|
|
 |
 |
 |
 |
|
|
Concurrent endophthalmitis and orbital cellulitis in a child with congenital glaucoma and a glaucoma drainage device
Digital Journal of Ophthalmology
2011
Volume 17, Number 4
November 6, 2011
DOI: 10.5693/djo.02.2011.10.002
|
Printer Friendly
Download PDF |
|
|


 Faazil Kassam, MD
Faazil Kassam, MD | Department of Ophthalmology, University of Alberta, Canada Bonita Lee, MD, FRCP(C), MSc (Epi) | Department of Pediatrics, University of Alberta, Canada Karim Damji, MD, FRCS(C), MBA | Department of Ophthalmology, University of Alberta, Canada
|
|
|
| Abstract | | A 3-year-old monocular boy with a history of congenital glaucoma and aqueous shunt implantation presented with periorbital swelling, erythema, and purulent discharge in his seeing right eye. Examination revealed an extensive hypopyon. Computed tomography (CT) showed right-sided proptosis, and a displaced aqueous shunt device deep in the orbit. Significant purulent fluid was encountered when the device was removed; vitreous and orbital cultures revealed Streptococcus pneumoniae. The patient received intravitreal, topical, intravenous, and oral antibiotics as well as intraocular tissue plasminogen activator and topical steroid. Orbital and intraocular inflammation decreased significantly but he developed a cataract, further complicated by a retinal detachment. | | | Case Report | A 3-year-old monocular boy with a history of congenital glaucoma presented to the ophthalmology clinic at the Royal Alexandra Hospital in May 2011 with purulent discharge from his seeing right eye associated with periorbital swelling and erythema. The patient had a routine examination by his pediatric ophthalmologist 2 days prior. At the time, red reflex and retinoscopy streak in his right eye was noted to be clear, but the examination was lengthy and difficult and attempts at a slit-lamp examination were unsuccessful. He presented to the emergency room the next day complaining of severe pain behind the right eye with no obvious eyelid swelling. Examination was limited since he was unwilling to open the eye, and he was referred to the ophthalmology clinic the next day. The parents denied a history of the patient rubbing his eye.
The family was of Turkish descent, and the patient’s paternal and maternal grandfathers were distant relatives. The patient’s older sister had also been diagnosed with congenital glaucoma and had received extensive treatment. Genetic testing found the patient to be autosomal recessive for the Cyp1B1 gene, which has been mapped to the 2p21 region and linked with primary congenital glaucoma.(1)
The patient had an extensive ophthalmic history, having been diagnosed with congenital glaucoma at birth and having undergone multiple bilateral trabeculectomies since 4 weeks of life. His left eye suffered from unresolved corneal haze since birth and was assumed to have no visual potential. Aggressive treatment in order to preserve vision in his right eye included a goniotomy in December 2008, the insertion of an Ahmed valve aqueous shunt (FP7, New World Medical Inc, Rancho Cucamonga, CA) in September 2010, and, most recently, a trimming of the tube (which was touching the cornea) via two corneal incisions in December 2010. The tube was last noted to be in normal position in the anterior chamber during a follow-up visit at the end of February 2011, 11 weeks before presenting to our clinic.
Blood cultures were drawn and an examination under anesthesia was performed with a vitreal tap and intravitreal injection of vancomycin, ceftazidime, and dexamethasone as well as injection of gentamicin subconjunctivally. The upper lid was found to be swollen and tense with an intact but chemotic and hyperemic conjunctiva superotemporally. The cornea was diffusely hazy and a hypopyon was present, clouding the entire anterior chamber. Two corneal 10-0 nylon sutures were removed, and the corneal incisions were intact; no leak was evident via the cornea or conjunctiva. There was no view of the lens or fundus. B-scan ultrasonography showed some vitreous debris with a flat retina (Figure 1A). An attempt was made to find the Ahmed valve via an anterior surgical approach using a large superotemporal peritomy, but neither the tube/reservoir complex nor the scleral patch graft could be located. Cultures were sent from the conjunctival discharge, the vitreous tap, and the sutures.
Subsequently, the patient was admitted and treated with empiric intravenous vancomycin and ceftazidime as well as topical gatifloxacin. A computed tomography (CT) scan of the orbits done the same day showed right-sided proptosis with the valve located superiorly and very posteriorly and ill-defined inflammatory changes in the extraconal fat (Figure 1B). No sinus opacification was noted. The following day the patient returned to the operating room, and the aqueous tube shunt was found deep in the orbit via a superotemporal peritomy with the assistance of an orbital surgeon. It was surrounded by dense fibrous adhesions, which were incised and followed back to find and remove the implant. Several pockets of purulent material were encountered during the dissection, and the valve mechanism also contained pus (Figures 2A-C). Tissue plasminogen activator (TPA) was injected intravitreally (25 mcg) as well as in the anterior chamber (25 mcg) to break up fibrin.
