|
|
 |
 |
 |
 |
|
|
Post-LASIK ectasia treated with intrastromal corneal ring segments and corneal crosslinking
Digital Journal of Ophthalmology
2013
Volume 19, Number 1
January 6, 2013
DOI: 10.5693/djo.02.2012.10.001
|
Printer Friendly
Download PDF |
|
|


 Kay Lam, MD
Kay Lam, MD | Department of Ophthalmology, University of Toronto Dan B. Rootman, MSc, MD | Department of Ophthalmology, University of Toronto Alejandro Lichtinger, MD | Department of Ophthalmology, University of Toronto David S. Rootman, MD, FRCSC | Department of Ophthalmology, University of Toronto
|
|
|
| Abstract | | Corneal ectasia is a serious complication of laser in situ keratomileusis (LASIK). We report the case of a 29-year-old man who underwent LASIK in both eyes and in whom corneal ectasia developed in the left eye 3 years after surgery. He was treated sequentially with intraocular pressure–lowering medication, intrastromal corneal ring segment (ICRS) implants, and collagen crosslinking. Vision improved and the ectasia stabilized following treatment. Combined ICRS implantation and collagen crosslinking should be considered early in the management of post-LASIK ectasia. | | | Introduction | | Corneal ectasia is a serious vision-threatening complication of laser in situ keratomileusis (LASIK).(1) It is associated with progressive corneal steepening, an increase in myopia and astigmatism, and decrease in uncorrected visual acuity. These cases can be managed with lamellar or penetrating keratoplasty; however, minimally invasive techniques are also possible. These options include medication to reduce intraocular pressure (IOP),(2) rigid gas-permeable contact lenses, intrastromal corneal ring segments (ICRSs),(3-5) and corneal crosslinking with ultraviolet radiation and riboflavin treatment.(6) | | | Case Report | A 32-year-old man presented at Yonge Eglinton Laser Eye Centre with a complaint of deteriorating and variable visual acuity of several weeks' duration. His medical history was remarkable for LASIK surgery 3 years earlier. On preoperative examination, his best-corrected visual acuity had been 20/20, with a manifest refraction of −6.00 −0.50 x 10 in the right eye and −7.00 −0.50 x 180 in the left eye. Slit-lamp examination and fundus examination were normal. The preoperative topography had revealed no significant irregularities. Keratometry was 47.40/45.42 D in the right eye and 45.92/46.68 D in the left. Preoperative central ultrasound pachymetry was 523 um in the right eye and 525 um in the left eye. He had had no prior ocular surgeries or family history of ocular disease, including keratoconus. Both eyes had underwent uneventful LASIK with IntraLase (Abbott Laboratories Inc, Abbott Park, IL) femtosecond laser flap construction. The ablation zone was 5.0 mm, with a transition zone of 8.5 mm and a superior-based 100 ì flap in both eyes. Ablations of 123.5 um and 140 um were performed, with a targeted residual total thickness of 399.5 um in the right eye and 385 um in the left eye. By day 14, uncorrected visual acuity was 20/20 in both eyes. He had had no complications at 1 month and 6 months' follow-up.
