|
|
 |
 |
 |
 |
|
|
Systemic non-Hodgkin's lymphoma involving the orbit and leptomeninges
Digital Journal of Ophthalmology
2010
Volume 16, Number 3
July 29, 2010
DOI: 10.5693/djo.02.2010.06.001
|
Printer Friendly
Download PDF |
|
|
|
|
|
|
| Abstract | | We report a case of diffuse large B-cell lymphoma in a 46-year-old female presenting in an unusual manner with stage IVB disease including concurrent orbital and leptomeningeal involvement. The cytologic features and cytogenetics of the malignancy are noted, and the management and progression of the disease, with attention to orbital involvement, is recorded for a period of over 2.5 years, until the patient’s death. | | | Case Report | A 46-year-old woman presented to our clinic with a complaint of intermittent proptosis, diplopia, and ptosis in her right eye for 4 months. During this period, she also noted a loss of balance, gait difficulties, and lower extremity weakness, numbness, and tingling. For the 6 months prior to presentation, she had also experienced weight loss and fatigue.
Ophthalmologic examination revealed visual acuities of 20/20 in both eyes. External examination demonstrated proptosis, soft tissue swelling in the upper and lower lids, and scleral “show” with mild conjunctival injection and chemosis in the right eye (Figure 1). Enlarged, matted, and non-tender cervical lymphadenopathy was also found. There was marked restriction of the right eye on adduction. The rest of the anterior and posterior segment examinations were unremarkable in both eyes. Neurological examination was pertinent for bilateral distal lower extremity motor and sensory deficits, diminished reflexes in the knees, and absent reflexes in the ankles. A Romberg test was positive.
Computed tomography of the head showed an enhancing soft tissue mass in the medial aspect of the right orbital fossa. MRI demonstrated an enhancing right orbital mass with intraconal and extraconal involvement, which communicated with the right ethmoid sinus. An MRI of the spine showed diffuse enlargement and enhancement of the lumbar and sacral nerve roots.
Biopsy of the left cervical lymph node (Figure 2) demonstrated diffuse large B-cell lymphoma (DLBCL). Diagnosis was confirmed with immunohistochemical stains that showed positive staining for B-cell markers CD19, CD20 (Figure 3) and lambda light chain restriction. Staining for CD3 and CD5 was negative, ruling out a T-cell lymphoma, small lymphocytic lymphoma/chronic lymphocytic leukemia, and mantle cell lymphoma; negative staining for CD10 ruled out a follicular lymphoma.(1) Furthermore, the BCL-1 stain showed heavy background staining, and definitive positivity was not ascertained, while fluorescence in situ hybridization of 100 cells did not show a [t(11;14)] rearrangement—a typical hallmark of mantle-cell lymphoma.(2) The Ki-67 proliferation index was 20% to 30%. Cytogenetic studies reported that all 7 cells studied showed monosomy for chromosome 1p and partial trisomy for the short arm and part of the long arm of chromosome 2, from the centromere to band 2q14.3. Cerebrospinal fluid cytology (Figure 4) was positive for malignant cells showing numerous atypical lymphocytes with a concurrent flow cytometry sample, which was positive for the same phenotypic profile of lymphoma. A bone marrow biopsy did not demonstrate evidence of lymphoma. Based on these findings, she was classified as stage IVB.
The patient was treated with 8 cycles of hyper-CVAD (fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) plus rituximab and intrathecal methotrexate, followed by central nervous system prophylaxis with liposomal Ara-C (cytarabine). About 2 months after the last cycle she had a recurrence in the medial portion of the right orbit (Figure 5). Orbitotomy and incisional biopsy confirmed recurrent DLBCL. Her cerebrospinal fluid at that time, however, was clear of malignant cells, and her nerve roots were no longer abnormal on imaging. While not confirmed by biopsy, the previous findings had been consistent with leptomeningeal involvement, which had improved clinically and radiologically with therapy. She was started on salvage chemotherapy with 4 cycles of RICE (rituximab, ifosfamide, carboplatin, and etoposide) and underwent 5 CyberKnife radiation treatments to the right orbit. One month after the last cycle, she had a recurrence in the right parotid gland, cervical lymph nodes, and a small persistent medial orbital lesion confirmed by PET/CT scan. Cerebrospinal fluid was again positive for malignant cells, and gene rearrangement studies showed a clonal population consistent with recurrent central nervous system DLBCL. Despite further salvage chemotherapy and intrathecal therapy, tumor progression was documented on the latest MRI report, including involvement of the lateral wall of the orbit and lacrimal gland. She died about 2.5 years after the diagnosis of her metastatic disease. | |

Figure 1
Facial image showing right eye proptosis, inferior scleral show, and right upper and lower lid swelling.
