|
|
 |
 |
 |
 |
|
|
Pigment deposition on the central aspect of the posterior lens capsule in pigmentary dispersion syndrome
Digital Journal of Ophthalmology
2011
Volume 17, Number 4
November 30, 2011
DOI: 10.5693/djo.02.2011.10.003
|
Printer Friendly
Download PDF |
|
|


 Shubha Nagarajaiah, MBBS, DO
Shubha Nagarajaiah, MBBS, DO | Department of Ophthalmology, Wolverhampton Eye Infirmary, New Cross Hospital, Wolverhampton, United Kingdom Georges Adrien Shun-Shin, FRCOphth, FRCS, DO, MBBS | Department of Ophthalmology, Wolverhampton Eye Infirmary, New Cross Hospital, Wolverhampton, United Kingdom
|
|
|
| Abstract | | We describe a case of an increasing pigmentary plaque on the posterior surface of the lens during follow-up of a case of pigment dispersion syndrome and suggest that this is a new sign of pigment dispersion. | | | Introduction | | In 1958 Scheie and Fleischhauer described the five features of pigment dispersion syndrome (PDS), namely, Krukenberg spindle, speckling of the anterior iris with pigment, pigmentation of the trabecular meshwork, atrophy of the iris, and pigment of the posterior lens surface near the equator.(1) | | | Case Report | In 1988 a 53-year-old, highly-myopic, white woman was referred to the Wolverhampton Eye Infirmary for a right eye floater. There was no history of previous blunt trauma to the eye. She was a known diabetic and was on oral hypoglycemic medications. On ophthalmological examination, best-corrected visual acuity was 6/9 in the right eye and 6/6 in the left eye. Bilateral Krukenberg spindles were noted on the cornea with pigment deposits on the posterior surface of the lens in both eyes (Figure 1). Intraocular pressure (IOP), measured by Goldmann applanation tonometry, was 14 mm Hg in each eye. Discs were healthy and not cupped. There was no evidence of diabetic retinopathy. Posterior vitreous face detachment was diagnosed in the right eye. She was reexamined once and discharged from follow-up.
She was referred back in 1997 with blurring of vision in the right eye. She was now on insulin for diabetes and was otherwise well. On examination, visual acuity was 6/18 in the right eye and 6/9 in the left eye. Anterior segment examination did not show any new changes. IOP was 19 mm Hg in the right eye and 17mm Hg in the left eye. There were drusen at both maculae associated with mild pigmentary changes. Visual fields by standard automated perimetry were normal. Fluorescein angiography confirmed dry, age-related macular degeneration. Electroretinogram (to exclude siderosis from a retained intraocular foreign body) and visual evoked potentials were normal. She was then seen intermittently in the outpatient clinic. Her IOPs were always <20 mm Hg.
She was referred again in 2002 complaining of deteriorating vision in her right eye. She was now hypertensive and was on anti-hypertensive medication. On examination, visual acuity was counting fingers in the right eye and 6/9 in the left eye. Bilateral Krukenberg spindles were still noted. There were multiple slitlike areas of transillumination on the left iris. There was a dense, brunescent cataract, with no view of the fundus in the right eye. There was a minimal left cataract. A dense pigment plaque was seen on the left posterior capsule (Figure 2). Compared to photographs from 1988, there was a distinct change in the shape of the plaque. It appeared to have regressed centrally and increased in size peripherally. There was no left diabetic retinopathy and a left posterior vitreous face detachment was noted. IOP was 17 mm Hg in the right eye and 19 mm Hg in the left eye. Gonioscopy showed a bilateral concave peripheral iris and a wide open pigmented angle. Visual fields were normal again. Unfortunately, the patient was subsequently lost to follow-up. | |

Figure 1
Clinical photograph (1988) of the left eye of a 53-year-old woman showing corneal Krukenberg spindles and pigment deposits on the posterior capsule of the lens.
