|
|
 |
 |
 |
 |
|
|
Optical coherence tomography changes in macular CMV retinitis
Digital Journal of Ophthalmology
2012
Volume 18, Number 2
May 13, 2012
DOI: 10.5693/djo.02.2012.04.001
|
Printer Friendly
Download PDF |
|
|
|
|
|
|
| Abstract | | Cytomegalovirus (CMV) retinitis characteristically causes peripheral retinitis with associated vasculitis. It rarely begins in the macula or causes macular necrosis exclusively. We report a case of unilateral macular CMV retinitis in a 65-year-old immunosuppressed patient and document changes in the macula during treatment through optical coherence tomography (OCT). | | | Introduction | | Active cytomegalovirus (CMV) infection is a serious and common infectious complication in immunosuppressed patients. It can take the form of retinitis, pneumonitis, hepatitis, colitis, and nephritis.(1) While CMV retinitis is the most common ocular complication in patients with acquired immunodeficiency syndrome (AIDS), it is relatively rare in patients following allogenic bone marrow transplant.(1-2) | | | Case Report | A 65-year-old man presented to the Eye Clinic of the Royal Brisbane and Women’s Hospital for evaluation after experiencing 2 weeks of blurred vision in his left eye. Three months earlier he had suffered a febrile illness during cytomegalovirus (CMV) reactivation and was started on intravenous foscarnet (50 mg/kg) after unresponsiveness to ganciclovir. Following a good response to foscarnet, the serological CMV DNA count dropped to <600 copies/ml some 2 months before presentation. Attempted cessation of foscarnet, however, resulted in reactivation of CMV 10 days later. The CMV DNA count increased to 2.0 × 104 copies/ml 3 weeks before his presentation to the eye clinic. He was recommenced on intravenous foscarnet.
His medical history included allogenic bone marrow transplant for acute myeloid leukemia 7 years previously, type 2 diabetes mellitus, thromboembolic disease (treated with warfarin), hypertension, stage 3 chronic kidney disease, hyperlipidemia, and chronic obstructive pulmonary disease. He had undergone bilateral cataract surgery more than a year before presenting. He had no other significant ophthalmic history.
On ophthalmological examination, his best-corrected visual acuity was 20/25 in the right eye and 20/125 in the left eye. Examination of the right eye was unremarkable. Examination of the left eye revealed a normal anterior segment, with clear anterior chamber and vitreous. Fundus examination revealed a confluent area of retinal whitening of approximately 1.5 disc areas at the macula, associated with retinal hemorrhages (Figure 1A). Peripheral retina and retinal vessels were otherwise normal, as was the optic disc. There was no vitritis. On presentation, optical coherence tomography (OCT) showed extensive necrosis of the fovea, resulting in significant destruction of the retinal nerve fiber layer and formation of multiple cystic spaces. There was also loss of the inner segment (IS)/outer segment (OS) junction of the photoreceptors (Figure 1B). Vitreous fluid polymerase chain reaction (PCR) from the left eye was positive for CMV DNA, thus confirming CMV retinitis. It was negative for bacteria, fungi, HSV-1, HSV-2, VZV, and EBV. While systemically responding to the intravenous foscarnet (serum CMV DNA <600 copies/ml), the patient’s vision deteriorated to 20/200 after 4 weeks of recommencement of intravenous foscarnet. Due to his fear of needles, the patient was started on weekly intravitreal foscarnet 2.4 mg/0.1 ml instead of twice weekly induction therapy. His vision improved to 20/125 after the first injection. After the first intravitreal injection, there was dramatic improvement in the retinal whitening seen on fundus examination (Figure 2A). He received a total of 5 injections. Serial OCT showed progression of retinal thinning/necrosis and collapse of cystic spaces and destruction of the retinal pigment epithelium (RPE) layer (Figures 2B and 3), which remained stable 3 months after the final injection (Figure 4B). Fundus photography showed scarring at the site of previous active retinitis (Figure 4A). At follow-up 6 months after treatment, his best-corrected visual acuity was 20/160. Fundus photography showed a mature scar at the macula (Figure 5A). OCT showed retinal thinning to the extent that no discernible structures were visible, and hypertrophy of the RPE layer (Figure 5B). | |
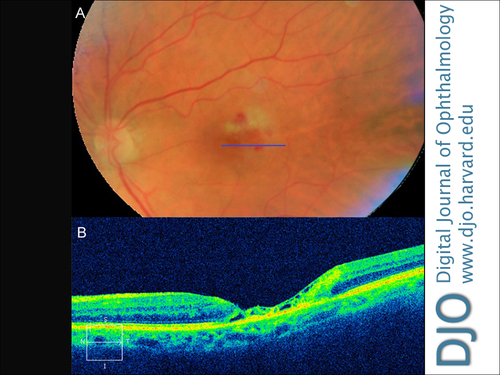
Figure 1
The left eye before intravitreal foscarnet therapy. A, Fundus photograph. B, Optical coherence tomography (OCT) image.