On ophthalmological examination at presentation, uncorrected visual acuity was 20/20 in the right eye and 20/250 in the left eye. Manifest refraction was −3.00 −2.00 x 162 in the left eye, resulting in a best-corrected visual acuity of 20/60, and −0.05 −2.50 x 149 in the right eye. Figure 1 shows the curvature with marked central corneal steepening in the left eye. The keratometry was 46.17/43.44 D in the right eye and 49.20/45.61 D in the left eye, with central corneal thickness (CCT) of 396 um in the right eye and 374 um in the left eye. Attempts to lower the patientfs IOP with brimonidine on the left showed no change in corneal topography. ICRSs (Intacs; Addition Technology, Sunnyvale, CA) were implanted in the left eye using the femtosecond laser for tunnel creation. Two standard segment implants of 400 um (7.0 mm optical zone) were placed at axis 60, with a tunnel depth of 400 um. The implants resulted in some improvement (see Table 1 for visual and keratometric results), but the patient still experienced variable visual acuity. Post-ICRS topography is shown in Figure 2. As a result of these concerns, 10 months after ICRS insertion, the ectatic left cornea was treated with combined ultraviolet radiation and riboflavin treatment to achieve collagen crosslinking. At 7 months after treatment, his uncorrected visual acuity improved from 20/60 to 20/25; his best-corrected visual acuity, from 20/30 to 20/20. His refraction changed from −6.50 + 2.50 x 180 to +0.25 + 1.00 x 30. Changes in the patient's corneal topography are given in Table 1 and Figure 3. The right eye remained stable throughout treatment. Figure 4 shows the difference maps to reflect the treatmentfs effect after ICRS and crosslinking procedures. | |
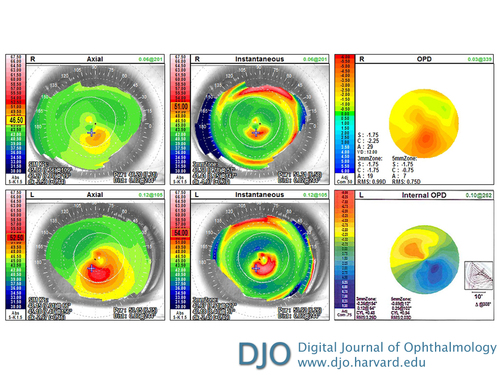
Figure 1
Corneal topography in the left eye at presentation, 3 years after myopic LASIK.
|
|
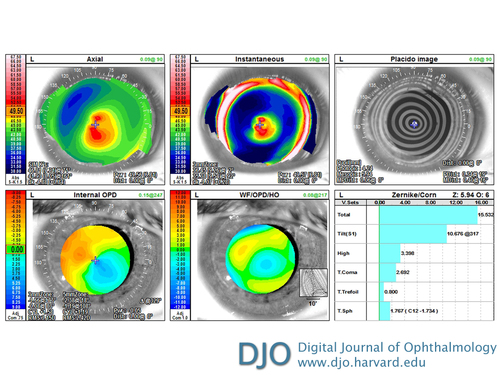
Figure 2
Corneal topography in the left eye 7.5 months post-Intacs implantation.
|
|
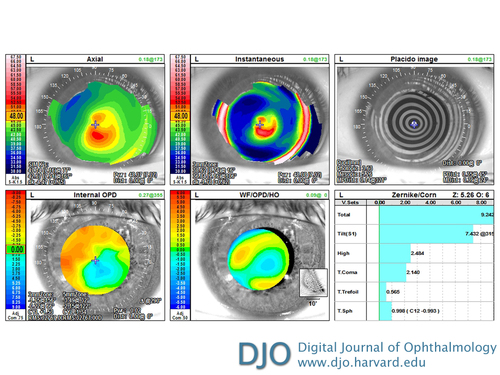
Figure 3
Corneal topography 7 months after collagen crosslinking in the left eye.
|
|
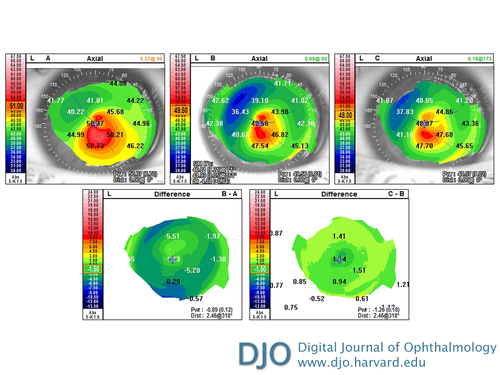
Figure 4
Corneal difference in the left eye (preoperative minus postoperative, after Intacs and collagen crosslinking procedures).
|
|
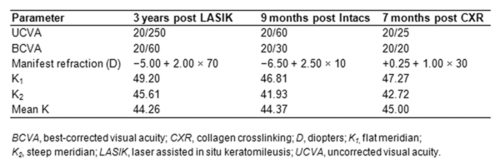
Table 1
Visual, refractive, and keratometric parameters in the left eye on presentation, after ICRS implantation, and after collagen cross-linking.