|
|
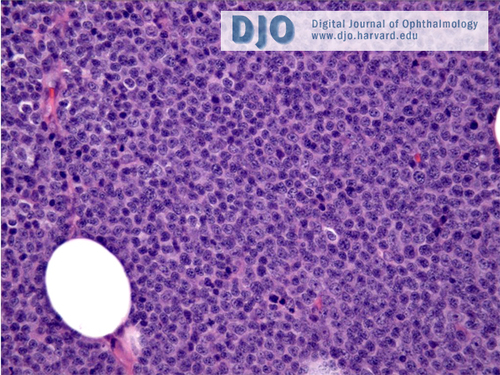
Figure 2
Left cervical lymph node biopsy showing a diffuse, large B-cell lymphoma. Effacement of nodal architecture by a diffuse proliferation of medium-to-large atypical lymphoid cells and abundant, mature small lymphocytes interspersed throughout the lymph node. (Hematoxylin and eosin stain, 100×).
|
|

Figure 3
Left cervical lymph node. Diffuse CD20-positive membranous stain of this large B-cell lymphoma. (CD20 immunohistochemical stain, 40×).
|
|
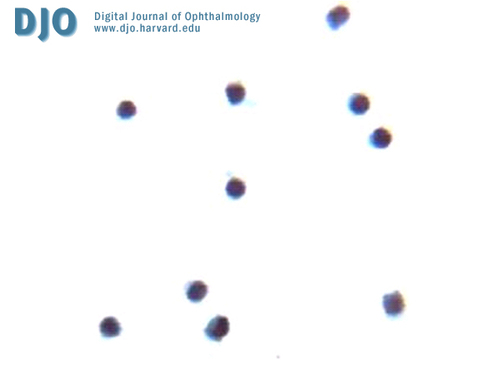
Figure 4
Cerebrospinal fluid (CSF) cytology. The CSF shows malignant lymphoma cells present. Flow cytometry of CSF was positive for a clonal lambda restricted B-cell lymphoma involving the CSF. (Papanicolaou stain, 400×).
|
|

Figure 5
Axial, T1-weighted MRI of the brain and orbits with gadolinium. A 4.8 × 2.4 × 3.9 cm homogenous, mildly enhancing mass is seen involving the medial extraconal space of the right obit with prominent exophthalmos.
|
|
| Discussion | The differential diagnosis of an orbital mass lesion is extensive. For the presentation described in this case, the differential is narrowed to mass lesions of the orbit with the potential for systemic involvement that would present in a woman in her fifth decade of life. These include metastatic disease, such as breast, lung, and renal cancers; lymphoid lesions, such as non-Hodgkin’s lymphoma;(3) and inflammatory lesions, such as orbital pseudotumor, sarcoid, or vasculitides. More rarely, an infectious etiology should also be considered.
When considering all lymphomas of the ocular adnexa (eyelid, conjunctiva, lacrimal gland, orbit) mucosa-associated lymphoid tissue (MALT) type is the most common, occurring in 44% to 67% of cases. The second most common type is either follicular, 12% to 23%, or DLBCL, 7% to 21%, depending on the study.(4-9) The frequency of ocular adnexal lymphoma with localization to the orbit has been cited as 54%.(5) It has been suggested that it may be more appropriate to analyze ocular adnexal lymphomas based on primary or secondary adnexal involvement. A study by McKelvie et al. of 73 patients with ocular adnexal lymphoproliferative disease found that follicular and DLBCL are the most common causes of secondary adnexal lymphomas.(5) A review article by Coupland et al. found that for secondary ocular adnexal lymphoma, follicular type is most common (33%-66%) followed by (in approximate decreasing frequency) multiple myeloma/plasmacytoma, lymphoplasmocytic lymphoma/immunocytoma, mantle cell lymphoma, DLBCL, Burkitt lymphoma, MALT lymphoma and chronic lymphocytic leukemia.(10)
To our knowledge, this is the first description of a case of systemic non-Hodgkin’s lymphoma with concurrent orbital and leptomeningeal involvement. Lymphoma is the most common orbital malignancy, has a predilection for the elderly, and classically presents as painless proptosis or adenexal swelling over a duration of 5-7 months.(7,9) Non-Hodgkin’s lymphoma is reported(11) to have an orbital presentation in 2.4% of all non-Hodgkin’s lymphoma cases, while its prevalence is about 5% in systemic NHL.(9) According to Liang et al., the incidence of secondary central nervous system lymphoma in a patient with orbital non-Hodgkin’s lymphoma is 5.9%,(12) and the most common form of central nervous system involvement in lymphoma is leptomeningeal metastasis.(13)
Chromosomal imbalance studies of lymphoid tumors are still in the early stages of development and classification. Previous comparative genomic hybridization studies of DLBCL are complex and frequently detect 5-6 aberrations in each case.(14) A well known example of chromosomal translocation in DLBCL is t(3;14)(q27,q32) in which the oncogene BCL6 is translocated to the vicinity of an Ig heavy-chain gene, causing an increased expression of the oncogene.(14) In a study by Coupland et al. lymphoma-related death occurred more often with tumors demonstrating large growth fractions as well as increased blast percentage with positivity for p21, p53, pRB and negativity for p16.(8) A loss of p16/INK4 expression has also been described as associated with lymphoma progression in DLBCL.(8) Our case did not demonstrate any gene rearrangements previously described as a risk factors for lymphoma progression or survival time.