Blood cultures were negative, and the first vitreal cultures grew Streptococcus pneumoniae serotype 19A with intermediate resistance to penicillin and sensitive to moxifloxacin (MIC by E-test: 0.12 mg/L), levofloxacin (MIC: 0.50 mg/L), and linezolid (MIC: 1.0 mg/L). Cultures from the orbit at the time of the valve removal grew the same organism. The sutures, as well as conjunctival cultures did not grow any organisms. The patient received vancomycin for 1 week, followed by 3 weeks of oral levofloxacin and frequent topical gatifloxacin, atropine, and prednisolone acetate. Two weeks after the device removal, a repeat injection of TPA was given in the anterior chamber (25 mcg). An examination under anesthesia was repeated approximately 2 and 4 weeks later, showing marked improvement in the inflammation and clearing of the cornea (Figure 3A), although a dense cataract and partial vitreous detachment had developed. The cataract was removed with some difficulty given the residual corneal haze, and the patient subsequently developed a retinal detachment that required two vitreoretinal surgeries to successfully repair. Unfortunately, given the severity of the infection and the retinal complications that ensued following cataract removal, the patient’s visual function has remained poor. Recent examination did positively reveal, however, that he is able to perceive colors and locate 3 mm candy beads at a distance of 8 inches (20 cm). | |
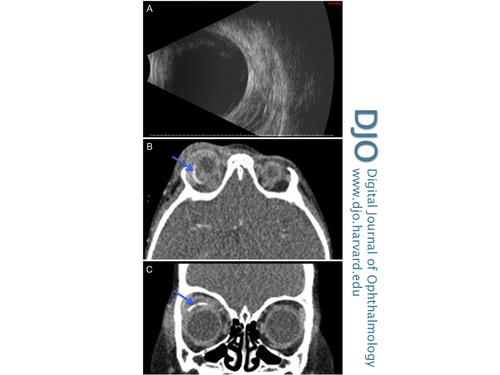
Figure 1
A, Initial B-scan ultrasound showing vitreous debris secondary to early endophthalmitis. B-C, CT scan showing right sided proptosis, inflammation of extraconal fat as well as Ahmed valve implant located superiorly in orbit (arrows).
|
|
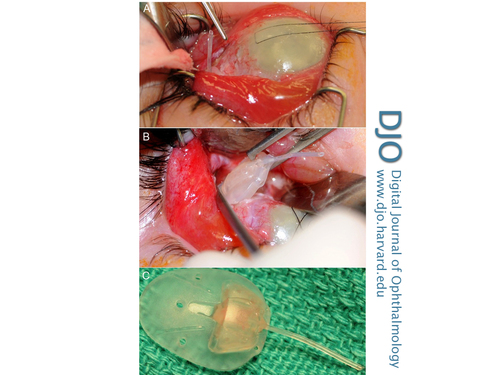
Figure 2
A, Supertemporal dissection exposing Ahmed valve tube buried deep in the orbit and diffusely cloudy cornea. B, Removal of the Ahmed valve device showing associated purulent discharge. C, Purulent discharge evident in the removed device.
|
|
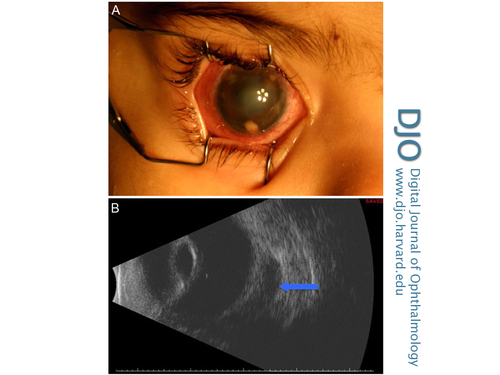
Figure 3
A, Examination under anesthesia 2 weeks following valve removal and antimicrobial therapy showing significant improvement in clearing of the cornea and anterior chamber. An opacity within the pupil can be seen representing a cataract. B, B-scan ultrasound 4 days after device removal showing relatively clear vitreous cavity with collection located posteriorly behind globe (arrow).
|
|
| Discussion | Cases of concurrent orbital cellulitis and endophthalmitis in adults have been reported in the literature.(2-6) In children, there have been cases of endophthalmitis and orbital cellulitis independently following placement of aqueous shunt devices.(7-10) This case is unique involving concurrent orbital cellulitis and endophthalmitis in association with an aqueous shunt device in a child who was monocular and had congenital glaucoma.
The child had been examined 2 days prior by a pediatric ophthalmologist and no evidence of infection was present. There are several possible pathways for the development of this rapidly progressive infection. First, organisms could have gained entry into the eye via the ocular surface, leading to endophthalmitis followed by orbital cellulitis through discharge via the tube, inflammation, and enzymatic degradation resulting in dislocation of the device. This is the most likely possibility, although corneal wounds were sealed, suture cultures were negative, and there was no obvious erosion anteriorly over the tube or valve site.
Second, orbital cellulitis caused by sinusitis could have led to endophthalmitis, although this is unlikely since the CT scan demonstrated no infection in the ethmoid sinus and only minimal thickening in the maxillary sinus. Third, an initial displacement in the valve via an unknown minor trauma may have also caused hypotony of the eye with inspissation of secretions, precipitating the infection. The last possibility, endogenous spread of the infection, is the least likely since the child had no systemic signs of septicemia and his blood cultures were negative.
