|
|
 |
 |
 |
 |
|
|
Anterior capsular rupture following blunt ocular injury
Digital Journal of Ophthalmology
2011
Volume 17, Number 4
November 15, 2011
DOI: 10.5693/djo.02.2011.10.005
|
Printer Friendly
Download PDF |
|
|


 Anas Gremida, MD
Anas Gremida, MD | Department of Ophthalmology, University of Illinois, Chicago Iris Kassem, MD | Department of Ophthalmology, University of Illinois, Chicago Aisha Traish, MD | Department of Ophthalmology, University of Illinois, Chicago
|
|
|
| Abstract | | A 10-year-old boy suffered a large, oblique anterior capsular tear following blunt injury to his right eye. The boy was followed daily for hyphema resolution and progressive traumatic cataract formation. After the hyphema had resolved, the lens was removed using an anterior approach and an intraocular lens was placed with excellent visual outcome. | | | Introduction | | Anterior capsular rupture secondary to penetrating injuries is well documented in the literature; anterior capsular tears following blunt ocular trauma are rare. We present a management approach with good visual outcome. | | | Case Report | A 10-year-old boy without past medical or ocular history sustained blunt trauma to his right eye by a rock slingshot. He presented to the emergency department of the University of Illinois one hour after being injured, at which time his visual acuity was 20/20 in the left eye and 20/200 in the right eye. There was 1+ conjunctival injection and moderate edema of the right upper eyelid. Slit-lamp examination of the right eye revealed a 0.5 mm × 0.5 mm central corneal abrasion and a 1.5 mm layered hyphema with 3+ red blood cells. There was traumatic mydriasis with posterior synechiae at 3 o’clock and 6 o’clock. Biomicroscopic examination of the lens revealed an early traumatic cataract with an anterior capsular tear running obliquely from 2 o'clock to 7 o'clock (Figure 1). The intraocular pressure (IOP) by Goldmann applanation was 23 mm Hg in the right eye and 18 mm Hg in the left eye. Dilated fundus examination revealed commotio retinae inferior to the right optic nerve. There were no fractures or foreign bodies. Clinical examination showed no sign of a ruptured globe; this was confirmed radiographically by noncontrast computed tomography (CT) scan of the orbits. He was negative for sickle cell trait.
Initial therapy included a topical cycloplegic, steroid, and antibiotic. He was monitored daily for intraocular pressure and lens changes and to follow resolution of the hyphema. The corneal abrasion was healed by day 2. With topical IOP-lowering medication, the maximum IOP of 34 mm Hg on day 6 returned to 15 mm Hg on day 9. The hyphema had resolved by day 19. Over this period of time, the lens slowly hydrated and began to protrude anteriorly, with reduction in vision consistent with the lenticular changes (Figure 2). The final preoperative vision was counting fingers at two feet.
After aspiration of the lens, the posterior synechiae were lysed by blunt dissection using a cannula containing dispersive viscoelastic and the anterior capsule was stained with trypan blue. Given that the anterior lens capsule was torn obliquely, our surgical plan was to create two half circles that would result in an ideally circular, continuous capsulorhexis. This was first attempted using a cystotome and Utrata forceps but completed with microscissors, as the capsule had fibrosed centrally at the location of the tear and was resistant to simple mechanical pulling from the Utrata forceps. No frank radialization of the tear posteriorly was noted, and there was no vitreous loss, but the remaining integrity of the anterior capsular support was in doubt; both edges of the tear were beyond the pupillary margin and could not be located even when the iris was mechanically elevated to enhance visualization. Therefore, it was considered optimal to stage sulcus placement of the lens, when the anterior capsule was fibrosed peripherally to the posterior capsule. This was accomplished successfully the following month, with a three-piece acrylic intraocular lens. Visual acuity 9 months after lens implantation was 20/25 in the right eye, with mild refractive correction and mild posterior capsular opacification (Figure 3). | |
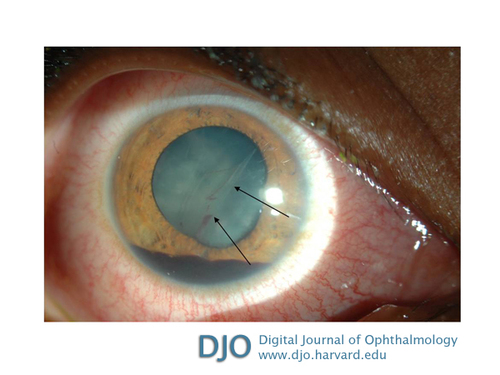
Figure 1
Slit-lamp photograph of the right eye of a 10-year-old boy 8 days after blunt trauma showing oblique anterior capsular tear running peripherally under the pupillary margin (arrows) in addition to layered traumatic hyphema and cataract.
