|
|
 |
 |
 |
 |
|
|
Successful femtosecond LASIK flap creation despite multiple suction losses
Digital Journal of Ophthalmology
2014
Volume 20, Number 1
January 17, 2014
DOI: 10.5693/djo.02.2013.09.006
|
Printer Friendly
|
|
|


 Zeba A. Syed, B.A.
Zeba A. Syed, B.A. | Massachusetts Eye Ear Infirmary, Harvard Medical School, Boston, MA, USA Samir A. Melki, MD, PhD | Massachusetts Eye & Ear Infirmary, Harvard Medical School, Boston, Massachusetts
|
|
|
| Abstract | | We present a case of successful completion of a laser in situ keratomileusis (LASIK) procedure despite 5 episodes of suction loss during femtosecond flap creation in a 30-year-old man with no risk factors. The patient had an uncorrected distance visual acuity of 20/20 in both eyes at his 2-month follow-up visit. Our experience in this case shows that multiple suction losses during femtosecond LASIK flap creation do not preclude completion of a successful procedure with excellent visual outcomes. Caution and technique modification are advised if multiple laser passes are applied to avoid creating multiplanar flaps. | | | Introduction | | Although widely used, laser in situ keratomileusis (LASIK) is associated with various complications. Femtosecond LASIK flap construction can be complicated by loss of suction when the vacuum ring is applied to the ocular globe, leading to an incomplete flap. If suction loss occurs after the femtosecond laser raster has been initiated, the focal plane shifts to the surface of the cornea. The surgeon must interrupt the procedure and a second femtosecond pass may be performed. The vacuum ring is immediately reapplied and flap creation repeated using the same docking cone.(1) We report the successful completion of a LASIK case despite 5 episodes of suction losses during femtosecond flap creation. | | | Case Report | A 30-year-old man underwent bilateral custom LASIK surgery at the Boston Eye Group for the correction of myopia with astigmatism. His preoperative refraction was −6.25 −1.25 × 140 in the right eye and −6.50 −1.00 × 10 in the left eye, with a best-corrected visual acuity of 20/20 in both eyes. Corneal videokeratography using Pentacam (Oculus Inc, Wetzlar, Germany) was normal in both eyes, with keratometry of 46.50/47.00 D at 67° in the right eye and 46.75/47.25 D at 88° in the left eye (Figure 1).
A femtosecond LASIK procedure was planned, with a flap diameter of 9.3 mm and a targeted depth of 90 μm (IntraLase FS 60kHz, Abbott Medical Optics, Santa Ana, CA). Initial surgery on the right eye resulted in an incomplete flap construction due to suction loss occurring at one-third the distance across the planned cut. Two additional episodes of suction loss of the right eye were observed prior to the second laser cut pass. These happened after docking to the Intralase and just prior to the initiation of the laser pass. The second laser pass was interrupted at two-thirds of the distance across the cornea due to another suction loss. The third pass proceeded to one-third the distance of the planned cut before loss of suction. The final pass resulted in complete flap creation (Figure 2). None of the interruptions in the laser pass occurred within the pupillary area. This prompted the surgeon (SAM) to consider further attempts rather than abort the surgery. The suction ring was replaced twice, once after the second suction loss and once prior to the last attempt. Ablation was subsequently performed on both eyes. Intraoperative pachymetry revealed a flap thickness of 87 μm in the right eye, compared to 108 μm in the left eye, in which a single laser pass was conducted. On the first day after surgery, the patient had an uncorrected distance visual acuity of 20/25 in each eye, with LASIK flaps clear and well centered on slit-lamp examination. At his 2-month follow-up visit, uncorrected distance visual acuity was 20/20 in each eye. | |
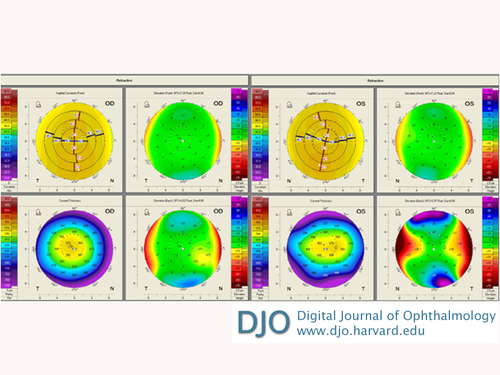
Figure 1
Preoperative Pentacam (Oculus Inc, Wetzlar, Germany) images of both eyes.