|
|
| Discussion | Iatrogenic corneal ectasia after LASIK is one of the most feared complications of refractive surgery.(7) This progressive corneal distortion can result in progressive myopia, irregular astigmatism, and visual impairment.(8) Rigid contact lenses are frequently required to achieve good functional vision, but ectatic progression can lead to intolerance of contact lenses, and ultimately the patients may require lamellar or penetrating keratoplasty. The use of Intacs for post-LASIK ectasia has been previously reported with positive results.(4,5,9,10) Treatment of post-LASIK ectasia with crosslinking procedures has also shown promise.(6,11)
Combined Intacs and collagen crosslinking treatment has been reported previously for one patient, who achieved a stable best-corrected visual acuity of 20/25.(12) Combined ICRS implantation and collagen crosslinking produced a dramatic, stable visual outcome in our patient. While IOP-lowering medication did not seem to improve our patient’s condition, we feel that, as a low-risk intervention with previously reported utility,(2) it may be worthwhile to attempt. The efficacy of this approach is clearly limited, however, and now we would generally consider more aggressive strategies at the outset. When our patient presented, crosslinking therapy was not yet available, and IOP control as a temporizing measure seemed appropriate.
ICRS implantation in the corneal periphery flattens the central corneal apex,(3) while crosslinking induces additional covalent bonds between collagen molecules to increase corneal strength.(11) A patient receiving both treatments consecutively may receive the beneficial effects of improved corneal topography and stabilization of corneal ectasia. We believe that a stepwise progression from IOP-lowering medication to ICRS implantation to collagen crosslinking may be an appropriate treatment strategy for cases of post-LASIK corneal ectasia. We did not combine our treatment measures with photorefractive keratectomy (PRK), as described by Kanellopoulos in the Athens Protocol,(13) because we have had little experience with this modality and also because the long-term results of further corneal thinning and destabilization remain uncertain.
The combination of these two minimally invasive therapies, Intacs and crosslinking, for the treatment of post-LASIK ectasia appears to be a promising alternative to lamellar or penetrating lamellar keratoplasty. Longer follow-up and larger studies are needed to evaluate the refractive and topographic stability of these alternative and desirable treatment options. | | | References | 1. Randleman JB. Post-laser in-situ keratomileusis ectasia: current understanding and future directions. Curr Opin Ophthalmol 2006;17:406-12.
2. Hiatt JA, Wachler BS, Grant C. Reversal of laser in situ keratomileusis-induced ectasia with intraocular pressure reduction. J Cataract Refract Surg 2005;31:1652-5.
3. Alio J, Salem T, Artola A, et al. Intracorneal rings to correct corneal ectasia after laser in situ keratomileusis. J Cataract Refract Surg 2002;28:1568-74.
4. Kymionis GD, Tsiklis NS, Pallikaris AI, et al. Long-term follow-up of Intacs for post-LASIK corneal ectasia. Ophthalmology 2006;113:1909-17.
5. Siganos CS, Kymionis GD, Astyrakakis N, et al. Management of corneal ectasia after laser in situ keratomileusis with INTACS. J Refract Surg 2002;18:43-6.
6. Kymionis GD, Diakonis VF, Kalyvianaki M, et al. One-year follow-up of corneal confocal microscopy after corneal cross-linking in patients with post laser in situ keratosmileusis ectasia and keratoconus. Am J Ophthalmol 2009;147:774-78.
7. Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg 1998;14:312-7.
8. Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology 2003;110:267-75.
9. Carrasquillo KG, Rand J, Talamo JH. Intacs for keratoconus and post-LASIK ectasia: mechanical versus femtosecond laser-assisted channel creation. Cornea 2007;26:956-62.
10. Pokroy R, Levinger S, Hirsh A. Single Intacs segment for post-laser in situ keratomileusis keratectasia. J Cataract Refract Surg 2004;30:1685-95.
11. Kanellopoulos AJ. Post-LASIK ectasia. Ophthalmology 2007;114:1230.
12. Kamburoglu G, Ertan A. Intacs implantation with sequential collagen cross-linking treatment in postoperative LASIK ectasia. J Refract Surg 2008;24:S726-9.
13. anellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the Athens protocol. J Refract Surg 2011;27:323-31. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in