|
|
 |
 |
 |
 |
|
|
Iatrogenic choroidal neovascularization following idiopathic epiretinal membrane peel
Digital Journal of Ophthalmology
2013
Volume 19, Number 1
March 31, 2013
DOI: 10.5693/djo.02.2013.02.001
|
Printer Friendly
Download PDF |
|
|


 Yi Wei Goh, MBChB
Yi Wei Goh, MBChB | Department of Ophthalmology, Faculty of Medical and Health Sciences, University of Auckland, New Zealand Rita Ehrlich, MD | Department of Ophthalmology, Faculty of Medical and Health Sciences, University of Auckland, New Zealand Sarah Welch, FRANZCO | Department of Ophthalmology, Auckland District Health Board, New Zealand
|
|
|
| Abstract | | Choroidal neovascularization is an uncommon complication of macular surgery. The functional outcome is poor despite various treatment options, including laser photocoagulation, photodynamic therapy, and a variety of surgical procedures. We report a case of iatrogenic choroidal neovascularization in a 69-year-old woman at the site of inadvertent retinal trauma 5 weeks after an epiretinal membrane peel. Visual acuity was 6/15 at the time of diagnosis. Four intravitreal bevacizumab injections were administered over a period of 6 months; treatment was discontinued when a disciform scar was noted. At last follow-up, 21 months after surgery, the patient’s visual acuity was counting fingers. | | | Introduction | | Surgical removal of symptomatic epiretinal membrane (ERM) is a common procedure. Functional improvement is generally expected in approximately 80% to 90% of cases, with improvement in visual acuity and reduction of metamorphosia.(1) The procedure is not without risk, and some sight-threatening complications can occur, including retinal breaks, rhegmatogenous retinal detachments, and endophthalmitis. In phakic patients, cataract formation is common.(1) The development of a choroidal neovascular membrane (CNVM) following ERM peel is rare.(2) | | | Case Report | A 69-year-old woman presented at the Auckland District Health Board with ongoing visual distortion and central scotoma on the right eye. Previous ocular and medical histories were noncontributory. On ophthalmological examination, the best-corrected visual acuity was 6/18 in the right and 6/6 in the left eye. The anterior segments were unremarkable in both eyes. Dilated fundus examination of the left eye was normal, but an epiretinal membrane was identified in the right macula and confirmed on optical coherence tomography (Figure 1). No other abnormality was observed, and the membrane was deemed idiopathic.
The patient underwent a standard 23-gauge pars plana vitrectomy with an epiretinal membrane peel using Membrane Blue (Dutch Ophthalmic USA, Exeter, NH). During the surgery, the retina was traumatized deep to the retinal pigment epithelium (RPE) and a small, deep intraretinal hemorrhage developed. The patient was regularly examined following the surgery because of persistent visual distortion. Five weeks after surgery the patient’s visual acuity was 6/15, but at the site of the retinal injury a serous elevation of the neurosensory retina was noted with a retinal hemorrhage. CNVM was diagnosed (Figure 2). Macular optical coherence tomography (OCT) showed disruption of RPE along the superotemporal arcade together with the serous detachment (Figure 3). Fluorescein angiography revealed a classic CNVM (Figure 4).
At that point our review of the literature indicated poor response of iatrogenic CNVM to laser photocoagulation, photodynamic therapy, and surgical removal of subretinal fluid.(2-6) Because intravitreal bevacizumab injections had been used effectively to treat CNVM secondary to other retinal diseases, it was decided that this treatment would be used in the present case. However, intravitreal bevacizumab injections are not readily available in our hospital, and strict criteria are applied before approval of their use. Treatment was started 5 weeks after the diagnosis of CNVM. Intravitreal bevacizumab injections in the right eye were administered every 6 weeks over a 6-month period, but visual acuity failed to improve. Nine months following surgery, a disciform scar developed and treatment was discontinued, at which time visual acuity in the right eye was counting fingers. | |
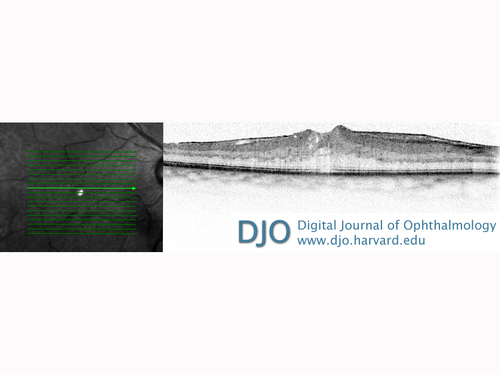
Figure 1
Optical coherence tomography (OCT) of the right eye of a 69-year-old woman confirming an epiretinal membrane, with some intraretinal fluid in the foveal region.