|
|

Figure 2
Preoperative photograph showing the scarred anterior capsular tear (arrow) and hydrated traumatic cataract of the right eye. The traumatic hyphema of the right eye had resolved, with no active inflammation, but the traumatic cataract had become hydrated.
|
|
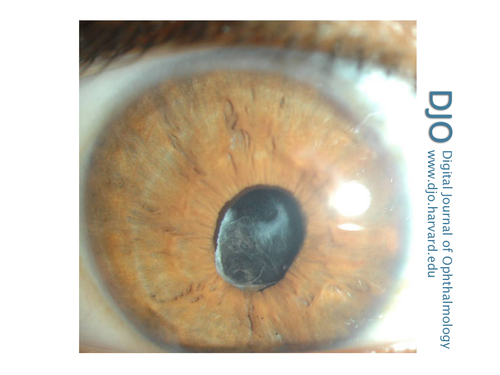
Figure 3
Photograph of the right eye taken 9 months after surgery showing mild posterior capsular opacification and fibrosis of the lens capsule; the intraocular lens (IOL) was well positioned in the sulcus.
|
|
| Discussion | Capsular ruptures following blunt trauma are infrequent. Posterior capsular tears secondary to blunt trauma are more common than anterior capsular tears.(1) The difference is likely due in part to the fact that the posterior capsule is thinner and weaker than the anterior capsule,(2-4) making it more vulnerable to this type of injury. The higher frequency of posterior capsular tears may also be due to the adherence of Wieger's ligament to the posterior capsule. The fact that this ligament is stronger in children than in adults may prompt suspicion of posterior capsular tears in cases of blunt trauma in children.(5)
The first traumatic anterior capsular rupture due to blunt injury was described by Bresgen in 1881.(6) Most cases since described have been due to air bag injury.(7) Banitt et al hypothesized that anterior capsular tears may be due to direct injury from a localized depression of the cornea onto the lens (coup injury) or due to a rapid anteriorly directed recoil of vitreous that ruptures the capsule via the mechanical fluidic forces (contre-coup injury).(1)
Our case highlights the importance of recognizing the rarer anterior capsular tear, so that surgical planning and appropriate traumatic cataract management may be employed. None of the cases described by Banitt et al were taken for immediate lens extraction. In fact, 2 of the 3 cases described underwent cataract extraction at least 1 week after injury and had in the interim been treated for posttraumatic inflammation and hyphema. They both had uneventful surgeries and excellent visual outcomes. This suggests that urgent lensectomy is not critical for a good visual outcome; perhaps the technique of minimizing preoperative inflammation can be beneficial in the postoperative phase. Certainly, when lens material is liberated into the anterior chamber from a large violation of the anterior lens capsule, it is critical to remove the lens promptly. However, as Banitt et al demonstrated, and as is the case with our patient, there are situations where rupture of the anterior lens capsule does not necessitate immediate surgery. We propose that time for quiescence of trauma-induced inflammation or layered hemorrhage prior to traumatic cataract extraction can be beneficial. | | | References | 1. Banitt MR, Malta JB, Mian SI, Soong HK. Rupture of the anterior lens capsule from blunt ocular injury. J Cataract Refract Surg 2009;35:943-5.
2. Lee SI, Hong HC. A case of isolated posterior capsule rupture and traumatic cataract caused by blunt ocular trauma. Korean J Ophthalmol 2001;15:140-4.
3. Rosen WJ, Campbell DG. Posterior capsule rupture after a paint-pellet injury. J Cataract Refract Surg 2000;26:1422-3.
4. Pavlovic S. Epilenticular intraocular lens implantation in traumatic cataract with a ruptured posterior capsule. Am J Ophthalmol 2000;130:352-3.
5. Campanella PC, Aminlari A, DeMaio R. Traumatic cataract and Wieger’s ligament. Ophthalmic Surg lasers 1997;28:422-3.
6. Bresgen H. Zur Kenntnis der Linsenkapselverletzungen. Arch Augenheilkd 1881;10:265-8.
7. Zabriskie NA, Hwang IP, Ramsey JF, Crandall AS. Anterior capsular rupture caused by air bag trauma. Am J Ophthalmol 1997;123:832-3. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in