|
|
 |
 |
 |
 |
|
|
Orbital leiomyosarcoma metastasis presenting prior to diagnosis of the primary tumor
Digital Journal of Ophthalmology
2017
Volume 23, Number 4
December 31, 2017
DOI: 10.5693/djo.02.2017.02.004
|
Printer Friendly
Download PDF |
|
|



Nailyn Rasool, MD, FRCPC | Edward Harkness Eye Institute, Columbia University. New York Daniel R. Lefebvre, MD | Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, Boston, Massachusetts Mark A. Latina, MD | Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, Boston, Massachusetts Ian F. Dunn, MD | Department of Neurosurgery. Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts Sandro Santagata, MD, PhD | Department of Pathology, Brigham and Women’s Hospital, Harvard Medical School. Boston, Massachusetts Suzanne K. Freitag, MD | Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, Boston, Massachusetts Dean M. Cestari, MD | Department of Ophthalmology, Massachusetts Eye and Ear, Harvard Medical School, Boston, Massachusetts
|
|
|
| Abstract | | Leiomyosarcomas, neoplasms of smooth muscle, are rarely found within the orbit. Orbital leiomyosarcoma may be primary, metastatic, or secondary to radiation. When they are metastatic, patients almost exclusively have a history of a primary leiomyosarcoma, often occurring in the spermatic cord, skin, gastrointestinal tract, or the uterus. We present the case of 48-year-old woman who presented with a metastatic orbital leiomyosarcoma, which was identified before the primary tumor. | | | Case Report | A 48-year-old woman with a history of primary open-angle glaucoma presented at Massachusetts Eye and Ear with binocular, horizontal diplopia, intermittent left retrobulbar pain, and mild discomfort of the left eye with eye movement. The patient complained of a 4-month history of hypoesthesia of the left cheek, which she associated to apparent nerve injury from ipsilateral injection of a local anesthetic for a root canal performed just prior to onset of symptoms. The patient’s visual acuity was 20/15 in each eye, with slight dyschromatopsia in both eyes. She had a superior arcuate visual field defect in the left eye secondary to glaucoma (Figure 1A). There was 1 mm of proptosis and limitation of abduction of the left eye resulting in an incomitant esotropia larger in left gaze. Magnetic resonance imaging (MRI) demonstrated a well circumscribed lesion in the left orbital apex that appeared inseparable from the left lateral rectus muscle; the lesion enhanced slightly less than muscle, with more prominent enhancement of the rim of the lesion (Figure 2).
Given that the lesion appeared intrinsic to the extraocular muscle, a common site to harbor an orbital metastasis, the patient underwent a systemic work-up searching for an occult primary malignancy. An 18-fluorodeoxyglucose positron emission tomography (18-FDG PET) scan showed a right lower quadrant mass that was lobulated and heterogeneously enhancing with 18-FDG avidity in the pelvis demonstrating its hypermetabolic nature (Figure 3).
A radiologically guided core needle biopsy was performed of the mass. The pathology demonstrated eosinophilic spindle-shaped cells with elongated nuclei, scattered mitotic figures, and areas of ischemic degeneration. The lesion stained positive for both desmin and smooth muscle actin, in keeping with a malignant smooth muscle neoplasm, specifically a leiomyosarcoma (Figure 4). Systemic chemotherapy was being considered for management of her metastatic disease when the patient developed worsening retrobulbar pain (2 months after initial presentation). On examination, her visual acuity was reduced to 20/25, and there was notable worsening of the dyschromatopsia and visual field defect in the left eye (Figure 1B). In addition, she had further limitation of abduction of the left eye. Repeat MRI scan demonstrated enlargement of the lesion, with compression of the left optic nerve laterally (Figure 5). In order to relieve the patient’s pain, preserve her vision, and remove the only identified metastasis, the patient underwent excision of the lesion, with care taken not to disrupt the lateral rectus muscle by using a cranio-orbital-zygomatic approach (Figure 6). The pathology was consistent with a leiomyosarcoma metastasis. The patient’s visual acuity returned to baseline, her visual field defect resolved, and she had no residual motility deficit after removal of the lesion. Postoperatively the patient underwent adjuvant fractionated radiotherapy. There has been no orbital recurrence with 18 months’ follow-up. The patient subsequently underwent a total abdominal hysterectomy and partial colectomy to remove the abdominal mass followed by chemotherapy. | |
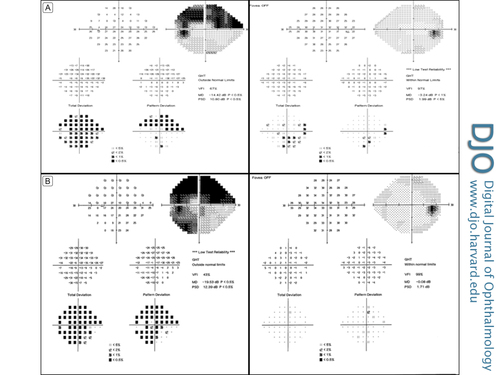
Figure 1
A, Patient’s initial visual field, with a full visual field in the right eye and a superior arcuate defect in the left eye resulting from her underlying glaucoma. B, Worsening of the visual field in the left eye, with a more significant superior visual field defect extending to the inferotemporal region.