|
|
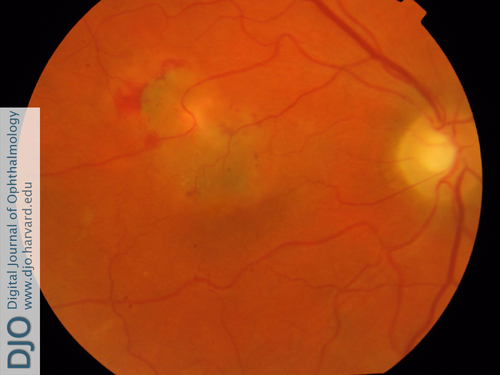
Figure 2
Clinical photograph of choroidal neovascularization that developed at the site of hemorrhage 5 weeks after epiretinal membrane peel.
|
|
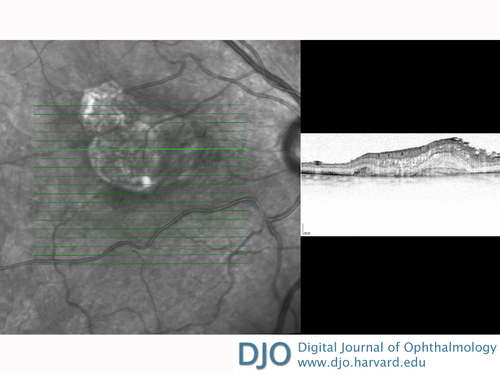
Figure 3
OCT demonstrating disruption of retinal pigment epithelium along the superotemporal arcade, with an adjacent serous detachment.
|
|
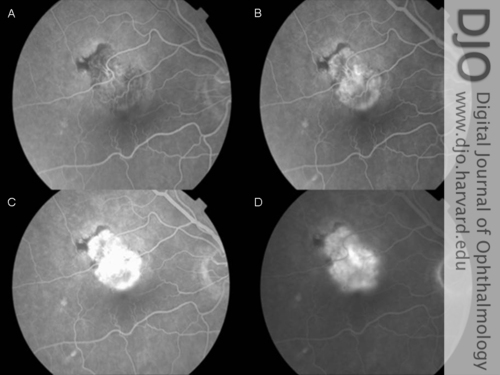
Figure 4
Fluorescein angiography of the right eye showing a lesion approximately 1.5 disc diameters in size with early hyperfluorescence that increases in size and intensity in the late frames, indicative of a classic choroidal neovasular membrane. There is an associated superotemporal hypofluoresence caused by a blockage from a retinal hemorrhage. A, 22.3 sec. B, 39.9 sec. C, 1 min 2.4 sec. D, 5 min 23.1 sec.
|
|
| Discussion | Anti-vascular endothelial growth factor (VEGF) therapy inhibits the release of pro-angiogenetic cytokines and has been proven to be an effective treatment for CNVM of various etiologies. In the present case, the disruption of Bruch’s membrane due to direct surgical trauma most likely triggered the reparative response process that constituted the activation of retinal pigment epithelium (RPE) that in turn synthesized and released VEGF. Although the pathogenesis is seemingly similar to CNVM secondary to age-related macular degeneration, angioid streaks, or myopic degeneration, the effective therapeutic response to anti-VEGF injections was not as favorable as hoped. To our knowledge, this is the first case of iatrogenic CNVM following epiretinal peel that was treated with intravitreal bevacizumab. Unfortunately, the visual prognosis remained poor.