|
|
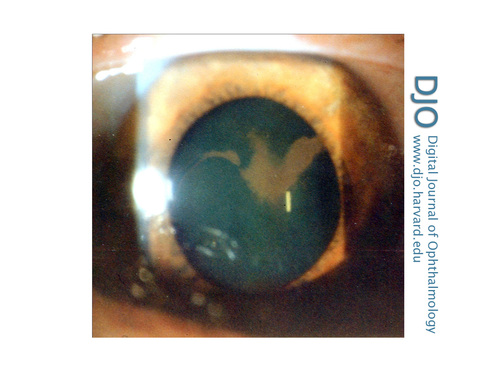
Figure 2
Slit-lamp photograph (2002) of the left eye of the same patient at age 67 showing significant change in shape of pigment deposits, which appeared to have regressed centrally and increased peripherally compared to the earlier photograph.
|
|
| Discussion | In 1938 Zentmayer described annular pigmentation of the lens.(2) Scheie and Fleischhauer noted an incomplete ring on the posterior surface of the lens in 14 eyes and a complete ring in 12 eyes.(1) Most eyes were examined by gonioscope, and it was observed that “the pigment frequently lodges in the angle between the face or anterior limiting membrane of the vitreous and the periphery of the posterior surface of the lens,” that is, at Wieger’s ligament. This pigment line now called “Scheie’s line.”(3)
In pigment dispersion syndrome, pigment release is thought to occur as a result of posterior-bowing of the mid-peripheral iris rubbing against the lens zonules.(4) This unusual iris configuration may be due to a type of “reverse pupil block,” which prevents pressure equalization between the anterior and posterior chambers, leading to transient rise in the IOP in the anterior chamber relative to the posterior. Prevention of blinking causes reversal of iris configuration.(5) Lance Liu et al have reported that the iris remains planar with continuous blinking and controlled accommodation and that the posterior curvature of the iris is induced and probably maintained by accommodation.(6)
During Nd:YAG iridotomy for PDS, pigment can be seen to flow backward into the posterior chamber and the iris periphery flattens, suggesting that the anterior chamber pressure is greater. It is known that pigment can flow freely from anterior to posterior chambers.(7) Little has shown that lens fragments during uncomplicated phacoemulsification can find their way into Berger’s space,(8) that is, the space between the anterior hyaloid and posterior lens capsule if there is disruption to Wieger’s ligament. Naumann has commented that blood can reach the retrolenticular space in blunt trauma via a break in Wieger’s ligament.(9)
It has been suggested that in PDS, the presence of Scheie’s line demonstrates that there is some flow of pigment from the anterior to the posterior chamber. If there is a break in Wieger’s ligament, then it is conceivable that pigment could flow in Berger’s space and accumulate there.. In our case, pigment accumulated in Berger’s space, which is central, as opposed to the space near Wieger’s ligament, which is peripheral. The fluid is continuing to flow since the shape of the plaque has changed over the years, a further unusual sign, we suggest, of pigmentary glaucoma. | | | References | 1. Scheie HG, Fleischhauer HW. Idiopathic atrophy of the epithelial layers of the iris and ciliary body. Arch Ophthalmol 1958;59:216-28.
2. Zentmayer W. Association of an annular band of pigment on the posterior capsule of the lens with a Krukenberg spindle. Arch Ophth 1938;20:52-7.
3. Campbell DG, Schertzer RM. Pigmentary glaucoma. In: Ritch R, Shields MB, and Krupin T, eds. The Glaucomas. St Louis: Mosby; 1996:975-91.
4. Campbell DG. Pigmentary dispersion and glaucoma: a new theory. Arch Ophthalmol 1979;97:1667-72.
5. Liebmann JM, Tello C, Chew SJ, et al. Prevention of blinking alters iris configuration in pigment dispersion syndrome and in normal eyes. Ophthalmology 1995;102:446 -55.
6. Liu L, Ong EL, Crowston J. The concave iris in pigment dispersion syndrome. Ophthalmology 2011;118:66-70.
7. Babalola OE, Murdoch IE. Free floating melanin particles in the anterior chamber: a normal finding in African eyes. Eye 2003;17:410-4.
8. Little B. Bits in Berger’s space. Video J Cataract Refract Surg 19;2003.
9. Naumann GOH. Correspondence. Photographs of intralenticular hemorrhage following blunt ocular trauma. Arch Ophthalmol 1999;117:549.
| |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in