|
|

Figure 2
The left eye 5 days after the first foscarnet injection. A, Fundus photograph showing improvement of retinitis. B, OCT image showing cystic changes, extensive foveal thinning, and loss of inner segment/outer segment junction of photoreceptors.
|
|
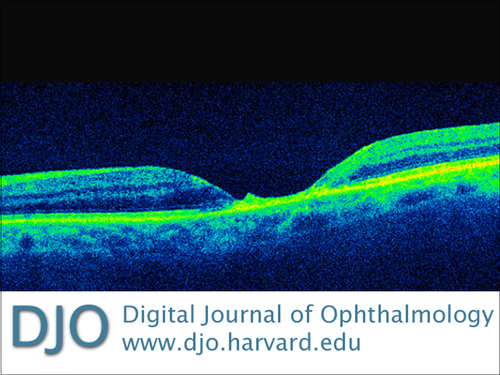
Figure 3
OCT image of the left eye after third foscarnet injection showing collapse of cystic spaces revealing almost complete loss of retinal tissues and destruction of RPE layer.
|
|
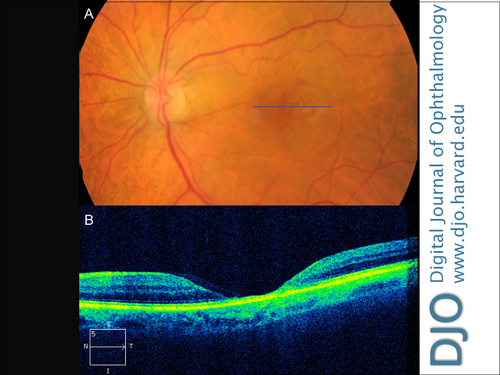
Figure 4
The left eye 3 months after treatment. A, Fundus photograph showing resolution of retinitis and mild scarring. B, OCT image showing marked thinning of retina without distinguishable internal structures.
|
|
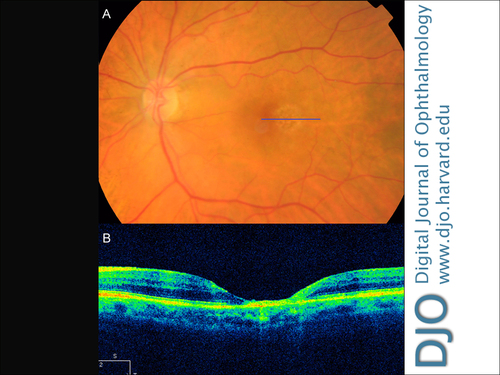
Figure 5
The left eye 6 months after treatment. A, Fundus photograph showing a mature macular scar. B, OCT image showing hypertrophy of RPE layer without change in retinal thinning.
|
|
| Discussion | CMV retinitis is an opportunistic ocular infection most commonly seen in people with AIDS. It can also affect those who are immunosuppressed after transplant surgery. It typically presents with peripheral areas of retinal whitening, often associated with retinal hemorrhages, which then progress in a “brushfire-like” extension across the posterior pole. If left untreated, significant vision loss and blindness can result. The macula is rarely affected first or exclusively in CMV retinitis.
