|
|
 |
 |
 |
 |
|
|
Spontaneous resolution of ophthalmologic symptoms following bilateral traumatic carotid cavernous fistulae
Digital Journal of Ophthalmology
2013
Volume 19, Number 2
May 10, 2013
DOI: doi:10.5693/djo.02.2013.02.003
|
Printer Friendly
Download PDF |
|
|


 Briana Gapsis, BS, BA
Briana Gapsis, BS, BA | University of Central Florida College of Medicine, Orlando, Florida Roshni U. Ranjit, BS, BA | Morsani College of Medicine, University of South Florida, Tampa, Florida Sharad Malavade, DNB (Ophth), MPH | USF Eye Institute, Morsani College of Medicine, University of South Florida, Tampa, Florida Andrew Carey, MD | USF Eye Institute, Morsani College of Medicine, University of South Florida, Tampa, Florida Reed Murtagh, MD | University Diagnostic Institute, Tampa, Florida Mitchell D. Drucker, MD | Morsani College of Medicine, University of South Florida, Tampa, Florida; USF Eye Institute, Morsani College of Medicine, University of South Florida, Tampa, Florida Peter R. Pavan, MD | Morsani College of Medicine, University of South Florida, Tampa, Florida; USF Eye Institute, Morsani College of Medicine, University of South Florida, Tampa, Florida
|
|
|
| Abstract | | A 38-year-old woman developed bilateral carotid cavernous fistulae (CCF) following a motor vehicle collision. Her initial ophthalmologic findings included periorbital edema, palsies of the left oculomotor and abducens nerves, and residual dilated pupils. She subsequently developed significant optic disc edema and retinal vascular dilation bilaterally. Patients with similar injuries typically require neurosurgical or vascular intervention. In this case, the patient’s signs resolved spontaneously by 21 months after onset, leaving no residual ocular deficits. | | | Introduction | A carotid cavernous fistula (CCF) is an aberrant communication between the cavernous sinus and the internal carotid artery or branches of the external carotid artery.(1) In the case of traumatic CCF, the intracavernous carotid artery and its branches are usually torn, resulting in the fistula. Elevated pressure inside the cavernous sinus and alterations in venous drainage account for the observed clinical signs, including conjunctival injection, proptosis, decreased visual acuity, elevated intraocular pressure (IOP), and cranial nerve palsies.(1-3)
CCF is usually treated aggressively with a variety of neurosurgical or vascular procedures to prevent progression of ophthalmic manifestations and irreversible consequences, such as permanent optic nerve damage, and to counter potential neurologically devastating or even fatal outcomes from blunt cerebrovascular injury, including intracranial hemorrhage and embolic stroke.(1-4) We describe a case of spontaneous resolution of ophthalmologic sequelae in a patient who developed post-traumatic, bilateral carotid dissections that resulted in bilateral CCF and central retinal venous insufficiency.
| | | Case Report | A 38-year-old woman presented to the USF Eye Institute in Tampa, Florida, for ophthalmological evaluation 2 months after a motor vehicle collision in which she suffered multiple cervical fractures and had become comatose for 9 days. During this period, she was reported to have periorbital edema, dilated pupils, and palsies of the left oculomotor and abducens nerves. Her medical history was otherwise unremarkable.
On examination at our institute, her uncorrected visual acuity was 20/20 in her right eye and 20/25 in her left eye. Visual fields were full to confrontation. Her intraocular pressure (IOP) was 14 mm Hg in the right eye and 10.5 mm Hg in the left eye. She had full motility in her right eye and was orthotropic in primary gaze. Although horizontal eye movements appeared full, the patient had an exotropia of 12 prism diopters on right gaze and an esotropia 16 prism diopters on left gaze, suggesting both an adduction and abduction deficit of the left eye. She wore a black patch on the left eye to relieve her horizontal diplopia. Neither proptosis nor bruit were observed at this time. The patient’s right pupil demonstrated 3+ reactivity; her left pupil exhibited residual dilation with 2+ reactivity. There was no relative afferent pupillary defect. Fundus examination was unremarkable.