Our patient presented with stage IVB disease, which is defined as multiple or disseminated foci of involvement of one or more extralymphatic organs or sites with or without lymphatic involvement. All stages are further divided on the basis of the absence (A) or presence (B) of systemic symptoms. The overall risk of lymphoma related death secondary to DLBCL has been reported as 38%, however a recent study by Madge et al. of ocular adnexal DLBCL found that in 11 patients with concurrent systemic disease at presentation, 5-year Kaplan-Meier survival estimates were 36%.(5,15) Our patient presented with simultaneous orbital and leptomeningeal involvement, perhaps a unique presentation. Having a high clinical suspicion and early diagnosis and intervention is important in orbital lymphoma cases since there have been reports stating prior or concurrent systemic disease as being the most significant predictive factor for lymphoma-related deaths.(16)
Literature Search
A thorough PubMed search for English-language articles was performed using the following terms: non-hodgkin’s lymphoma, diffuse large B-cell lymphoma, orbit, leptomeningeal carcinomatosis, central nervous system, and meningitis. | | | References | 1. Silverberg, SG, et al. Silverberg’s Principles and Practice of Surgical Pathology and Cytopathology. Churchill Livingstone Elsevier, 2006:508-9.
2. Li, Jian-Yong, et al. Detection of Translocation t(11;14)(q13;q32) in Mantle Cell Lymphoma by Fluorescence in Situ Hybridization. Am J Pathol 1999;154:1449-52.
3. Shields J, Shields C, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions. Ophthalmology 2004;111:997-1008.
4. Hatef E, Roberts D, McLaughlin P, Pro B, Esmaeli B. Prevalence and nature of systemic involvement and stage at initial examination in patients with orbital and ocular adnexal lymphoma. Arch Ophthalmol 2007;125:1663-7.
5. McKelvie PA, McNab A, Francis IC, Fox R, O’Day. Ocular adnexal lymphoproliferative disease: a series of 73 cases. J Clin Experiment Ophthalmol 2001;29:387-93.
6. Auw-Haedrich C, Coupland SE, Kapp A, et al. Long term outcome of ocular adnexal lymphoma subtyped according to the REAL classification. Revised European and American Lymphoma. Br J Ophthalmol 2001;85:63-9.
7. Ferry JA, Fung CY, Zukerberg L, et al. Lymphoma of the ocular adnexa: a study of 353 cases. Am J Surg Pathol 2007;31:170-84.
8. Coupland SE, Hellmich M, Auw-Haedrich C, Lee WR, Stein H. Prognostic value of cell-cycle markers in ocular adnexal lymphoma: an assessment of 230 cases. Graefes Arch Clin Exp Ophthalmol 2004; 242:130-45. Epub 2003 Dec 18.
9. Sullivan TJ, Whitehead K, Williamson R, et al. Lymphoproliferative disease of the ocular adnexa: a clinical and pathologic study with statistical analysis of 69 patients. Ophthal Plast Reconstr Surg 2005; 21:177-88.
10. Coupland SE, Damato B. Lymphomas involving the eye and the ocular adnexa. Curr Opin Ophthalmol 2006;17:523-31.
11. Lazzarino M, Morra E, Rosso R, et al. Clinicopathologic and immunologic characteristics of non-Hodgkin’s lymphomas presenting in the orbit: A report of eight cases. Cancer 1985; 55:1907-12.
12. Liang RH, Woo EK, Yu YL, et al. Central nervous system involvement in non-Hodgkin’s lymphoma. Eur J Cancer Clin Oncol 1990;8:141-5.
13. Bierman P, Giglio P. Diagnosis and treatment of central nervous system involvement in non-Hodgkin’s lymphoma. Hematol Oncol Clin North Am 2005;19:597-609, v.
14. Ness GO, Lybaek H, Arnes J, Rødahl E. Chromosomal imbalances in lymphoid tumors of the orbit. Invest Ophthalmol Vis Sci 2002;43:9-14.
15. Madge SN, McCormick A, Patel I, et al. Ocular adnexal diffuse large B-cell lymphoma: local disease correlates with better outcomes. Eye (Lond). 2009 Nov 27.
16. Jenkins C, Rose GE, Bunce C, et al. Clinical features associated with survival of patients with lymphoma of ocular adnexa. Eye 2003;17:809-20. | |
|
 |
 |
 |

|
|
 Welcome, please sign in
Welcome, please sign in  Welcome, please sign in
Welcome, please sign in