Our case demonstrates an immunosuppressed patient after bone marrow transplant, who developed his first episode of CMV retinitis confined to the macula while on intravenous foscarnet therapy for recent CMV reactivation. This is a rare case of CMV retinitis that occurred exclusively in the macula in an immunosuppressed patient who did not have AIDS. There was no sign of peripheral retinitis as evidenced by the absence of peripheral retinal whitening or scarring, nor signs of vasculitis and vitritis. There are only a three published reports of CMV retinitis limited to the macula. One reported an AIDS patient who responded to intravitreal but not intravenous foscarnet;(3) a second reported presumed CMV retinitis beginning in the macula, which was left untreated allowing the retinitis to extend from the posterior pole.(4) Another case of exclusive macular CMV retinitis was reported in a patient following bone marrow transplant.(5)
In addition, our case demonstrates progressive OCT changes in the macula from CMV retinitis. Despite timely treatment, CMV retinitis is a destructive disease resulting in a significant necrosis of retinal tissues with destruction of inner and outer retinal tissues and retinitis involving the IS/OS junction of the photoreceptors. At 3 months, disruption of the RPE layer was seen, which progressed to hypertrophy of this layer at 6 months.
Intravitreal foscarnet and ganciclovir are effective first-line therapies for zone 1 CMV retinitis (ie, 2 disc diameter from foveal center and 1 disc diameter from margin of optic disc), and are also indicated when patients are intolerant or unresponsive to systemic therapy. They offer a higher concentration of the drug in the retina.(6) Previous small uncontrolled studies showed efficacious use of intravitreal foscarnet in CMV retinitis in AIDS patients with a lower rate of recurrences than ganciclovir.(7-8) In our patient, a good response was seen one week after the first intravitreal foscarnet injection with improvement in vision and regression of retinal whitening on clinical examination. Despite significant necrosis at the fovea, his vision improved to 20/120 albeit with a central scotoma. His vision has since regressed to 20/160 at the 6 months follow-up, and the CMV retinitis has been inactive since. Due to the absence of previous ocular symptoms and any peripheral retinal scarring, it is unlikely that peripheral retinitis was present prior to this presentation while the patient was on intravenous foscarnet. Peripheral retinal necrosis can be asymptomatic, but it is usually accompanied by vitritis, which can cause floaters. This case highlights the need for a high index of clinical suspicion in recognizing an atypical presentation of CMV retinitis, and the importance of providing prompt diagnosis and treatment of a potentially devastating infection. | | | References | 1. Hennis HL, Scott AA, Apple DJ. Cytomegalovirus retinitis. Surv Ophthalmol 1989;34:193-203.
2. Larsson K, Lonnqvist B, Ringen O et al. CMV retinitis after allogenic bone marrow transplant. Transpl Infect Dis 2002;4:75-79.
3. Demols P, Claes CA, Farber CM et al. Macular CMV retinitis: a case report. Bull Soc Belge Ophtalmol 2004;293:17-21.
4. To KW and Nadel AJ. Atypical presumed CMV retinitis. Graefe’s Arch Clin Exp Ophthalmol 1989;227:535-7.
5. Crippa F, Corey L, Chuang ER et al. Virological, clinical, and ophthalmological feature of cytomegalovirus retinitis after hematopoietic stem cell transplantation. Clin Infect Dis 2001;32:214-9.
6. Stewart MW. Optimal management of cytomegalovirus retinitis in patients with AIDS. Clin Ophthalmol 2010;4:285-99.
7. Diaz-Llopis M, Chipont E, Sanchez et al. Intravitreal foscarnet for cytomegalovirus retinitis in a patient with acquired immunodeficiency syndrome. Am J Ophthalmol 1992;114:742-7.
8. Diaz-Llopis M, Espana E, Munoz G et al. High dose intravitreal foscarnet in the treatment of cytomegalovirus retinitis in AIDS. Br J Ophthalmol 1994;78:120-4.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in