Diplopia resolved by 7 months after trauma. The patient’s visual acuity remained 20/20 in the right eye and 20/25 in the left eye, with full extraocular movements. Her periorbital edema and left oculomotor and abducens cranial nerve palsies had resolved. The patient’s fundus examination remained normal; however, she continued to have residual left pupillary dilation.
By 10 months after trauma, the patient had begun to complain of distorted vision and exhibited a left relative afferent pupillary defect. Her visual acuity was stable, with full visual fields to confrontation and Humphrey automated perimetry indicating limited focal depressions. Her extraocular movements were intact, and she did not demonstrate conjunctival injection, chemosis, arterializaiton of the episcleral vessels, pulsatile proptosis on Goldmann applanation, or orbital bruit. However, dilated fundus examination of the left eye revealed abnormal venous engorgement with disc edema (Figure 1). There was concern for impending venous occlusion due to stasis. On computed tomography (CT), the patient did not demonstrate proptosis, globe abnormalities, evidence of clinoid meningioma, conal masses, or orbital masses. Subsequent computed tomographic angiography (CTA) was markedly abnormal, with significant dilation of the superior ophthalmic veins bilaterally, measuring 4.3 mm on the right and 3.3 mm in diameter on the left (Figure 2). Her cavernous sinuses were also dilated, reaching 14.6 mm × 26.8 mm on axial scan on the right and 7.2 mm in diameter on the left, consistent with CCF (Figure 3). No carotid cavernous aneurysms were observed at this time, and the normal size and morphology of the cavernous sinus allowed cavernous sinus thrombosis to be ruled out. There was a recanalized dissection of the right high anterior cerebral artery, a branch off the internal carotid artery, with a 5 mm irregularity in the vessel wall. There was also marked left internal carotid artery dilation with recanalization and lateral pseudoaneurysm consistent with an old left internal carotid artery dissection. The risks of neurosurgical or vascular intervention were deemed to outweigh the potential benefits, given the limited nature of the patient’s symptoms and the precarious nature of her fistulae.
One year after presentating, the patient was still experiencing some visual distortions but continued to have full visual fields and unchanged visual acuity. Amsler grid testing revealed no deficits or distortions. IOP remained within normal limits and no inflammatory cell was observed on slit-lamp biomioscropy. Gonioscopy did not reveal any blood in Schlemm’s canal or angle neovascularization. On dilated fundus examination, the left disc was edematous. There were dilated and tortuous vessels bilaterally with midperipheral hemorrhages in the left eye (Figure 4). Most of the blot hemorrhages were observed anterior to the equator, although a few were observed posterior to it. Optical coherence tomography (OCT) documented left optic disc edema. Fluorescein angiography was normal in the right eye, but the left eye showed leakage around the disc (Figure 5A). The left eye had a prolonged arteriolar to venous transit time of 6.71 seconds and demonstrated staining of the disc (Figure 5B). The perifoveal capillary network was intact, and there was adequate macular perfusion.
Over the next 7 months, the patient’s visual acuity remained 20/20 in both eyes and her IOP was normal. Visual field examination revealed no defects and the focal depressions on Humphry automated perimetry had resolved. The retinal vessels remained tortuous, although the disc edema and hemorrhages began to subside (Figure 6). Her angles remained open and her macula remained flat and dry. Magnetic resonance angiography performed 16 months after the accident demonstrated persistent bilateral cavernous pseudoaneurysms and marked dilation of the left superior ophthalmic vein.
| |
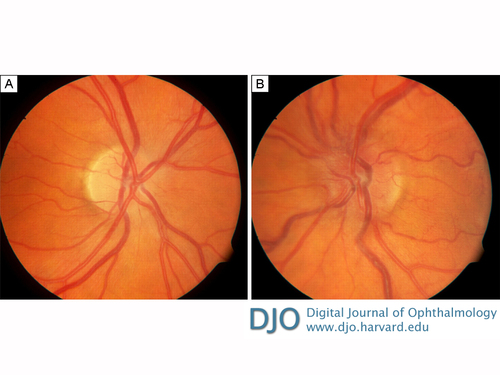
Figure 1
Photographs of the retina 10 months after trauma, showing disc edema with dilated veins in the right eye (A) and disc edema, dilated veins, and tortuous vessels in the left eye (B).
