|
|
 |
 |
 |
 |
|
|
A microbubble of gas as an early indication of macular hole formation after vitrectomy surgery for retinal detachment repair
Digital Journal of Ophthalmology
2017
Volume 23, Number 3
September 3, 2017
DOI: 10.5693/djo.02.2017.04.002
|
Printer Friendly
Download PDF |
|
|


 Alexander Melamud, MD
Alexander Melamud, MD | The Retina Group of Washington, Fairfax, Virginia Dionysios Koroulakis, BS | Georgetown University School of Medicine, Washington, DC Ferdinand Rodriguez-Agramonte, MD | Medstar Washington Hospital Center / Georgetown University Hospital, Washington, DC
|
|
|
| Abstract | | We present a novel case of a 67-year-old man who developed a full-thickness macular hole in the presence of a microbubble after repair of rhegmatogenous retinal detachment. | | | Introduction | A microbubble of gas discovered trapped in a macular hole during postoperative recovery is an unusual clinical presentation described in three previous cases associated with macular hole repair surgery.(1-3) In these previous cases, it was hypothesized that the presence of the microbubble may have prevented successful macular hole closure after the first attempted surgical repair.(1-3) Often, failed initial closure may be attributed to residual traction because of the incomplete removal of epiretinal membranes or the internal limiting membrane.(4)
We present the first case of a microbubble of gas in the macula after rhegmatogenous retinal detachment repair associated with the de novo formation of a macular hole. We also offer a quantitative hypothesis to explain the factors that could possibly lead to the formation of this microbubble.
| | | Case Report | A 67-year-old pseudophakic man presented to the Retina Group of Washington clinic with a complaint of a shadow in the peripheral vision of the left eye. The patient’s past ocular history was notable for macula-involving rhegmatogenous retinal detachment following pars plana vitrectomy (PPV) several years prior to presentation. On examination, visual acuity was 20/60 in the left eye. Dilated fundus examination revealed a nasal, macula-sparing, rhegmatogenous retinal detachment (RRD), macular pucker, and a pseudohole. Optical coherence tomography (OCT) performed prior to the repair of this newly found retinal detachment showed evidence of a pseudohole (Figure 1). Surgery was performed with PPV, retinotomy, endodrainage, air fluid exchange, and 14% perfluoropropane (C3F8) gas infusion. The patient was instructed to maintain 3 days of postoperative positioning, alternating between lying face down and on the left side. At the 1-month postoperative visit, ophthalmoscopy revealed a microbubble in the macula of the left eye (Figure 2). OCT 2 months after surgery revealed a gas microbubble causing a shadowing effect in the fovea (Figure 3). At 10 weeks postoperatively, OCT showed a full-thickness macular hole (Figure 4). Visual acuity was 20/200 in the left eye.
Two and a half months after the nasal retinal detachment repair the patient underwent repeat PPV with membrane peeling and intraocular gas (15% C3F8) to repair the macular hole. Surgical repair was successful, as evidenced by OCT (Figure 5) at 1 year after retinal detachment repair. The patient’s visual acuity in the left eye stabilized at 20/30 | |
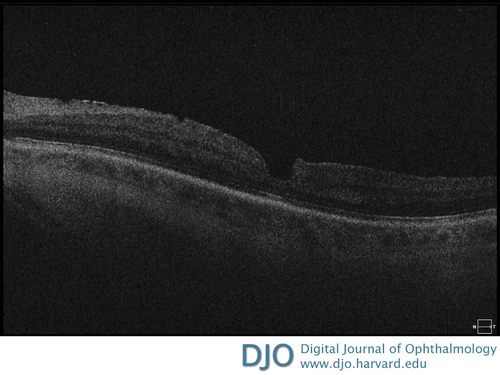
Figure 1
Optical coherence tomographic (OCT) image prior to repair of nasal retinal detachment showing a macular pseudohole prior to vitrectomy but absence of a full-thickness macular hole.
|
|

Figure 2
Fundus photograph 1 month after surgery showing a microbubble in the fovea. The C3F8 and aqueous interface is reflecting the optic nerve and macula in the upper part of the image.
|
|
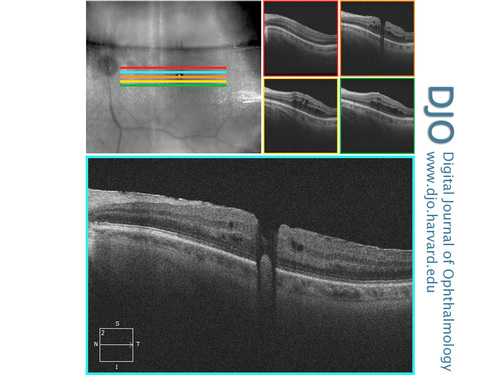
Figure 3
High-definition OCT image of the macula 2 months after surgery focusing on the gas microbubble in the fovea.
|
|
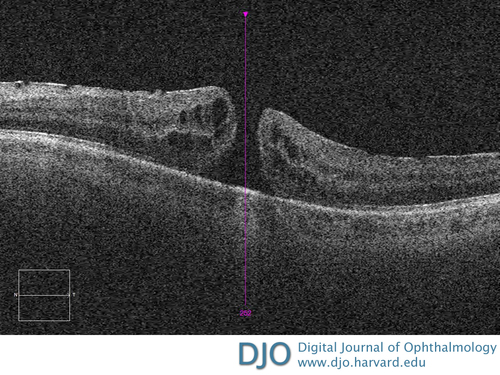
Figure 4
OCT image of the macula 10 weeks after surgery showing a full-thickness macular hole. Nasal hyperreflectivity is noted in the inner retinal layers in the presence of an epiretinal membrane.
