|
|
 |
 |
 |
 |
|
|
Chorioretinal atrophy after electrical injury
Digital Journal of Ophthalmology
2011
Volume 17, Number 3
September 6, 2011
DOI: 10.5693/djo.02.2011.07.003
|
Printer Friendly
Download PDF |
|
|


 Gregory Zablocki, BA
Gregory Zablocki, BA | Department of Ophthalmology, Colorado School of Medicine Curtis Hagedorn, MD | Colorado Retina Associates
|
|
|
| Abstract | Objective
A 26-year-old-man who had suffered a severe electrical injury 3 years previously presented with blurred vision in his left eye caused by a posterior subcapsular cataract with nuclear sclerotic changes and peripapillary chorioretinal scarring. The pattern of retinal atrophy surrounding the optic nerve suggests a possible path of electrical current to the eye and demonstrates the selective tissuedamage that may occur in electrical injuries. | | | Introduction | | The clinical findings of cataract formation following electrical injury are well documented.(1-4) Macular cysts and holes have also been reported.(5,6) We present a case of retinal damage after severe electrical injury. | | | Case Report | A 26-year-old man with blurred vision in his left eye was referred to Colorado Retina Associates for retinal evaluation prior to cataract surgery. The patient’s medical history was significant for an electrical injury suffered 3 years earlier, after which he began to notice the visual decline. The injury occurred when he was grasping the extended cables of a crane and the boom came into contact with high-tension transmission lines carrying a reported 115,000 Volt potential. He underwent amputation of all four extremities and remained in the burn unit for three months, receiving treatment for deep tissue burns on his left side, covering roughly 40% of the torso.
On ophthalmological examination, visual acuity was 20/20 in the right eye and 20/40-2 in the left eye, with no improvement on pinhole. The anterior examination of the left eye revealed a posterior subcapsular cataract with trace nuclear sclerotic changes (Figure 1A) The optic nerve was sharp, pink, and full, with a cup/disc ratio of 0.4 and an early posterior vitreous detachment. On dilated fundus examination of the left eye, preretinal fibrosis and chorioretinal atrophy surrounding the optic nerve and two smaller regions superonasal and inferotemporal of the same description were observed. (Figure 1B) Results of optical coherence tomography (OCT) correlated with fundus examination findings, showing retinal thinning and retinal pigment epithelium/choriocapillary irregularity in the area adjacent to the optic nerve (Figure 2). Anterior and posterior examination of right eye demonstrated normal anatomical findings, as did the OCT that was performed (Figure 3).
Based on our examination we concluded that the macula was of sufficient viability that cataract extraction would likely result in an improvement in vision. Cataract extraction was subsequently performed and an intraocular lens was implanted. Postoperatively his visual acuity improved to 20/30. | |
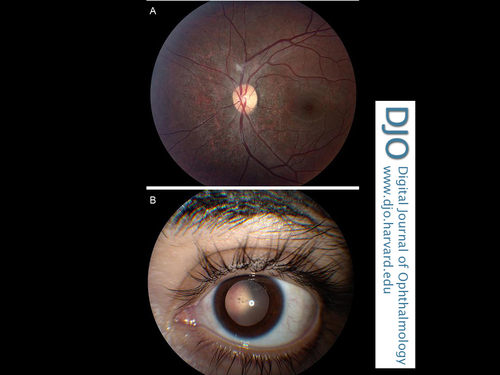
Figure 1
Left eye of electrical trauma patient. A, Fundus photograph of left eye showing fibroses and atrophy of the retina surrounding the optic disc. B, Cataract of the lens.
|
|
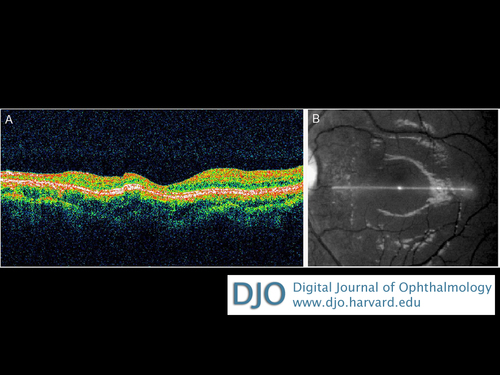
Figure 2
A, OCT of the left retina showing atrophy of the retina as well as the extent of the changes relative to the fovea. B, fundus photograph showing position of scan.