|
|
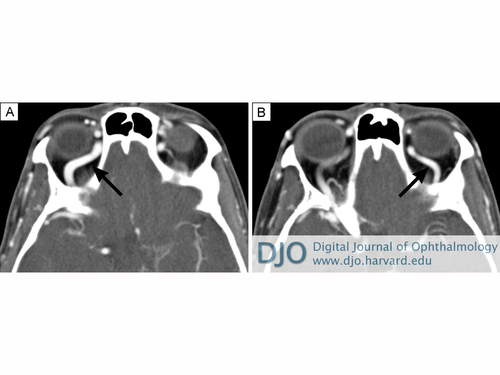
Figure 2
Computed tomography angiography 9 months after trauma was markedly abnormal, with the right (A) and left (B) superior ophthalmic veins significantly dilated, measuring 4.3 mm and 3.3 mm, respectively.
|
|

Figure 3
CT angiography 9 months after trauma showing bilateral cavernous sinus dilation, measuring 14.6 mm × 26.8 mm on axial scan on the right and 7.2 mm in diameter on the left, consistent with carotid cavernous fistulae.
|
|
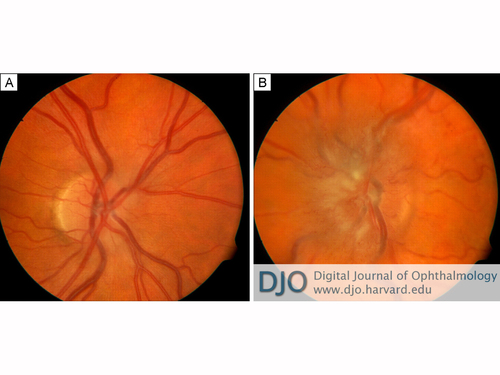
Figure 4
Photographs of the retina 13 months after trauma. A, The right eye showed swelling of disc margin temporally and thinning of the disc margin nasally; increased dilation of vessels was noted, but no hemorrhages were seen. B, The left eye showed swelling of disc nasally with mid-peripheral hemorrhages and tortuous vessels. A high concentration of blot hemorrhages was seen anterior to the equator, and the posterior pole lacked hemorrhages.
|
|
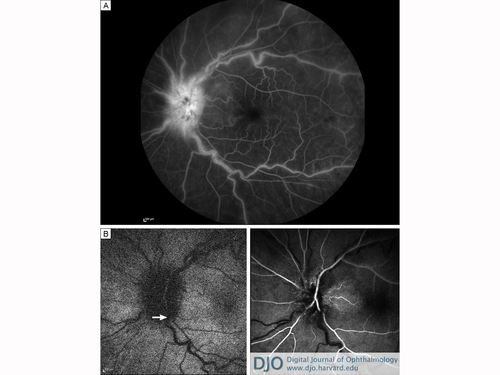
Figure 5
Fluorescein angiography, 13 months post trauma. A, The left eye shows leakage around the disc and surrounding hemorrhages and late staining of the walls with adequate macular perfusion with an intact perifoveal capillary network. B, An arterial venous filling delay of 6.71 sec was noted, indicating a low flow state within the venous system in the left eye. Arrows delineate the arterial venous delay, with the left arrow noting the arterial flash in the retinal artery and right arrow demonstrating the venous flash in the retinal vein in the fluorescein angiogram.
|
|

Figure 6
Photographs of the retina 20 months after trauma. A, The right eye shows decreased disc swelling and vessel dilation compared to imaging at 13 months after trauma, but tortuosity in the vessels was still noted. B, The left eye also shows decreased but persistent disc swelling, with blurry disc margins and continuing tortuosity of the vessels.