|
|
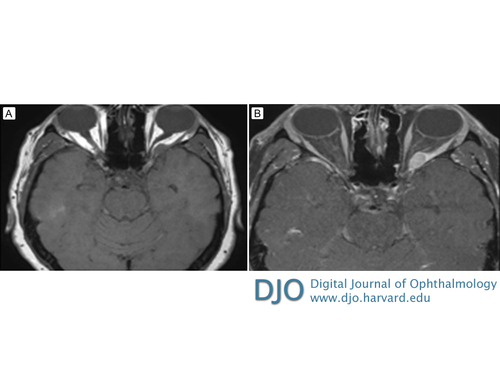
Figure 2
The figure demonstrates axial magnetic resonance imaging T1-weighted pre- (A) and post-contrast (B) images showing a well circumscribed lesion in the left orbital apex that diffusely enhances but with prominent rim enhancement; the lesion is inseparable from the left lateral rectus muscle.
|
|
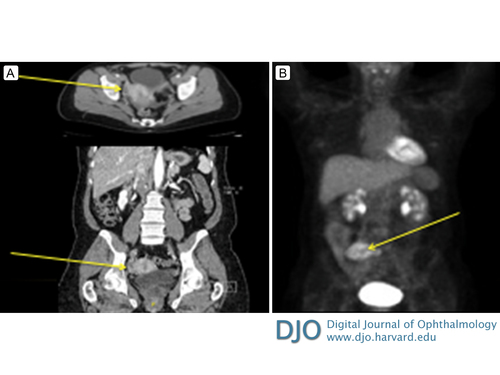
Figure 3
Computed tomography (A) and 18-fluorodeoxyglucose positron emission tomography (18-FDG PET; B) showing findings of the uterine leiomyosarcoma. There is an 8.5 cm heterogeneously enhancing lesion in the right lower quadrant with hypermetabolic activity as noted by the avidity of 18-FDG to the tumor.
|
|
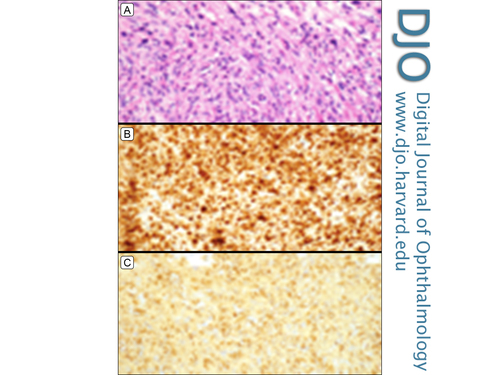
Figure 4
On hematoxylin and eosin stained sections, the pathology of the uterine tumor demonstrated spindle-shaped cells with eosinophilic cytoplasm and elongated, cigar-shaped nuclei with mitotic figures and areas of ischemic degeneration (A). The lesion was immunopositive for desmin (B) and smooth muscle actin (C), in keeping with a leiomyosarcoma. Original magnification ×400.
|
|
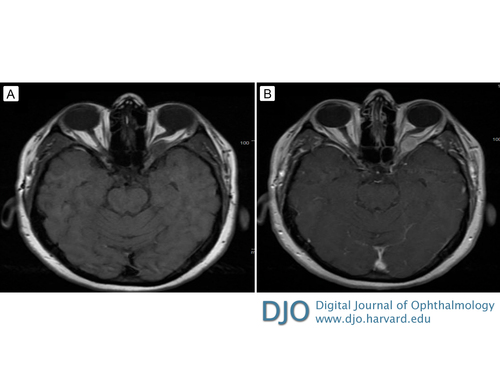
Figure 5
T1-weighted pre- (A) and postcontrast (B) magnetic resonance imaging (MRI) demonstrating interval enlargement of the orbital lesion with compression of the left optic nerve.