|
|
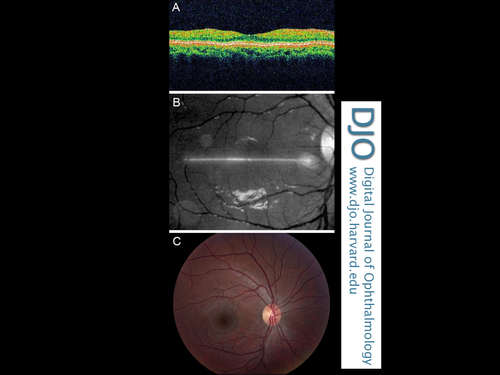
Figure 3
Normal anatomy of the right eye. A, posterior pole. B, OCT scan of retina. C, Fundus photograph showing position of scan.
|
|
| Discussion | | The ocular complications resulting from electrical injuries are quite varied; chemosis, corneal perforation, iritis, cataract, retinal pigment epithelium damage, macular edema, retinal detachment, macular hole, optic neuritis, and choroidal atrophy have all been previously reported.(4) The development of cataracts has been postulated to be induced by direct effect on the proteins of the lens from the current or by contraction of the ciliary muscle causing a concussion-type injury, changes in capsular permeability, or thermal damage.(1,5) The presumed mechanism for retinal damage is coagulative necrosis due to loss of choroidal and retinal vasculature and possibly electroporation.(4,7-9). The extent and pattern of damage from electrical injury is diverse but, simplistically, an approximation of damage from electrical injury is related to Joule’s law, Q = I²RT, where Q is the thermal energy generated; I, the electrical current; R, the resistance of the material the current is passing through; and T, the duration of exposure.(7) Increasing I, R, or T will result in greater generation of heat and subsequently more tissue damage. I and T depend on conditions of the event, while R is determined by the composition of the bodily tissue. The resistance of biological tissues increases in the order nerve, blood vessels, muscle, skin, tendon, fat, and bone.(4,7) With this paradigm in mind, a possible mechanism for the pattern of tissue injury observed in this case is suggested. The optic nerve could be the pathway of least resistance for current to flow to the eye. The relatively low resistance of the nerve may be what spares it from heat generation and damage. At the insertion of the optic nerve to the posterior of the eye, the current spreads through the sclera, choroid, and retina. The increased resistance of the sclera and choroid would thus cause increased heat and damage to these structures; the neuronal cells of the retina would generate less heat. As the current spreads from the optic nerve, the energy is dissipated over a larger area, causing proportionally less damage. This could explain the orientation of chorioretinal atrophy as well as the apparent selectivity of tissue damage in our case. The patient’s 20/30 vision and lack of peripheral vision defects suggest that the ganglion cell layer was spared. Yet the sparing of the central retinal vessels from significant involvement is somewhat contradictory to the proposed mechanism and a more formal investigation of how electrical current behaves in the eye would be needed to confirm the suggested etiology. The differing cellular composition of the eye may factor into the pattern of pathology, but how this presents clinically is still unpredictable; requiring that the complications must be treated on an individual basis. | | | References | 1. Boozalis G, Purdue G, Hunt J, McCulley J. Ocular changes from electrical burn injuries: a literature review and report of cases. J Burn Care Rehabil 1991;12:458-62.
2. Chun-Ju L, Chang-Hao Y, Chung-May Y, Kuo-Pin C. Abnormal Electroretinogram and abnormal electrooculogram after lightning-induced ocular injury. Am J Ophthalmol 2002;133:578-9.
3. Datta H, Sarkar K, Chatterjee PR, Datta S, Mukherjee U. An unusual case of late ocular changes after lightning injury. Indian J Ophthalmol 2002;50:224-5.
4. Miller B, Goldstein M, Monshizadeh R, Tabandeh H, Bhatti T. Ocular manifestations of electrical injury: a case report and review of the literature. CLAO J. 2002;28:224-7.
5. Espaillat A, Janigian R, King T. Cataract, bilateral macular holes, and rhegmatogenous retinal detachment induced by lightning. Am J Ophthalmol 1999;127:216-7.
6. Rivas-Aguiño PJ, Garcia RA, Arevalo JF. Bilateral macular cyst after lightning visualized with optical coherence tomography. Clin Experiment Ophthalmol 2006;34:893-4.
7. Jain S, Bandi V. Electrical and lightning injuries. Crit Care Clin 1999;15:319-31.
8. Grover S, Goodwin J. Lightning and electrical injuries: Neuro-ophthalmologic aspects. Semin Neurol 1995;15:335-41.
9. Lee R, Aarsvold J, Chen W, et al. Biophysical mechanisms of cell membrane damage in electrical shock. Semin Neurol 1995;15:367-74. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in