|
|
| Discussion | In traumatic CCF, the intracavernous carotid artery and its branches are torn, resulting in an inappropriate communication between the intracavernous carotid artery and the cavernous sinus.(2,3) Traumatic CCF is usually accompanied by significant cervical damage and additional damage to the vasculature, including lesions of the vertebral arteries.(4-6) Additionally, the cavernous sinuses are closely associated with numerous structures related to ocular function, including the superior and inferior ophthalmic veins as well as cranial nerves III, IV, V1, V2, and VI.(1) The abducens nerve is particularly vulnerable to injury from vascular engorgement and trauma due to its proximity to the internal carotid artery and unsecured course through the cavernous sinus.(7)
Elevated pressure inside the cavernous sinus and alterations in venous drainage account for clinically observed signs.(2) Anterior drainage results in congestive orbito-ocular features due to blockage of the superior ophthalmic vein,(8) including conjunctival injection and chemosis, proptosis, bruit, elevated intraocular pressure, and reduced visual acuity.(1) Posterior drainage may cause cranial nerve palsies, resulting in diplopia, ophthalmoplegia, and trigeminal neuropathy.(1) This is likely due to neural compression by an expanding cavernous sinus or inferior petrosal sinus, venous congestion and thrombosis, vascular steal with ischemia to the blood supply, or any combination of these etiologies.(8-11)
Ophthalmologic sequelae may include open-angle glaucoma, glaucoma secondary to neovascularization, retinal ischemia, central retinal artery occlusion, and, as seen in our patient, central retinal vein obstruction (CRVO).(12-14) CRVO not associated with CCF has been found to be the result of thrombus formation within the central retinal vein at the level of the lamina cribrosa.(15) It is possible that, in our patient, the CCF resulted in reduced arteriolar pressure and elevated venous pressure, leading to the CRVO-like picture in the left eye in the absence of thrombosis at the level of the lamina cribosa. Prolonged arteriolar-to-venous transit time on fluorescein angiography indicates low flow rates in the retinal vessels. The preponderance of retinal hemorrhages anterior to the equator suggests low pressure within the central retinal artery. Similar hemorrhage distribution patterns are seen in high-grade carotid artery occlusions, whereas CRVO independent of carotid occlusive disease typically has more posterior hemorrhages. The markedly dilated superior ophthalmic veins suggest that there was also elevated venous pressure in the retinal vessels, which could cause the optic disc edema and contribute to the vascular dilation.
CCF is typically treated aggressively, particularly in high-flow states due to the frequency of unilateral vision loss.(16) Treatment modalities include embolization of the fistula with neurosurgical coils(17-18) and the use of Amplatzer vascular plugs to occlude large vessels and high-flow lesions.(19) Goldberg et al describe a small case series in which they were able to successfully access the cavernous sinus through dilated superior ophthalmic veins by anterior orbitotomy with cannulation without any significant complications.(20) The primary goal of management is obliteration of the fistula to prevent further venous hypertension and intracranial hemorrhage.(20) Additionally, symptomatic management, particularly medical and surgical control of IOP, is used to reduce the rate of associated complications.(14)
In the literature, resolution of CCF and its ocular manifestations is almost exclusively achieved with one more interventions.(2-3,14,17-21 ) However, Yong and Heran describe a case of post-traumatic carotid and vertebral artery dissection with CCF that resolved without neurosurgical intervention.(5) They do not describe any ophthalmologic findings or sequelae. In contrast, our patient had venous stasis with ophthalmic signs that waned over time, resolving without neurosurgical or vascular intervention. The patient’s only lingering sequela was minimal pupillary dilation, and she retained 20/20 visual acuity in both eyes, though her vascular abnormalities persisted at last follow-up.
Intervention is not without risk, and in cases similar to ours, in which the potential complications associated with intervention are great, the knowledge that spontaneous and thorough resolution is possible, if rare, may help guide clinicians in making the decisions for patient management. Physicians may choose to monitor patients that are stable and experiencing few and non-life-threatening symptoms. | | | References | 1. Mateos E, Arruabarrena C, Veiga C, et al. Massive exophthalmos after traumatic carotid-cavernous fistula embolization. Orbit 2007;26:121-4.