CNVM complicating idiopathic epiretinal membrane peel surgery is uncommon. A literature search revealed 6 previously published cases, all but 2 of which have occurred in males.(2-6) The mean age of those presenting with this complication was 62.83 years (range, 20-80). The development of the CNVM coincided with a worsening of visual acuity, with the mean pre-operative best-corrected visual acuity deteriorating from 20/65 to 20/230 in 5 of the 6 reported cases. The development of the CNVM occurred at a mean of 6.16 months (range, 1-24) following the epiretinal membrane peel. Despite a variety of treatment modalities, the functional outcome was poor, with an average final visual acuity of 20/260.
In 5 patients, the CNVM was treated with laser argon photocoagulation, resulting in stable visual acuities in 4 eyes.(2-6) One patient with CNVM recurrence subsequently received 4 sessions of photodynamic therapy, but subretinal fibrosis developed, and the visual acuity remained poor. Another, highly myopic patient (−7.75 D) underwent surgical removal of the sub-retinal membrane but subsequently developed a rhegmatogenous retinal detachment. After reattachment, a further vitrectomy and silicone oil injection were performed. Final visual acuity in this patient was 20/500.(3)
CNVM can also complicate macular hole surgery. A retrospective report detailing 9 eyes of 8 patients with foveal-involving CNVM complex following macular hole repair.(3) In these eyes all macular holes were successfully closed with surgery. The fluorescein angiograms in 8 of the 9 eyes were described as having moderate to severe leakage of fluorescein during the transit, implying an aggressive membrane. One patient in that series was treated with photodynamic therapy and achieved 20/50 acuity. This compared favorably to the outcome experienced by other treatment types, of which the resulting average best-corrected visual acuity at final follow-up was <20/200.(3)
Kelly and Wendel reported approximately 10% of the patients who underwent macular hole surgery were found to have postoperative RPE mottling and suggested that it could be due to intraocular manipulation, direct trauma, or light toxicity.(7) We postulate that the inflammatory process following surgical intervention might have contributed to the additional oxidative stress to the neurosensory retina and that a preexisting surgically induced abnormal RPE activation resulted in an unfamiliar VEGF upregulation. This phenomenon may explain the unexpected lack of response to anti-VEGF treatment.
To date, in addition to our case, 6 cases of choroidal neovascularization after idiopathic epiretinal membrane peel and 14 cases of choroidal neovascularization following macular hole surgery have been reported, all with poor functional outcomes despite various modes of treatment.
Literature Search
PubMed was searched without language restriction using the medical subject headings database; hierarchal search was conducted in June 2012 and was based on the following terms: epiretinal membrane and choroidal neovascularization. | | | References | 1. Fang X, Chen Z, Weng Y, et al. Surgical outcome after removal of idiopathic macular epiretinal membrane in young patients. Eye (Lond) 2008;22:1430-5.
2. Graham K, D’Amico DJ. Postoperative complications of epiretinal membrane surgery. Int Ophthalmol Clin 2000;40:215-23.
3. Warden SM, Pachydaki SI, Christoforidis JB, et al. Choroidal neovascularization after epiretinal membrane removal. Arch Ophthalmol 2006;124:1652-4.
4. Ng EW, Bressler NM, Boyer DS, de Juan E, Jr. Iatrogenic choroidal neovascularization occurring in patients undergoing macular surgery. Retina 2002;22:711-8.
5. Korobelnik JF, Dureau P, Sarfati A, et al. Choroidal neovascularization complicating epiretinal membrane removal. Acta Ophthalmol Scand 1997;75:320-1.
6. Ferrari TM, Dammacco R, Quaranta GM, et al. Choroidal neovascularization secondary to vitrectomy for idiopathic epiretinal membrane: report of an unusual case. Eur J Ophthalmol 2003;13:218-20.
7. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes: results of a pilot study. Arch Ophthalmol 1991;109:654-9. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in