|
|
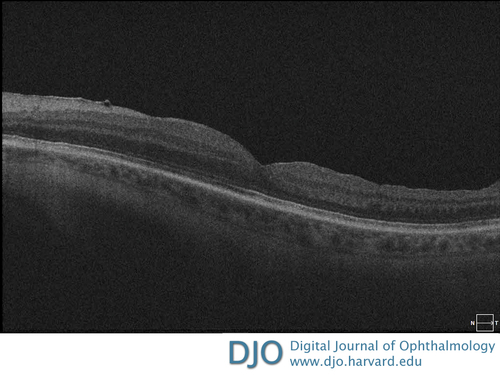
Figure 5
OCT 9.5 months after retinal detachment repair showing evidence of successful surgical outcome. Patient’s vision at this time was 20/30.
|
|
| Discussion | The sequestration of a microbubble of gas within a retinal cavity after PPV is very rare.(1,2) To speculate on the cause(s), it is useful to review the physics of a two-phase system, such as the vitreous cavity with gas and liquid phases. During the demixing of two-phase emulsion, a system will undergo flocculation (bunching of bubbles), followed by coalescence (merging of bubbles) until complete phase separation is achieved.(5) In cases where a microbubble persists, we postulate that the energetically favored decrease in free energy leading to coalescence is prohibited by geometric restrictions of the particular system, which stabilize the two-bubble system. For a system of two bubbles separated by a thin film, the decrease in free energy of the formation of the semiequilibrium interdroplet film is given by the equation
ΔF = 2γo/w (1 – cosθ),
where γo/w is the interfacial tension between the continuous phase of the film and the droplets, and θ denotes the contact angle between the bubbles.(5) Decreased free energy causes a thinning of the interdroplet film, which becomes destabilized, or coalesces, once a critical thinness is breached.(5) Thus, the two variables that contribute to thin film stability are interfacial (surface) tension and the contact angle. It is known that the surface tension of the perfluoropropane and aqueous fluid interface is substantial and favors the usual coalescence of gas bubbles.(6,7) Therefore, the only other variable that can account for the stabilization of the thin film is a fixed contact angle between the two bubbles, preventing the thinning and destabilization of the film.(5) The geometric boundaries facilitating such a setup with a fixed contact angle could be a particular macular hole diameter, depth, or diameter:depth ratio. Therefore, if a macular hole (full thickness, lamellar, or pseudohole) were present, this would help maintain a fixed contact angle, which in turn would stabilize the thin film and prevent the microbubble from coalescing with the primary gas bubble.
Whereas in previously reported cases it has been hypothesized that the microbubble may have supported the persistence of the macular hole after attempted repair, in our case the relationship is more likely the opposite.(1-3) Given the fragility of the film barrier that separates a microbubble from the large gas bubble in the eye, it is very unlikely that the small bubble exerted enough mechanical force against the adjacent retinal tissue to cause macular hole formation. If this much force was possible, it is more likely that the microbubble would have coalesced with the larger bubble. We believe that it is more plausible that the formation of the macular hole in this case was related to traction exerted by the epiretinal membrane and further aided by the presence of the preexisting pseudohole. The geometry of the formed macular hole then facilitated the existence of the microbubble.
To our knowledge, this is the first reported case of a microbubble as an early sign of macular hole formation after nonmacular hole repair vitrectomy surgery. The visualization of a microbubble in the macula of a patient recovering from vitrectomy surgery suggests that an underlying macular hole is present. Early surgical intervention may be considered in such cases to facilitate closure of the macular hole and speed visual recovery. Of note, in the three previously reported cases of microbubble as well as in our case 12%-16% perfluoropropane was used for the repair. Further understanding of the physics in a two-phase system and its applications in retinal surgery will help to elucidate whether more factors play a role in the microbubble formation in these cases where perfluoropropane was used.
Literature Search
PubMed (1970-present) was searched for English-language results on January 15, 2017, using the terms gas microbubble and retinal microbubble. No publications were found with cases of de novo macular hole formation with microbubble after pars plana vitrectomy for rhegmatogenous retinal detachment repair. | | | References | 1. Tatlipinar S, Yenerel NM. Microbubble in the hole: a rare cause of failed macular hole surgery? Retin Cases Brief Rep 2013;7:150-1.
2. Chow DR, Hassan T. Microbubble retention and failed macular hole surgery. Ophthalmic Surg Lasers 2001;32:243-4.
3. Kim J, Lee GH, Lee SW. A case of failed macular hole closure associated with an entrapped microbubble in the hole. J Korean Ophthalmol Soc 2016;57:853-6.
4. Welch M, De Souza SA. Silicone oil microbubble found in failed full-thickness macular hole closure. Retin Cases Brief Rep 2014;8:132-4.
5. Friberg S., Yang J. Emulsion stability. In: Sjoblom J., ed. Emulsions and Emulsion Stability. Surfactant Science Series V. 61. New York, NY: Marcel Dekker; 1996:1-8.
6. de Juan E, McCuen B, Tiedeman J. Intraocular tamponade and surface tension. Surv Ophthalmol 1085;30:47-51.
7. Shaheeda M, Lai TY. Intraocular gas in vitreoretinal surgery. Hong Kong J Ophthalmol 2010;14:8-13.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in