2. Fang C. Endovascular treatment of a high-flow direct traumatic carotid cavernous fistula with a two year follow-up. Interv Neuroradiol 2008;14:297-301.
3. Phadke RV, Kumar S, Sawlani V, et al. Traumatic carotid cavernous fistula: anatomical variations and their treatment by detachable balloons. Australas Radiol 1998;42:1-5.
4. Keilani ZM, Berne JD. Bilateral internal carotid and vertebral artery dissection after a horse-riding injury. J Vasc Surg 2010;52:1052-7.
5. Yong RL, Heran NS. Traumatica carotid cavernous fistula with bilateral carotid artery and vertebral artery dissections. Acta Neurochir (Wien) 2005;147:1109-13.
6. Fukuda I, Meguro K, Matsusita S, et al. Traumatic disruption of bilateral vertebral arteries and internal carotid arteries: a case report. J Trauma 1989;29:263-6.
7. Bilyk JR. Embryoogy and anatomy of the orbit and lacrimal system. In: Tasman W, Jaeger EA, eds. Duane’s Foundations of Clinical Ophthalmology. 2013e. Philadelphia, PA: Lippincott Williams & Wilkins; 2013.
8. Ikeda K, Deguchi K, Tsukaguchi M, et al. Absence of orbito-ocular signs in a dural carotid-cavernous sinus fistula with a prominent anterior venous drainage. J Neurol Sci 2005;236:81-4.
9. Leonard TJ, Moseley IF, Sanders MD. Ophthalmoplegia in carotid cavernous sinus fistula. Br J Ophthalmol 1984;68:128-34.
10. Acierno MD, Trobe JD, Cornblath WT, Gebarski SS. Painful oculomotor palsy caused by posterior-draining dural carotid cavernous fistulas. Arch Ophthalmol 1995;113:1045-9.
11. Miyachi S, Negoro M, Handa T, Sugita K. Dural carotid cavernous sinus fistula presenting as isolated oculomotor nerve palsy. Surg Neurol 1993;39:105-9.
12. Fattahi T, Brandt T, Jenkins W, Steinberg B. Traumatic carotidcavernous fistula: pathophysiology and treatment. J Craniofac Surg 2003;14:240-6.
13. Keizer R. Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit 2003;22:121-42.
14. Gupta N, Kikkawa D, Levi L, Weinreb R. Severe vision loss and neovascular glaucoma complicating superior ophthalmic vein approach to carotid-cavernous sinus fistula. Am J Ophthalmol 1997;124:853-5.
15. Jonas JB, Berenhstein E, Holbach L. Anatomic relationship between lamina cribrosa, intraocular space, and cerebrospinal fluid space. Invest Ophthalmol Vis Sci 2003;44:5189-95.
16. Kupersmith MJ, Berenstein A, Flamm E, Ransohoff J. Neuroophthalmologic abnormalities and intravascular therapy of traumatic carotid cavernous fistulas. Ophthalmology 1986;93:906-12.
17. Preechawat P, Narmkerd P, Jiarakongmun P, et al. Dural carotid cavernous sinus fistula: ocular characteristics, endovascular management and clinical outcome. J Med Assoc Thai 2008;91:852-8.
18. Leibovitch I, Modjtahedi S, Duckwiler GR, Goldberg RA. Lessons learned from difficult or unsuccessful cannulations of the superior ophthalmic vein in the treatment of cavernous sinus dural fistulas. Ophthalmology 2006;113:1220-6.
19. Gralla J, Schroth G, Kickuth R, et al. Closing the gap between coil and balloon in the neurointerventional armamentarium: Initial clinical experience with a nitinol vascular occlusion plug. Neuroradiol 2008;50:709-14.
20. Goldberg RA, Goldley SH, Duckwiler G, Vinuela F. Management of cavernous sinus-dural fistulas. Arch Ophthalmol 1996;114:707-14.
21. Bhatti MT, Peters KR. A red eye and then a really red eye. Surv Ophthalmol 2003;2:225-9.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in