There is limited data on the use of systemic antibiotics in the treatment of endophthalmitis, with the main clinical trial completed in the context of infections related to cataract surgery in adults that have different microbial pathogens (most frequently coagulase-negative staphylococcus).(11) Levofloxacin was chosen for this case based on the availability of pediatric dosing recommendations (not available for moxifloxacin), MIC results, and evidence of good systemic and vitreous penetration.(12) Linezolid was not chosen since it has been associated with optic neuropathy.(13) Duration of therapy was governed by the presence of orbital cellulitis and a collection posterior to the orbit seen on B-scan ultrasonography 4 days after removal of the device (Figure 3B). Small case series of post-bleb endophthalmitis with and without shunt devices seemed to suggest that pneumococcus is more prevalent in children than in adults.(9,14,15) Of interest is the inclusion of the S. pneumoniae serotype 19A in the 13-valent pneumococcal vaccine(16); this patient received three doses of the 7-valent conjugated pneumonococcal vaccine in infancy and was due to receive the 13-valent vaccine, which was incorporated in July 2010 in the provincial immunization schedule, at his preschool vaccination in 2012.(17)
Following the patient’s course of intravenous vancomycin and oral levofloxacin, the patient improved significantly with respect to the orbital reaction as well as decreased inflammation in the anterior chamber and marked clearing of the corneal haze. The addition of TPA soon after the diagnosis may have assisted in clearing fibrin within the anterior chamber and vitreous cavity.
Acknowledgments
The authors thank Dr. Brad Hinz, Dr. Ezekiel Weis, Dr. Matthew Tennant, and Dr. Bonnieca Islam for their assistance and consultation in the management of this case and Dr. Michelle Noga for her assistance in reviewing and providing the computed tomography images. | | | References | 1. Sarfarazi M, Stoilov I, Schenkman JB. Genetics and biochemistry of primary congenital glaucoma. Ophthalmol Clin North Am 2003;16:543-54.
2. Decock C, Claerhout I, Kestelyn P, Van Aken EH. Orbital cellulitis as complication of endophthalmitis after cataract surgery. J Cataract Refract Surg 2010;36:673-5.
3. Argelich R, Ibáñez-Flores N, Bardavio J, et al. Orbital cellulitis and endogenous endophthalmitis secondary to Proteus mirabilis cholecystitis. Diagn Microbiol Infect Dis 2009;64:442-4.
4. Limaiem R, Merdassi A, Lahdhiri I, et al. Orbital cellulitis and endophthalmitis after cataract surgery. Bull Soc Belge Ophthalmol 2008;309-310:27-30.
5. Luemsamran P, Pornpanich K, Vangveeravong S, Mekanandha P. Orbital cellulitis and endophthalmitis in pseudomonas septicemia. Orbit 2008;27:455-7.
6. Lip PL, Moutsou M, Hero M. A postoperative complication far worse than endophthalmitis: the coexistence of orbital cellulitis. Br J Ophthalmol 2001;85:631-2.
7. Bayraktar Z, Kapran Z, Bayraktar S, et al. Delayed-onset streptococcus pyogenes endophthalmitis following Ahmed glaucoma valve implantation. Jpn J Ophthalmol 2005;49:315-7.
8. Al-Torbak AA, Edward DP. Delayed endophthalmitis in a child following an Ahmed glaucoma valve implant. J AAPOS 2002;6:123-5.
9. Al-Torbak AA, Al-Shahwan S, Al-Jadaan I, et al. Endophthalmitis associated with the Ahmed glaucoma valve implant. Br J Ophthalmol 2005;89:454-8.
10. Chaudhry IA, Shamsi FA, Morales J. Orbital cellulitis following implantation of aqueous drainage devices. Eur J Ophthalmol 2007;17:136-40.
11. Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study: a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol 1995;113:1479-96.
12. George JM, Fiscella R, Blair M, et al. Aqueous and vitreous penetration of linezolid and levofloxacin after oral administration. J Ocul Pharmacol Ther 2010;26:579-86.
13. Linezolid. In: DRUGDEX Evaluations [Internet database]. Greenwood Village, Colo: Thomson Reuters (Healthcare) Inc. Updated periodically.
14. Al-Turki TA, Al-Shahwan S, Al-Mezaine HS, et al. Microbiology and visual outcome of bleb-associated endophthalmitis. Ocul Immunol Inflamm 2010;18:121-6.
15. Leng T, Miller D, Flynn HW Jr, et al. Delayed-onset bleb-associated endophthalmitis (1996-2008): causative organisms and visual acuity outcomes. Retina 2011;31:344-52.
16. Paradiso, PR. Advances in pneumococcal disease prevention: 13-valent pneumococcal conjugate vaccine for infants and children. Clin Infect Dis 2011;52:1241-7.
17. Government of Alberta—Alberta Health and Wellness. Immunization: pneumococcal vaccine. Available at: http://www.health.alberta.ca/health-info/imm-pneumococcal.html. Accessed June 2011. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in