|
|
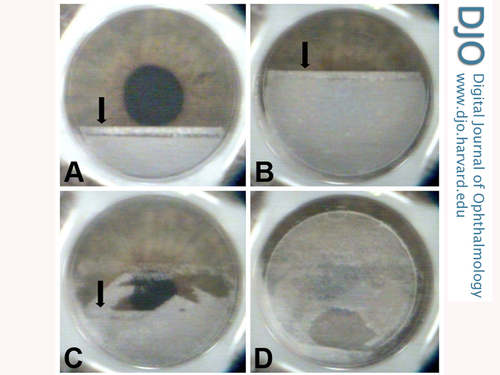
Figure 2
Photographs taken at the moment of suction loss during multiple passes (A-C) and after complete femtosecond flap creation (D). The arrow indicates the location of the raster ablation at the moment of the loss of suction.
|
|
| Discussion | To our knowledge, this is the first report of successfully creating a femtosecond LASIK flap after 5 episodes of suction loss. The exact cause of suction loss during this procedure is unclear. Known factors for such a suction loss include significantly flat keratometric power (K-readings <42.00 D), small palpebral apertures, deep-set eyes, and excessive eyelid squeezing.(2) Our patient had none of these risk factors. Other causes cannot be excluded, such as poor suction ring application technique and patient anxiety resulting in head and globe movement.
Most surgeons elect to proceed with immediate recut after an incomplete femtosecond flap as a result of suction loss. The laser manufacturer recommends replacing the suction ring while reusing the same docking cone to avoid ablation at a different depth. The transient opaque bubble layer pattern remains visible if the suction ring is immediately reapplied, allowing for identification of the border of the first raster pass.(1) Once the vacuum is reapplied and the femtosecond laser activated, the newly created cavitation bubbles percolate toward the previously created lamellar cut. This avoids the creation of multiple ablation planes. Our patient’s visual outcome was consistent with previous studies that reported good visual results after single and multiple passes of the femtosecond laser.(1)
There is only one report in the literature of an uneven transected lamellar cut after immediate second femtosecond laser pass. The second pass resulted in an opacified stromal scar and a loss of 6 lines of best-corrected visual acuity.(3) In contrast to our report and those of others, the second cut was not applied at the same session but rather 5 days later. A study in porcine eyes showed that an immediate second femtosecond laser pass may cause irregular surface and multiple flaps and lead to a free sliver of the corneal stroma.(4) There have been no such reports among humans. In cases where more than one femtosecond laser passes are needed, we recommend initiating flap dissection in the area where a single femtosecond ablation was performed (typically inferiorly). Dissection can then proceed toward the area where multiple ablations were performed to avoid the unlikely possibility of dissecting at multiple planes.
Multiple vacuum applications may not be permissible in certain situations, for example, in patients with glaucoma. There is no evidence of an adverse effect on the retina due to repeated suction application to the globe. One possible approach to an interrupted flap creation is to abort the procedure and perform surface ablation at a later date.(5)
Literature Search
The authors searched PubMed, most recently on January 16, 2014, for reports in English, without date restriction, using the following terms: suction loss LASIK and suction loss femtosecond. | | | References | 1. Muñoz G, Albarrán-Diego C, Ferrer-Blasco T, Javaloy J, García-Lázaro S. Single versus double femtosecond laser pass for incomplete laser in situ keratomileusis flap in contralateral eyes: visual and optical outcomes. J Cataract Refract Surg 2012;38:8-15.
2. Asano-Kato N, Toda I, Hori-Komai Y, Takano Y, Tsubota K. Risk factors for insufficient fixation of microkeratome during laser in situ keratomileusis. J Refract Surg 2002;18:47-50.
3. Liu A, Manche EE. Transected lamellar cut following second pass with a femtosecond laser after incomplete flap construction during laser in situ keratomileusis. J Clinic Experiment Ophthalmol 2012;3:215.
4. Ide T, Yoo SH, Kymionis GD, et al. Second femtosecond laser pass for incomplete laser in situ keratomileusis flaps caused by suction loss. J Cataract Refract Surg 2009;35:153-7.
5. Jabbur NS, Myrowitz E, Wexler JL, O’Brien TP. Outcome of second surgery in LASIK cases aborted due to flap complications. J Cataract Refract Surg 2004;30:993-9.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in