lens-bag complex position, with lens-iris touch. The patient underwent intraocular lens (IOL) explantation, anterior vitrectomy, and flanged intrascleral haptic-fixated IOL placement via double-needle technique, with resolution of all symptoms. | | | Introduction | | Uveitis-glaucoma-hyphema (UGH) syndrome is caused by uveal chafing from intraocular lens (IOL) implants. Most commonly, anterior chamber IOLs (ACIOLs) are the culprit; however, sulcus and posterior chamber IOLs (PCIOLs) can also cause UGH syndrome, with the resulting symptoms of eye pain, photophobia, and vision loss. These symptoms are induced by any combination of anterior segment inflammation, cystoid macular edema, hyphema, iris neovascularization, and optic nerve damage. UGH syndrome can manifest itself immediately after cataract surgery or years afterward. Less than 10% of patients with UGH syndrome display all clinical manifestations, making the diagnosis difficult in many patients.(1) Diagnosis is often remarkably delayed and comes only after multiple examinations from various eye care providers. One retrospective study found a mean of 1,970 days from the time of cataract surgery to diagnosis in patients with UGH syndrome and an ACIOL and 753 days for patients with either sulcus or PCIOLs (Cheung AY, ASCRS Annual Meeting, 2016). Our report highlights the importance of careful history and the relevance of ancillary imaging in the diagnosis of UGH syndrome. | | | Case Report | A 74-year-old white, pseudophakic, woman presented to the Department of Ophthalmology, University of Minnesota, with right eye pain and photophobia 3 years after uncomplicated cataract surgery in this eye. She had an ocular history of pseudoexfoliation syndrome (without glaucoma). Her past medical history and review of systems were unremarkable. Examination revealed anterior uveitis, elevated intraocular pressure (IOP), a single-piece IOL in the capsular bag, pseudophacodenesis, microhyphema, and no iris transillumination deficits. She was managed medically with topical steroids and IOP-lowering medications; however, over the next 2 years she experienced at least four similar recurrences. A thorough infectious and inflammatory uveitis work-up was unremarkable. Visual acuity dropped from 20/20 to 20/40 during flares, and IOP rose to 28–32 mm Hg.
On detailed questioning, the patient recalled that all episodes occurred after yoga sessions with intensive facedown postures. Ultrasound biomicroscopy performed in supine (Figure 1A) and prone (Figure 1B) positions demonstrated significant change in the lens-bag complex position. Lens-iris touch was noted in the prone position. Optical coherence tomography through the macula revealed no evidence of cystoid macular edema. The patient underwent IOL explantation, anterior vitrectomy, and flanged intrascleral haptic fixation of a three-piece IOL (CT Lucia 602; Zeiss, Oberkochen, German) using a double-needle technique.
At 1 year after surgery, the patient experienced no further recurrences and had 20/20 visual acuity and normal IOP. Repeat UBM demonstrated no iris chafing in supine (Figure 1C) or prone (Figure 1D) positions.
| |
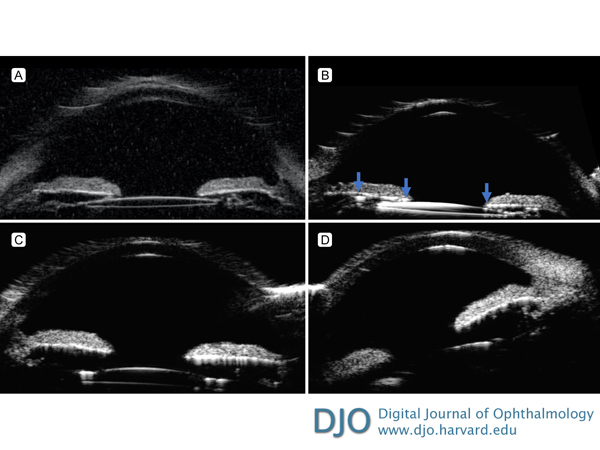
Figure 1
A-B, Ultrasound biomicroscopy (UBM) performed in supine (A) and prone (B) positions showing significant change in the lens-bag complex position. Lens-iris touch was noted in the prone position (arrows). C-D, Repeat UBM 1 year postoperatively showing no iris chafing in supine (C) or prone (D) positions.
|
|
| Discussion | UGH syndrome, caused by malposition of an IOL, creates mechanical trauma to the iris, ciliary body, or iridocorneal angle. This trauma may lead to anterior chamber inflammation, microhyphema, iris transillumination defects, and pigmentary dispersion, with resultant rise in IOP. Chronic inflammation can lead to iris neovascularization and cystoid macular edema.(1)
Originally reported to occur with anterior chamber IOLs, UGH syndrome also occurs with iris-fixated lenses and even posterior chamber IOLs. Although much less common, malpositioned in-the-bag IOLs, which are commonly associated with both high myopia and intraocular complications at the time of cataract surgery, may also result in UGH syndrome.(2) Our patient was only mildly myopic (spherical equivalent, −1.50); however, she did have pseudoexfoliation syndrome, which is a common cause of phaco- and pseudophacodenesis.(3)
While UGH syndrome with an in-the-bag lens and pseudoexfoliation is rare, our patient had a significant lifestyle risk factor in her practice of yoga, which involved exercises with intensive facedown positioning. Ancillary imaging with UBM in the supine and prone positioning supported our suspicion of recurrent IOL-induced iris trauma in this case. Using UBM in the prone and supine positions has only been described once before in the diagnosis of UGH syndrome.(4) At first, our patient decided to minimize her yoga routine, taper off topical steroids, and manage her IOP with topical IOP-lowering agents. However, due to her active lifestyle, she continued having recurrences whenever she resumed yoga. She eventually elected to proceed with IOL explantation and a secondary scleral-fixated IOL procedure. UBM postoperatively revealed a stable IOL-bag complex, and the patient has experienced no recurrences at the time of her most recent follow-up.
Literature Search
PubMed was searched on March 15, 2020, for English-language results using the following terms and combinations: uveitis, glaucoma, hyphema syndrome, UGH syndrome, yoga AND uveitis, yoga AND glaucoma, yoga AND UGH syndrome, exercise AND uveitis, exercise AND UGH syndrome. | | | References | 1. Zemba M, Camburu G. Uveitis-glaucoma-hyphaema syndrome. General review. Rom J Ophthalmol 2017;61:11-17.
2. Lin CJ, Tan CY, Lin SY, Jou JR. Uveitis-glaucoma-hyphaema syndrome caused by posterior chamber intraocular lens—a rare complication in pediatric cataract surgery. Ann Ophthalmology 2008;40:183-4.
3. Jofe MA. Detection of lens subluxation in pseudoexfoliation. Arch Ophthalmol 1988;106:1032.
4. Wu N, Zhang H, Chen B, Ding W. A novel application of B-ultrasonography at various head positions in the diagnosis of untypical uveitis-glaucoma-hyphema (UGH) syndrome: a case report. Medicine (Baltimore) 2019;98:e13891.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in