|
|
 |
 |
 |
 |
|
|
Idiopathic pupillary capture 7 years after extracapsular cataract extraction and intraocular lens implantation
Digital Journal of Ophthalmology
2011
Volume 17, Number 3
August 16, 2011
DOI: 10.5693/djo.02.2011.06.001
|
Printer Friendly
Download PDF |
|
|


 Juan A. Ramos, MD
Juan A. Ramos, MD | Department of Internal Medicine, Westchester Medical Center, Valhalla, New York Venancio Jurado, MD* | Department of Ophthalmology, Centro Policlínico Valencia, Avenida Carabobo, La Vina, Valencia, Venezuela
|
|
|
| Abstract | | Pupillary capture is a pathology commonly associated with traumatic or inflammatory processes of the eye. We present a case of idiopathic pupillary capture, 7 years after extracapsular cataract extraction and intraocular lens implantation. This case highlights the need for ongoing patient surveillance, especially in elderly patients who are less able to detect subtle changes in their vision. | | | Introduction | | Extracapsular cataract extraction (ECCE) with intraocular lens (IOL) implantation is one of the most common ophthalmologic surgical procedures in the United States and worldwide.(1-3) An uncommon complication is pupillary capture, or entrapment. Pupillary capture occurs when part of the pupil margin is displaced posteriorly behind the IOL, which then appears to lie in the anterior chamber.(4) Pupillary capture is typically noted as an early postoperative event, although a late form is also recognized.(4,5) It is generally attributed to inflammatory processes within the eye, such as endophthalmitis, iritis, blunt trauma, or YAG laser treatment.(5-10) Its incidence has been reported as ranging from 3.1% to 8.95%.(5,10) We have found only one previous report of idiopathic pupillary capture.(5) The present case describes a subject with idiopathic pupillary capture 7 years after ECCE. | | | Case Report | A 67-year-old man presented in July 2010 to the Ophthalmology Clinic of the Centro Policlínico Valencia complaining of blurred vision in his left eye of 2 months’ duration. There was no history of medical illness. Pertinent ophthalmologic history included bilateral cataracts treated with ECCE and IOL implantation in 2003. Preoperative visual acuity was 20/125 in the right eye and counting fingers at 9 feet in the left eye. Postoperative best-corrected visual acuity was 20/30 in the right eye and 20/40 in the left eye, with no evidence of early or late perioperative endophthalmitis, iritis, pupillary capture, or wound leakage. The patient was seen annually in the eye clinic and maintained his postoperative visual acuity and remained disease free. His final eye clinical assessment was performed in 2006.
On examination in 2010 (Figure 1A), the patient’s visual acuity was 20/30 in the right eye and 20/125 in the left eye. Biomicroscopic examination of the left eye revealed posterior capsule opacification and pupillary capture with abundant iridocapsular synechiae formation. Although the optic was displaced, the capsular bag’s location seemed to have been preserved. Some parts of the lens implant may have traveled outside the bounds of the capsular bag;(11) however, the authors were unable to determine whether or not this was the case during biomicroscopy. The patient denied any history of eye trauma, strenuous activity, or lifting associated with his clinical picture. Significant compromise of mydriatic capabilities was observed, making pharmacologic reversal impossible.
One week after presentation, surgical correction was performed. Under local and intramuscular anesthesia 2.5 mm incisions were performed at 3 and 9 o’clock. DuoVisc (Alcon Laboratories, Fort Worth, TX) viscoelastic material was injected, after which synechiolysis was performed and the lens repositioned. The IOL used was a three-piece Visiontech (ISO 9001, ISO 13485; Nova Lima, Minas Gerais,Brazil) CC16H2B. Miosis was then induced with carbachol intraocular solution. No intraoperative complications occurred, and there were no early or late postoperative complications (Figure 1B). The patient’s postoperative course was satisfactory, with visual acuity restored to 20/40. A dilated fundus examination 1 month after surgery showed posterior capsule opacification. | |
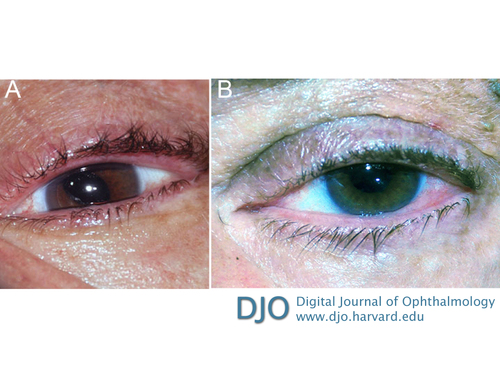
Figure 1
A, Photograph of patient’s left eye at presentation showing significant pupillary capture of the nasal pupillary border. B, Restored intraocular lens positioning and pupillary borders 1 month after surgery.
