|
|
 |
 |
 |
 |
|
|
Detection of pars plana rupture by ultrasound biomicroscopy after cannula dislodgement during cataract wound hydration
Digital Journal of Ophthalmology
2017
Volume 23, Number 1
February 25, 2017
DOI: 10.5693/djo.02.2016.09.001
|
Printer Friendly
Download PDF |
|
|


 Yoshihiro Yonekawa, MD
Yoshihiro Yonekawa, MD | Massachusetts Eye and Ear Infirmary, Boston, Massachusetts; Boston Children's Hospital, Boston, Massachusetts Benjamin J. Thomas, MD | Florida Retina Institute, Jacksonville, Florida Laurie K. Lau-Sickon, CDOS, ROUB | Beaumont Eye Institute, William Beaumont Hospital, Royal Oak, Michigan Bradley J. Anderson, MD | Beaumont Eye Institute Alan J. Ruby, MD | Beaumont Eye Institute, William Beaumont Hospital, Royal Oak, Michigan; Associated Retinal Consultants, Royal Oak, Michigan
|
|
|
| Abstract | | Ultrasound biomicroscopy (UBM) is a valuable diagnostic modality for imaging anterior ocular structures. Its utility has been well studied in anterior segment, lenticular, and pars plicata pathologies. However, imaging of the pars plana has been seldom described. We present the case of a 66-year-old woman referred for vitreous hemorrhage after expulsive cannula dislodgement into the posterior segment during wound hydration at the end of cataract surgery. B-scan ultrasonography initially detected a very anterior abnormality, but the resolution was insufficient for accurate diagnosis. Subsequent UBM clearly showed rupture of the pars plana and a mild cyclodialysis cleft. To our knowledge, this is the first report of a pars plana rupture detected by ultrasound, which expands the diagnostic capacities and indications for UBM. | | | Introduction | | Ultrasound biomicroscopy (UBM) is an imaging modality that allows high-resolution imaging of anterior ocular structures using very high-frequency ultrasound. Its utility in the anterior segment is well established, but the literature on posterior segment applications beyond the pars plicata is limited. This report demonstrates the utility of high-resolution imaging of the pars plana in a patient referred for a cataract surgery complication that resulted in a focal rupture of the pars plana. | | | Case Report | A 66-year-old woman was undergoing routine phacoemulsification cataract surgery in the left eye. At the end of the procedure, during wound hydration of a temporal clear corneal incision, the cannula dislodged forcefully into the posterior segment. The cannula spontaneously retracted back out of the corneal incision. Vitreous hemorrhage was noted, and the patient was referred to Associated Retinal Consultants, Royal Oak, Michigan, for evaluation.
On examination at our clinic, visual acuity was 20/40 in the right eye and hand motions in the left eye. Intraocular pressure (IOP) in the right eye was 10 mm Hg; in the left eye, 7 mm Hg. Slit-lamp examination revealed diffuse conjunctival injection, corneal stromal edema, Descemet’s folds, and 4+ red blood cells in the anterior chamber. A one-piece intraocular lens (IOL) was well centered in the capsule, but there was a subtle defect in the peripheral capsule in the inferonasal quadrant. There was no view to the posterior segment due to dense vitreous hemorrhage.
Initial B-scan ultrasonography of the left eye showed vitreous hemorrhage and an attached retina. Further focused examination in the inferonasal quadrant revealed an abnormality in the far anterior periphery (Figure 1A). UBM of the same area revealed a full-thickness rupture of the pars plana with intact sclera (Figure 1B). There was fluid tracking anteriorly under the pars plana to form a cyclodialysis cleft to the iris insertion (Figure 1C). No iridodialysis was identified, however. The IOL remained well positioned (Figure 1D). The patient was started on topical steroids and cycloplegia. On repeat UBM 1 week later, the pars plana rupture and cyclodialysis cleft appeared stable. The vitreous hemorrhage, presumably from the pars plana impact site, gradually cleared, and visual acuity improved to 20/25, 7 weeks postoperatively. The IOP also increased to 10 mm Hg.
| |
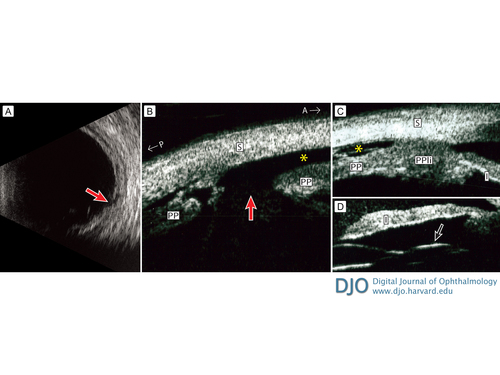
Figure 1
A 66-year-old woman referred for vitreous hemorrhage after cannula dislodgement during cataract surgery wound hydration. A, Transverse B-scan at 7:00 detected a tissue abnormality anteriorly (red arrow). B-C, Ultrasound biomicroscopy revealed rupture of the pars plana (red arrow) and subuveal fluid tracking anteriorly (asterisks) at 7:00. D, The lens haptic remains well-positioned (black arrow). A, anterior; I, iris; P, posterior; PP, pars plana; PPli, pars plicata; S, sclera.
|
|
| Discussion | Ultrasonography uses high-frequency acoustic waves that propagate within a fluid medium.(1) Acoustic pulse reflections occur at tissue boundaries and are returned to the transducer and converted into images. UBM was introduced in the early 1990s.(2) It utilizes frequencies of 35-100 MHz to allow higher-resolution imaging of anterior structures compared to conventional B-scans. As with any ultrasound technology, UBM allows imaging of occult structures visually hindered by normal anatomy (such as the iris) or pathologic states (such as corneal opacities).