|
|

Figure 6
A, Orbital apex periorbita (*) exposed in a cranio-orbitozygomatic approach; the frontal lobe dura (F) and temporal dura (T) are noted beneath cottonoids. B, Periorbita is open and the lateral rectus (LR) reflected, showing the tumor (arrow). C, After resection of the tumor. D, T1-weighted post-gadolinium MRI 2 months after surgery showing no evidence of residual or recurrent tumor.
|
|
| Discussion | To our knowledge, this is the report the first metastatic orbital leiomyosarcoma presenting without prior identification of the primary tumor. Leiomyosarcomas can present as primary or metastatic orbital tumors or as secondary tumors after prior radiation therapy (as seen in patients with a history of retinoblastoma).(1) Most primary cases of leiomyosarcoma occur in the posterior orbit; however, anterior, lacrimal gland, and even conjunctival cases have been described.(2-4) The primary orbital tumors are thought to originate in primitive replicating cells associated with blood vessels in the posterior orbit and possibly Mueller’s muscle when present in the anterior orbit. In metastatic lesions, the primary tumors are often pelvic, cutaneous, or gastrointestinal in origin. All metastatic cases in the literature have had a known primary, previously diagnosed months to years before the development of orbital symptoms, with subsequent identification of the metastasis.
The typical presenting signs of metastatic orbital leiomyosarcomas include progressive proptosis, optic neuropathy, and eye movement abnormalities. Primary orbital leiomyosarcomas are isointense to extraocular muscle tissue and cerebral gray matter on MRI T1-weighted sequences, with notable peripheral rim enhancement.(5) However, Voros et al noted that metastatic orbital leiomyosarcomas may demonstrate more diffuse enhancement.(6) Our case presented with a lesion that radiographically appeared intrinsic to the extraocular muscle with both diffuse enhancement of the lesion but also with recognizable rim enhancement.
Pathologically, the lesion may be encapsulated and well demarcated, nonencapsulated, or incompletely encapsulated and invading nearby structures.(6-9) They are relatively insensitive to chemotherapy and radiation; wide surgical excision is often recommended. Some advocate exenteration, given the aggressive nature of the tumor.(9) The use of adjuvant chemotherapy and radiotherapy particularly for metastatic disease has demonstrated limited benefit.(10)
Although our patient had no history of malignancy, the presentation of the lesion being indistinguishable from the extraocular muscle prompted a systemic work-up and identification of the patient’s uterine malignancy. It is important for clinicians to know that orbital lesions intrinsic to extraocular muscles may be metastatic malignant lesions and a systemic work-up is indicated to rule out a distant primary tumor.
Literature Search
PubMed was searched on April 3, 2016, without date restriction, for English-language articles, using the following terms singly and in combination: orbital leiomyosarcoma, leiomyosarcoma metastases, optic neuropathy, and orbital leiomyosarcoma imaging. The reference lists of all relevant articles were also searched. | | | References | 1. Folberg R, Cleasby G, Flanagan JA, Spencer WH, Zimmerman LE. Orbital leiomyosarcoma after radiation therapy for bilateral retinoblastoma. Arch Ophthalmol 1983;101:1562-5.
2. Guerriero S, Sborgia A, Giancipoli G, Fiore MG, Ross R, Piscitelli D. A rare case of primitive epithelioid leiomyosarcoma of the conjunctiva. Orbit 2011;30:169-71.
3. White VA, Damji KF, Richards JS, Rootman J. Leiomyosarcoma of the conjunctiva. Ophthalmology 1991;98:1560-4.
4. Yeniad B, Tuncer S, Peksayar G, Mete O, Minareci O. Primary orbital leiomyosarcoma. Ophthal Plast Reconstr Surg 2009;25:154-5.
5. Hou LC, Murphy MA, Tung GA. Primary orbital leiomyosarcoma: a case report with MRI findings. Am J Ophthalmol 2003;135:408-10.
6. Voros GM, Birchall D, Ressiniotis T, Neoh C, Owen RI, Strong NP. Imaging of metastatic orbital leiomyosarcoma. Ophthal Plast Reconstr Surg 2005;21:453-5.
7. Bakri SJ, Krohel GB, Peters GB, Farber MG. Spermatic cord leiomyosarcoma metastatic to the orbit. Am J Ophthalmol. 2003;136:213-5.
8. Kaltreider SA, Destro M, Lemke BN. Leiomyosarcoma of the orbit: a case report and review of the literature. Ophthal Plast Reconstr Surg 1987;3:35-41.
9. Jakobiec FA, Howard GM, Rosen M, Wolff M. Leiomyoma and leiomyosarcoma of the orbit. Am J Ophthalmol 1975;80:1028-42.
10. Chen J, Wei R, Ma X. Orbital metastasis of retroperitoneal leiomyosarcoma. Med Oncol 2012;29:392-5.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in