|
|
| Discussion | Pupillary capture is a documented complication of ECCE and IOL implantation. Most often it is associated with inflammation, either from infection or trauma of the eye.(5-10) Late pupillary capture is described as formation of iridocapsular adhesions from fibrous metaplasia of the lens epithelial cells and from inflamed or traumatized iris tissue.(12,13) It can also present spontaneously, as shown by this case. A possible, albeit unlikely, cause for the prior could be an excessively large capsulorhexis promoting proliferation of lens epithelial cells, leading to optic displacement.
This case is remarkable not only for its occurring 7 years after ECCE and IOL implantation but also for its idiopathic etiology. It highlights the need for ongoing postoperative follow-up of these patients, especially the elderly, many of whom may not spontaneously seek medical attention until visual acuity degrades. Health care workers and general practitioners should be familiar with cataract surgery and be able to screen patients on a regular basis to prevent complications such as the one described here. We recommend yearly ophthalmological follow-up in conjunction with the general practitioners’ routine care.
Literature Search
A PubMed was conducted, without date restriction, using the following terms: pupillary capture, pupillary capture causes, and idiopathic pupillary capture. The most recent articles identified by search were screened for relevance and similarity to the present case.
*The authors contributed equally to this case report.
Acknowledgments
The authors thank Dr. Armando Ramos for guidance on medical literature. | | | References |
1. Stark WJ, Terry AC, Worthen D, Murray GC. Update of intraocular lenses implanted in the United States. Am J Ophthalmol 1984;98:238-9.
2. Gogate PM. Small incision cataract surgery: complications and mini-review. Indian J Ophthalmol 2009;57:45-9.
3. Rao GN, Basti S, Vasavada AR, et al. Extracapsular cataract extraction: surgical techniques. Indian J Ophthalmol 1993;41:195-210.
4. Lindstrom RL, Herman WK. Pupil capture: prevention and management. J Am Intraocul Implant Soc 1983;9:201-4.
5. Lavin M, Jagger J. Pathogenesis of pupillary capture after posterior chamber intraocular lens implantation. Br J Ophthalmol 1986;70:886-9.
6. Obstbaum SA, To K. Posterior chamber intraocular lens dislocations and malpositions. Aust N Z J Ophthalmol 1989;17:265-71.
7. Hadid OH, Steel D. Pupillary capture of the haptic of an anterior chamber intraocular lens after blunt trauma. Can J Ophthalmol 2009;44:e27-8.
8. Leccisotti A. Traumatic pupillary capture of the haptic of an angle-supported phakic intraocular lens. J Cataract Refract Surg 2006;32:2133-4.
9. Park S, Ressiniotis T, Wood C. Intraocular lens pupillary capture after neodymium:YAG laser treatment of interlenticular opacification of posterior chamber piggyback intraocular lenses. J Cataract Refract Surg 2006;32:1056-8.
10. Rahman R, Rosen PH. Pupillary capture after combined management of cataract and vitreoretinal pathology. J Cataract Refract Surg 2002;28:1607-12.
11. Kurz GH. Histologic findings after successful posterior chamber lens implantation. J Cataract Refract Surg 1987;13:190-4.
12. Odrich MG, Hall SJ, Worgul BV, et al. Posterior capsule opacification: experimental analyses. Ophthalmic Res 1985;17:75-84.
13. Yeo JH, Jakobiec FA, Pokorny K, et al. The ultrastructure of an IOL “cocoon membrane.” Ophthalmology 1983;90:410-9. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in