Applications of UBM have been well studied in the anterior segment, particularly by glaucoma specialists. It is particularly useful in the imaging of plateau iris,(3) iris and ciliary body cysts(4) and tumors,(5) cyclodialysis clefts,(6) IOL positioning,(7) and capsular anatomy.(8) However, UBM in the vitreoretinal literature has been limited, in part because the high frequency of the UBM acoustic waves provides superior resolution of anterior structures, but the wavelengths become quickly attenuated and lose resolution beyond the pars plana. Early studies showed feasibility in imaging retinoschisis and choroidal thickening in inflammatory and effusive processes.(9) In Japan, where retinal detachment related to atopic dermatitis is well described, UBM has been used to image detachment of the nonpigmented ciliary epithelium (which is contiguous with the neurosensory retina) in such patients.(10,11) UBM is also useful in detecting occult intraocular foreign bodies,(12) especially if suspected to be hidden behind the iris or within the zonules. To our knowledge, traumatic tangential rupture of the pars plana, with or without UBM confirmation, has not been previously described.
Isolated trauma of the pars plana without an associated contiguous external penetrating wound is rare and likely underdiagnosed. The pars plana is difficult to examine and detection of pathology requires a high index of suspicion to employ scleral indentation. Even with scleral depression, ophthalmoscopic examination is limited if there is associated vitreous hemorrhage, as in the present case. The diagnosis would have been difficult to make without the UBM. The B-scan was able to detect an abnormality in the area, but the resolution was insufficient to differentiate the lesion from a retinal break or lamellar pars plicata detachment. The accurate diagnosis allowed us to initiate appropriate conservative treatment.
In the present case, the pars plana rupture was caused by iatrogenic cannula dislodgement during cataract surgery, which resulted in the cannula piercing the capsule adjacent to the IOL, striking the pars plana, and causing vitreous hemorrhage. Cannula detachment is a not an uncommon phenomenon, most commonly occurring during wound hydration.(13) Potential complications include retinal damage and vitreous loss.(13,14) The cannula should be tightened by the surgeon after being handed by the assistant, and patency of the cannula should be confirmed prior to use to prevent such adverse events. Luer locking cannulas are appropriate in this context.
Literature Search
PubMed was searched for English-language results on October 13, 2014, using the following terms: pars plana AND ultrasound. | | | References | 1. Yonekawa Y, Sun G, Silverman RH, Coleman DJ, Chan RVP. The role of high-frequency ultrasound in ophthalmic diagnosis. Contemporary Ophthalmology 2009;8:1-8.
2. Pavlin CJ, Harasiewicz K, Foster FS. Ultrasound biomicroscopy of anterior segment structures in normal and glaucomatous eyes. Am J Ophthalmol 1992;113:381-9.
3. Kumar RS, Tantisevi V, Wong MH, et al. Plateau iris in Asian subjects with primary angle closure glaucoma. Arch Ophthalmol 2009;127:1269-72.
4. Augsburger JJ, Affel LL, Benarosh DA. Ultrasound biomicroscopy of cystic lesions of the iris and ciliary body. Trans Am Ophthalmol Soc 1996;94:259-71.
5. Bianciotto C, Shields CL, Guzman JM, et al. Assessment of anterior segment tumors with ultrasound biomicroscopy versus anterior segment optical coherence tomography in 200 cases. Ophthalmology 2011;118:1297-302.
6. Gentile RC, Pavlin CJ, Liebmann JM, et al. Diagnosis of traumatic cyclodialysis by ultrasound biomicroscopy. Ophthalmic Surg Lasers 1996;27:97-105.
7. Piette S, Canlas OA, Tran HV, Ishikawa H, Liebmann JM, Ritch R. Ultrasound biomicroscopy in uveitis-glaucoma-hyphema syndrome. Am J Ophthalmol 2002;133:839-41.
8. Papakostas TD, Yonekawa Y, Chee YE, Qiang XC, Kim IK. Ultrasound biomicroscopy in lens-induced glaucoma. JAMA Ophthalmol 2015;133:112.
9. Gentile RC, Berinstein DM, Liebmann J, et al. High-resolution ultrasound biomicroscopy of the pars plana and peripheral retina. Ophthalmology 1998;105:478-84.
10. Yoshida S, Sasoh M, Arima M, Uji Y. Ultrasound biomicroscopic view of detachment of the ciliary epithelium in retinal detachment with atopic dermatitis. Ophthalmology 1997;104:283-7.
11. Tanaka S, Takeuchi S, Ideta H. Ultrasound biomicroscopy for detection of breaks and detachment of the ciliary epithelium. Am J Ophthalmol 1999;128:466-71.
12. Deramo VA, Shah GK, Baumal CR, et al. Ultrasound biomicroscopy as a tool for detecting and localizing occult foreign bodies after ocular trauma. Ophthalmology 1999;106:301-5.
13. Pandey P, Kirkby G. Cannula detachment during cataract surgery: results of a survey. Can J Ophthalmol 2012;47:280-2.
14. McPherson ZE, Lau OU, Chen TS, et al. High-speed cannula detachment into the eye during hydrodissection. Ophthalmic Surg Lasers Imaging Retina 2014;45:347-9. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in