|
|
 |
 |
 |
 |
|
|
Treatment of Takayasu arteritis–related photic and postprandial amaurosis
Digital Journal of Ophthalmology
2017
Volume 23, Number 4
October 28, 2017
DOI: 10.5693/djo.02.2017.09.002
|
Printer Friendly
Download PDF |
|
|



Sze H. Wong, MD | Institute of Ophthalmology & Visual Science, Rutgers New Jersey Medical School, Newark Roger E. Turbin, MD, FACS | Institute of Ophthalmology & Visual Science, Rutgers New Jersey Medical School, Newark Larry P. Frohman, MD | Institute of Ophthalmology & Visual Science, Rutgers New Jersey Medical School, Newark
|
|
|
| Abstract | | We report the case of a 66-year-old man with Takayasu arteritis who developed photic and postprandial amaurosis occurring at a corticosteroid dose <40 mg per day, despite concurrent methotrexate. The amaurosis resolved with correction of anemia by packed red blood cell transfusion. Marginal retinal perfusion in Takayasu arteritis may precipitate symptomatic hypoxia as a result of eating a meal or exposing the eye to bright lights. Correction of anemia improves oxygen delivery to the hypoxic retina and relieves recurrent amaurosis. | | | Introduction | | Takayasu arteritis (TA) is a granulomatous vasculitis of large vessels, commonly affecting the aortic arch and its branches, that may cause ocular ischemic syndrome, ischemic optic neuropathy, or retinal ischemia.(1) Vertebrobasilar disease may cause amaurosis induced by neck extension. We present a unique case of TA with vision changes that occurred after the patient consumed food or looked at bright light. | | | Case Report | A 66-year-old white man presented with a 3-month history of painless, bilateral visual disturbance described as colors dimming after exposure to bright sunlight or prolonged viewing of his computer monitor. Similar loss occurred repeatedly 30 minutes after eating. His vision would return to its previous state after closing his eyes for 30 minutes.
He was treated for hypertension (hydralazine, amlodipine, carvedilol, lisinopril, hydrochlorothiazide, clonidine patch) and hypercholesterolemia (atorvastatin), and had been diagnosed with polymyalgia rheumatica (received corticosteroids 9 years previously). He had radiation seed implantation for local prostate cancer 1 year prior to presentation.
TA was diagnosed 3 years earlier by a vascular surgeon who noted absent upper extremity pulses. Magnetic resonance angiogram revealed diffuse narrowing of bilateral subclavian and axillary arteries without intracranial or carotid artery involvement.
On neuro-ophthalmologic examination, corrected visual acuity was 20/20 in each eye. A photostress test recovery time was 13 seconds bilaterally. His pupils were equal and reactive to light without relative afferent pupil defect. Intraocular pressures, ocular ductions and alignment, and color vision testing were normal in each eye. No carotid bruits were heard, and the temporal arteries were normal to palpation. Anterior and posterior segment examination was unremarkable.
Intravenous fluorescein angiogram revealed an arm-to-eye time of 18.7 seconds and a 1/3 disc-diameter area of delayed perfusion superior to the superotemporal arcade (Figure 1). Humphrey visual fields (24-2) were within normal limits. Hemoglobin level was 9.3 g/dL (mean corpuscular volume, 100.7 fL).
He received oral prednisone 20 mg daily and oral methotrexate 7.5 mg weekly. His visual symptoms subsided only at prednisone dosage of at least 40 mg daily. Three months later, his hemoglobin level was 7.5 g/dL, attributed to bleeding from hemorrhoids and a duodenal ulcer. After he received a blood transfusion, increasing the level to 10.1 g/dL, he no longer experienced amaurosis even after prednisone was tapered to 5 mg daily, except for one instance when his hemoglobin dropped to 8.7 g/dL. | |
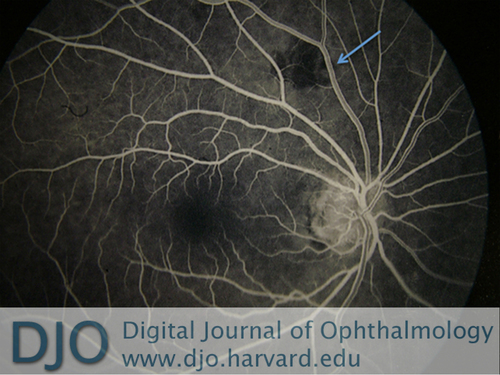
Figure 1
Intravenous fluorescein angiogram (arteriovenous phase) in the setting of Takayasu arteritis–induced amaurosis. The arrow points to an area of delayed perfusion. (The C-shaped black line superotemporal to the macula is an artifact.)
|
|
| Discussion | Our patient’s postprandial and photic amaurosis were signs of hypoxia of the retina. Postprandial blood flow to the gastrointestinal tract may triple, with the diversion reducing ocular perfusion.(2) Photic amaurosis occurred when increased metabolic demand in the retina exceeded our patient’s ability to oxygenate his retina through circulation compromised by sequelae of vasculitis.
Postprandial and photic amaurosis are typically symptoms of carotid artery atherosclerosis effectively treated with endarterectomies.(3-6) However, our patient did not have internal carotid artery stenosis. Decreased eye perfusion was likely due to proximal occlusion near the aortic arch. His symptoms resolved whenever his prednisone dose was titrated up, indicating that arteritis was partially responsible for his visual disturbances. TA-induced amaurosis can be successfully treated with corticosteroids and methotrexate.(7) However, prednisone and methotrexate use in our patient’s case may have exacerbated his anemia caused by hemorrhoids and a duodenal ulcer. Although our patient had been placed on iron and folate supplementation, it was not until he received a blood transfusion that his symptoms subsided. The transfusion maintained his hemoglobin level at approximately 10 mg/dL and allowed tapering of prednisone without symptom recurrence.
In a patient with TA presenting with postprandial and/or photic amaurosis, treating the etiology of the problem with immunosuppressant treatments, while optimizing oxygenation to the eye with blood transfusions may alleviate the visual symptoms.
Literature Search
PubMed was searched on August 22, 2015, for English-language articles using the following terms: Takayasu arteritis; Takayasu arteritis AND amaurosis; photic amaurosis; light-induced amaurosis; and postprandial amaurosis. | | | References | 1. Peter J, David S, Danda D, Peter JV, Horo S, Joseph G. Ocular manifestations of Takayasu arteritis: a cross-sectional study. Retina 2011;31:1170-8.
2. Gatt M, MacFie J, Anderson AD, et al. Changes in superior mesenteric artery blood flow after oral, enteral, and parenteral feeding in humans. Crit Care Med 2009;37:171-6.
3. Levin LA, Mootha VV. Postprandial transient visual loss: a symptom of critical carotid stenosis. Ophthalmology 1997;104:397-401.
4. Shin YW, Kim JM, Jung KH, et al. Light-induced amaurosis fugax due to severe distal internal carotid artery stenosis: in view of managing ocular ischemic syndrome. J Neurol 2013;260:1655-7.
5. Kaiboriboon K, Piriyawat P, Selhorst JB. Light-induced amaurosis fugax. Am J Ophthalmol 2001;131:674-6.
6. Pantin CF, Young RA. Postprandial blindness. Br Med J 1980;281:1686.
7. Rocci CA, Ferrera PC. Takayasu arteritis presenting as amaurosis fugax in a man. Am J Emerg Med 1998;16:185-7.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in